CHAPTER 45 Pectoral girdle and upper limb: overview and surface anatomy
This chapter is divided into two sections. The first is an overview of the general organization of the upper limb, with particular emphasis on the distribution of the major blood vessels and lymphatic channels, and of the branches of the brachial plexus: it is intended to complement the detailed regional anatomy described in Chapters 46 to 50 Chapter 47 Chapter 48 Chapter 49 Chapter 50. The second section describes the surface anatomy of the upper limb.
BONES AND JOINTS
The bones of the upper limb are the clavicle, scapula, humerus, radius and ulna (connected for a large portion of their length by an interosseous membrane) and the bones of the hand, i.e. the carpals, metacarpals and phalanges (Figs 45.1, 45.2).
The shoulder girdle is extremely mobile because reciprocal movements at the sternoclavicular and glenohumeral joints enable 180° abduction of the upper limb. Movement occurs in all three planes at the glenohumeral joint.
MUSCLES
The extensor muscles of the wrist and fingers, together with brachioradialis and a slip of origin of supinator, arise from the lateral epicondyle of the humerus. The principal head of pronator teres, the carpal flexor muscles, palmaris longus and, at a deeper level, the main origin of flexor digitorum superficialis, all arise from the medial epicondyle of the humerus. More deeply, flexor pollicis longus, flexor digitorum profundus and pronator quadratus arise from the anterior aspects of the shafts of the radius and ulna and the intervening interosseous membrane. Abductor pollicis longus, extensors pollicis longus and brevis and extensor indicis all arise from the posterior aspects of these bones and the intervening interosseous membrane.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
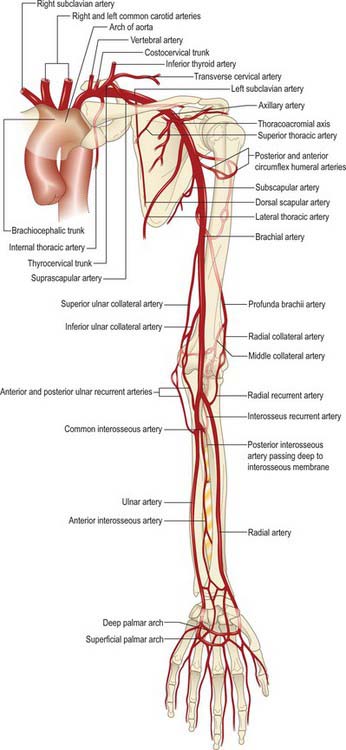
ARTERIAL SUPPLY
The blood supply to the skin of the upper limb comes from a combination of direct cutaneous, fasciocutaneous and musculocutaneous vessels (Figs 45.3, 45.4; see Fig. 7.19).

Fig. 45.4 The anatomical territories served by the cutaneous blood supply to the upper limb.
(From Cormack GC, Lamberty BGH 1994 The Arterial Anatomy of Skin Flaps, 2nd edn. Edinburgh: Churchill Livingstone, with permission.)
VENOUS DRAINAGE
The venous drainage of the upper limb is composed of superficial and deep groups of vessels.
The superficial group starts as an irregular dorsal arch on the back of the hand. The cephalic vein begins at the radial extremity of the arch, ascends along the lateral aspect of the arm within the superficial fascia and then pierces the deep fascia to enter the axillary vein just distal to the clavicle (Fig. 45.5). The basilic vein drains the ulnar end of the arch, passes along the medial aspect of the forearm, pierces the deep fascia at the elbow and joins the venae comitantes of the brachial artery to form the axillary vein. In front of the elbow, the prominent median cubital vein links the cephalic and basilic veins. It receives a number of tributaries from the front of the forearm and gives off the deep median vein which pierces the fascial roof of the antecubital fossa to join the venae comitantes of the brachial artery.
LYMPH NODES AND DRAINAGE
Superficial tissues
In the forearm and arm, superficial vessels run with the superficial veins. Collecting vessels from the hand pass into the forearm on all carpal aspects. Dorsal vessels, after running proximally in parallel, curve successively round the borders of the limb to join the ventral vessels. Anterior carpal vessels run through the forearm parallel with the median vein of the forearm to the cubital region, then follow the medial border of biceps brachii before piercing the deep fascia at the anterior axillary fold to end in the lateral axillary lymph nodes (Fig. 45.6).
