Ophthalmic Surgery
Eileen Mielcarek
Eyesight is not essential to life, but quality of vision enables us to have a higher quality of life. Much of what we learn throughout our lifetime and how we understand and navigate our world is through our vision. In 2012 Bausch + Lomb surveyed more than 11,000 people in 11 countries to gauge eye care habits and perceptions. Their survey, the Barometer of Global Eye Health, revealed that respondents said they would rather lose a limb, lose 10 years of their life, or receive a 50% cut in income rather than lose 50% of their vision (Bausch + Lomb, 2012). Early detection of eye disease through regular eye examinations can provide the most effective treatment when needed and ultimately preserve vision.
There is a disconnect between Americans’ fear of losing their vision and not taking the necessary steps to preserve and enhance their eyesight. The previously mentioned survey revealed that more than two thirds of respondents did not have a recent eye examination—the most basic step necessary to preserve eyesight. In addition, 7 in 10 consumers said they were somewhat or very knowledgeable about their eye healthcare, yet 97% of eye doctors say the public does not sufficiently understand proper eye healthcare. Part of the disconnect could be attributed to the fact that sick or diseased eyes often look normal and certain diseases exhibit no warning signs (Bausch + Lomb, 2012).
The ocular surgical interventions discussed in this chapter are delicate, are microscopic, and demand careful planning and execution by both the surgeon and the perioperative staff. As technology advances in eye care, surgical interventions become more detailed and require advanced instrumentation as well as more planning and participation. Emerging technology requires a partnership with high-tech computers and precise instrumentation. The perioperative nurse must keep abreast of changes in technology, procedural techniques, safety issues, efficiency, communication, and patient education resources to provide optimal care to ophthalmic surgery patients.
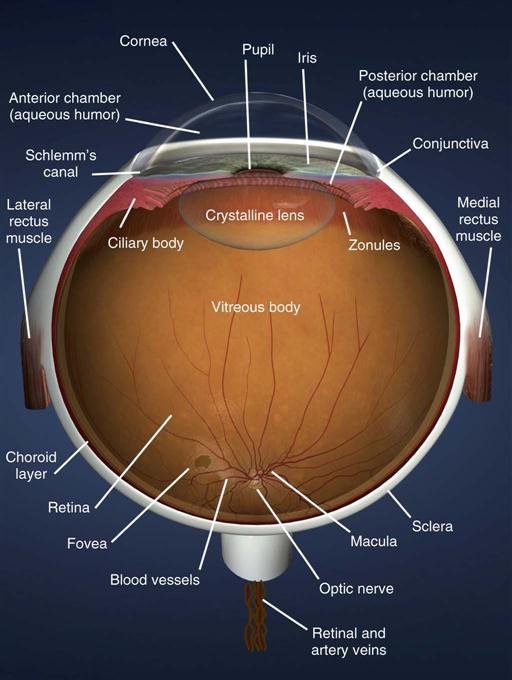
Surgical Anatomy
The eyes are one of the more complex organs of the human body. Vision begins with a focal point of light, which travels through the cornea, lens, and vitreous fluid, and lands on the retina to be sent to and interpreted by the brain. Clear vision requires all of the following: healthy, functioning eye structures; adequate light; intact neurovascular communication with the brain; and the brain’s effective interpretation of the images relayed. The following cycle, if completed in the full sequence, leads to accurate visual images.
2. Iris muscles control the size of the pupil to allow the appropriate amount of light into the eyes.
4. The rays travel through the clear vitreous fluid and land directly on the macula, the central part of the retina and the area of highest sensitivity for details. The nerve endings of the retina pass the images as nerve impulses through the optic nerve to the brain, where the occipital area interprets the images (Figure 18-1).
The American Academy of Ophthalmology (AAO) recommends that healthy adults receive an eye examination every 2 years, even if vision is normal and unchanged. Children should receive a baseline eye examination by an ophthalmologist prior to starting school, even if no signs of impairment or complications are presented. Diabetic individuals of any age should see an ophthalmologist every year because they are at higher risk for eye diseases (AAO, 2012).
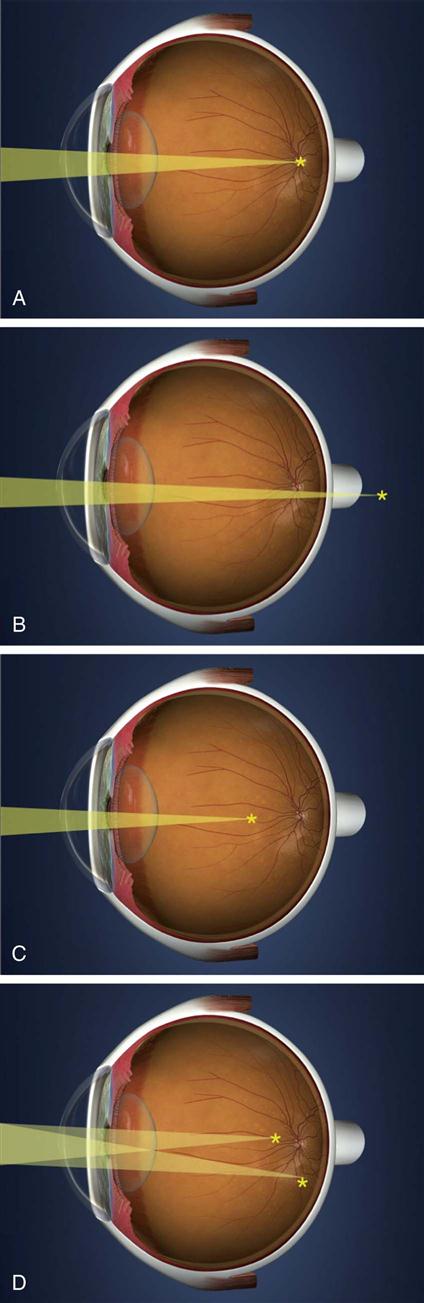
Refractive Apparatus
As light rays pass through the eye, there are opportunities for the light not to land directly on the macula. Refractive errors occur when images do not focus and fall directly on the retina, but these can be corrected with eyeglasses or contact lenses. Myopia (e.g., nearsightedness) occurs when the focal point of the light rays is behind the retina. Hyperopia (e.g., farsightedness) occurs when the light rays focus in front of the retina. Astigmatism occurs when the cornea is cylindrically shaped instead of spherical, and the light rays diverge as they reach the retina. Presbyopia is the natural aging of the eye in which the lens cannot change shape and accommodate for the focusing needed to see close objects. Myopia, hyperopia, and astigmatism are considered lower-order aberrations that account for the majority of refractive errors. Higher-order aberrations are complex microscopic irregularities presented on the surface of the cornea, lens, and retina that can affect the quality of visual acuity.
Eyeglasses that minimize images are prescribed to refocus light rays in myopic patients; eyeglasses that magnify images are prescribed for hyperopic patients; and magnifying bifocals or reading glasses are prescribed for presbyopic patients, usually after age 40. Presbyopia occurs in everyone older than age 45, even if they have perfect distance vision. The unit of measure in refraction is called a diopter. The more diopters required to correct vision, the worse unaided vision one has (Figure 18-2).
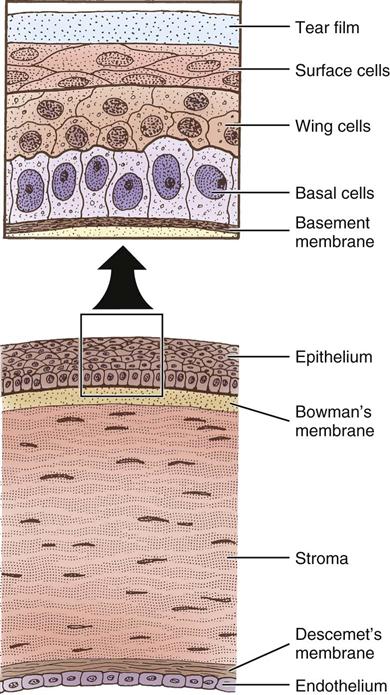
Cornea
The cornea is the transparent, avascular window through which light passes to the retina; it joins the white sclera at a transitional zone called the limbus. The cornea is composed of five layers: the epithelium, Bowman’s membrane, the stroma, Descemet’s membrane, and the endothelium. The epithelium consists of constantly renewing cell layers with many nerve endings, accounting for the cornea’s great sensitivity to foreign bodies and abrasions. Bowman’s membrane is connective tissue thickening that forms a barrier to trauma and infection under the epithelium. If damaged, Bowman’s membrane does not regenerate and a permanent scar is formed. The stroma accounts for 90% of the corneal thickness and is composed of precisely layered fibers. If this layering is disrupted (for example, by edema), the corneal clarity decreases. Descemet membrane is a thin layer between the endothelial layer of the cornea and the stroma. The corneal endothelium is a single layer of hexagonal cells that acts as a fluid pump to keep the cornea clear by maintaining the proper level of stromal dehydration for clarity. Because corneal endothelial cells do not regenerate, damage to this layer may cause persistent corneal edema and loss of transparency (Figure 18-3).
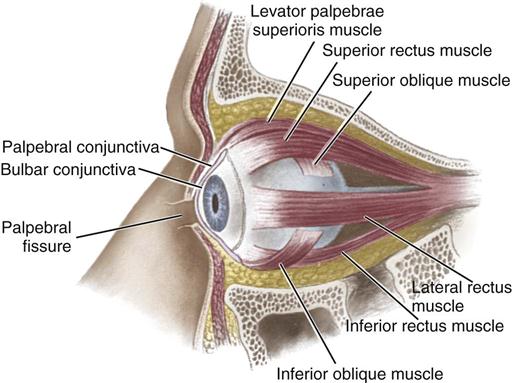
The sclera is the opaque “white” part of the strong external layer, and is made up of collagenous fibers loosely connected with fascia. The sclera receives the attachments of the extraocular muscle tendons, and is pierced by the ciliary arteries and nerves posteriorly by the optic nerve. The sclera provides the eye with form and shape and encompasses the entire side and back of the eye.
Conjunctiva
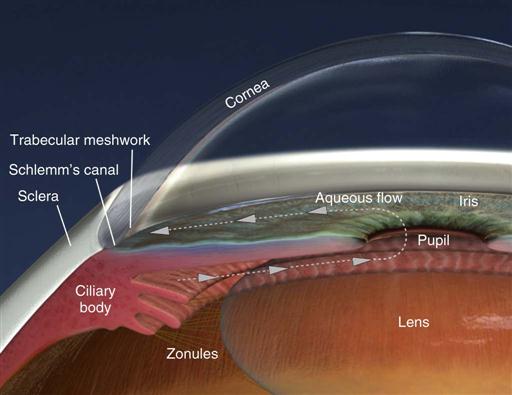
The conjunctiva is a thin, transparent mucous membrane divided into a palpebral portion (lining the inside of the eyelids) and a bulbar portion (lining the surface of the globe). The junction between the palpebral and bulbar conjunctivae forms a forniceal sac (Figure 18-4).
Crystalline Lens
The biconvex lens is suspended behind the iris and connected to the ciliary body by delicate collagenous strings called zonules. The lens changes shape and focus (accommodation) by either relaxation or tightening of the zonular fibers. Over time (particularly after age 40), the lens and lens zonules becomes progressively less elastic, resulting in presbyopia. This loss of accommodative power is typically corrected by reading glasses or bifocals.
Vitreous Humor
The vitreous body is a transparent, gelatinous mass composed of 99% water and 1% collagen and hyaluronic acid. It fills the posterior four fifths of the eyeball and is adherent to the retina at the vitreous base. The vitreous supports the shape of the eye internally and gives the eye its shape.
Retina
The retina is an extension and modification of the brain designed to perceive light and relay visual signals through the optic nerve back to the occipital brain. The central portion of the retina is called the macula and is responsible for central detailed vision (20/20), while the peripheral retina is responsible for spatial orientation, night vision, and peripheral vision. The visual sensory nerve endings of the retina pass the images as nerve impulses through nerve fibers of the optic nerve to the brain, where the occipital area interprets the images.
Supporting Structures
Nerve and Blood Supply
The optic nerve (second cranial nerve) extends between the posterior eyeball and the optic chiasm. This cranial nerve carries visual impulses as well as the sensations of pain, touch, and temperature from the eye and its surrounding structures to the brain, where it can be interpreted. The ophthalmic artery, the main arterial supply to the orbit and globe, is a branch of the internal carotid artery. It divides into branches supplying the globe, muscles, and eyelids. The central retinal artery and central retinal vein travel through the optic nerve and provide a separate blood supply for the retina.
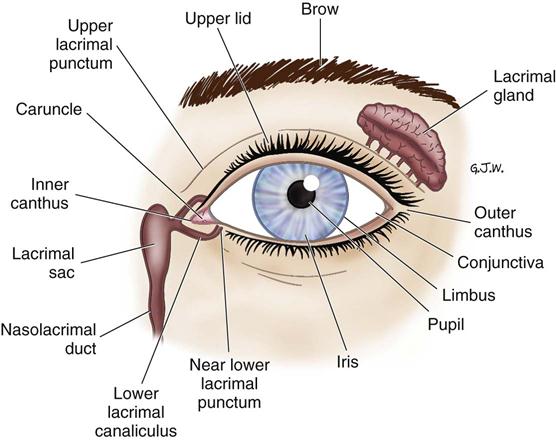
Lacrimal Apparatus
The lacrimal gland produces aqueous tears and secretes them through a series of ducts onto the anterior ocular surface, thereby keeping the cornea moist and washing away any debris. The tears then flow inward to the puncta, from which they are conducted by the canaliculi to the lacrimal sac and finally pass into the nasolacrimal duct. The lacrimal apparatus effectively functions like a sink, with a faucet (main and accessory lacrimal glands) and drain (lacrimal puncta, canaliculi, sac, and nasolacrimal duct) (Figure 18-5).
Eyelid
Eyelids provide protection to the eye from debris and foreign bodies, as well as provide continuous tear moisture to the cornea (blinking). The anterior eyelid layers contain the eyelid skin, ocular adnexa (eyelashes and associated glands), and subcutaneous tissue, lymphatics, and muscles. The tarsus is a plate of dense fibrous tissue that forms the main scaffolding of the eyelids. Within the tarsus are the meibomian glands, which secrete the oily component (sebum) of the tear film. The orifices of these sebaceous glands are found at the eyelid margin just posterior to the eyelashes.
The palpebral fissure refers to the space between the margins of the two eyelids. When the eye is closed, the fissure becomes a mere slit and the cornea is completely covered by the upper eyelid. The upper eyelid is more mobile and larger than the lower. The eyelids are closed by the orbicularis oculi muscle, and the upper lid is opened by the levator muscle.
Tears
Tears are essential for keeping the cornea lubricated to maintain clarity and optical performance. Tears have three layers; the mucous layer that sits closest to the cornea, the aqueous water layer, and the oily lipid layer. Aqueous tears are created by the lacrimal glands located within the upper temporal eyelid, mucous layer by conjunctival cells, and oily layer by meibomian glands in the eyelid. The cornea does not have blood vessels or blood flow, so tears provide antibodies and nutrition to the cornea, as well as flush out irritations and debris.
Muscles
Seven separate eye muscles control the movement of the eyeball. The muscles work in yoked pairs, with ocular movements generated by an increase in the tone of one set of muscles and a decrease in the tone of the antagonistic muscles. Named according to their relative position on the eyeball, the extraocular muscles of the eyeball include the four recti (the superior rectus, inferior rectus, medial rectus, and lateral rectus) and two oblique muscles (the superior oblique and inferior oblique). Except for the inferior oblique muscle, these muscles originate from the back of the orbit. The extraocular muscles are supplied by cranial nerves III (oculomotor, supplying the superior, inferior, and medial recti), IV (trochlear, supplying the superior oblique), and VI (abducens, supplying the lateral rectus) (Figure 18-6).
Perioperative Nursing Considerations
Assessment
Patients undergoing eye surgery range from premature infants with retinopathy of prematurity or congenital conditions to elderly patients whose conditions result from the aging process. These patients need assessment of both their vision and general health status. A preoperative visit to the eye clinic or surgeon’s office typically completes the diagnostic testing and physical examination pertinent to the presenting eye condition subsequently requiring surgery. Communication with the physician’s office staff to coordinate patient preparation and teaching and to collate preoperative test results increases the efficiency and effectiveness of preoperative procedures. Perioperative nurses contact patients preoperatively by phone to provide needed information concerning the day of surgery and to obtain initial preoperative assessment information.
The perioperative nursing staff must be prepared to meet the specific needs of each patient and family, collaborate and communicate effectively for continuity of patient care, and prepare the patient for home care. On admission, a staff member should fully orient the patient to the physical surroundings. Constant description and reinforcement are important to visually impaired patients. Approaching the patient from the unaffected side increases the patient’s independence and decreases the possibility of startling the patient.
The assessment is designed to collect and disseminate pertinent information and must be carried out in a comprehensive, yet efficient, manner. A standard set of parameters should provide enough information to facilitate appropriate care in the event of an emergency. Physiologic information (e.g., height, weight, vital signs), psychosocial factors (e.g., support systems, fears, anxiety), and environmental, education, and self-care needs are assessed. The general health history includes completing a comprehensive list of current medication therapy (often the patient is asked to bring currently prescribed medications to the appointment). The medical history is very important in cueing the nurse to evaluate for ocular manifestations of systemic disease. For example, the patient may present for retinal surgery as a consequence of retinopathy related to diabetes mellitus. Additional discharge planning factors are also explored.
Data may be collected from family or significant others or directly from physicians or their office staff. Throughout the assessment process the nurse encourages the patient toward self-actualization and assuming an active role in his or her healthcare needs. All information should be documented so that it is readily available to others.
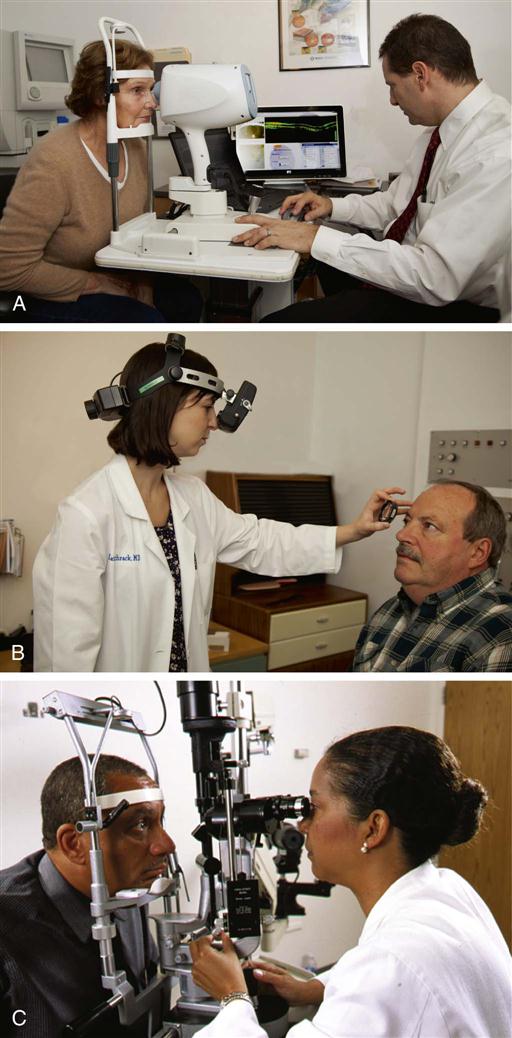
An ocular history, which includes the patient’s primary problem, history of the present condition, symptoms, and visual limitations, is collected from the patient’s initial visit to the eye care provider’s office, and the nurse confirms these findings. Some common forms of ocular examination are shown in Figure 18-7.
An external examination of