Lymphatic drainage of deep tissues
Deep lymph vessels follow the main neurovascular bundles (radial, ulnar, interosseous and brachial) to the lateral axillary nodes. They are less numerous than the superficial vessels and communicate with them at intervals. A few lymph nodes occur along the vessels. Scapular muscles drain mainly to the subscapular axillary nodes, and pectoral muscles drain mainly to the pectoral, central and apical nodes (Fig. 45.6).
INNERVATION
OVERVIEW OF THE BRACHIAL PLEXUS
The brachial plexus is formed by the union of the ventral rami of the lower four cervical nerves and the greater part of the first thoracic ventral ramus (Fig. 45.7; see Fig. 46.29).

Fig. 45.7 A schematic plan of the left brachial plexus.
(Adapted from Drake, Vogl and Mitchell 2005.)
The fourth ramus usually gives a branch to the fifth, and the first thoracic ramus frequently receives a branch from the second. These ventral rami are the roots of the plexus: they are almost equal in size but variable in their mode of junction. Contributions to the plexus by C4 and T2 vary. When the branch from C4 is large, that from T2 is frequently absent and the branch from T1 is reduced, forming a ‘prefixed’ type of plexus. If the branch from C4 is small or absent, the contribution from C5 is reduced but that from T1 is larger and there is always a contribution from T2: this arrangement constitutes a ‘postfixed’ type of plexus.
Axillary nerve (C5, 6)
The axillary nerve is a branch of the posterior cord of the brachial plexus. It winds posteriorly around the neck of the humerus together with the circumflex humeral vessels, and supplies deltoid and teres minor and an area of skin over the deltoid region (Fig. 45.8).
Radial nerve (C5–8, T1)
The radial nerve is the continuation of the posterior cord of the brachial plexus (Fig. 45.9). In the upper arm it lies in the spiral groove of the humerus where it is accompanied by the profunda brachii artery and its venal comitantes. It enters the posterior (extensor) compartment and supplies triceps, then re-enters the anterior compartment of the arm by piercing the lateral intermuscular septum. At the level of the lateral epicondyle it gives off the posterior interosseous nerve, which passes between the two heads of supinator and enters the extensor compartment of the forearm. The posterior interosseous nerve supplies these muscles, while the radial nerve proper continues into the forearm in the anterior compartment deep to brachioradialis and terminates by supplying the skin over the posterior aspect of the thumb, index, middle and radial half of the ring finger.
Musculocutaneous nerve (C5–7)
The musculocutaneous nerve is formed from the continuation of the lateral cord of the brachial plexus. It pierces and supplies coracobrachialis, biceps and brachialis, and then continues into the forearm as the lateral cutaneous nerve of the forearm (Fig. 45.10).
Median nerve (C6–8, T1)
The median nerve is formed by the union of the terminal branch of the lateral and medial cords of the brachial plexus (Fig. 45.11). It has no branches in the upper arm. It enters the forearm between the two heads of pronator teres and gives off the anterior interosseous nerve, which supplies all the flexor muscles of the forearm apart from flexor carpi ulnaris and the ulnar half of flexor digitorum profundus. The median nerve itself passes deep to the flexor retinaculum at the wrist. On entering the palm, it gives off motor branches to the thenar muscles and the radial two lumbricals, and cutaneous branches to the palmar aspect of the thumb, index and middle fingers and the radial half of the ring finger.
Ulnar nerve (C7, C8, T1)
The ulnar nerve is the continuation of the medial cord of the brachial plexus (Fig. 45.12). Like the median nerve, it has no branches in the upper arm. It enters the posterior compartment of the upper arm midway down its length by piercing the medial intermuscular septum, passes behind the medial epicondyle of the humerus to enter the forearm and descends to the wrist deep to flexor carpi ulnaris. The ulnar nerve supplies flexor carpi ulnaris and the ulnar half of flexor digitorum profundus. Just proximal to the wrist it gives off a dorsal cutaneous branch that supplies the skin over the dorsal aspect of the little finger and the ulnar half of the ring finger, and then crosses into the palm superficial to the flexor retinaculum in Guyon’s canal. It divides into a motor branch, which supplies the hypothenar muscles, the intrinsic muscles of the hand (apart from the radial two lumbricals) and adductor pollicis, and cutaneous branches, which supply the skin of the palmar aspect of the little finger and the ulnar half of the ring finger.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree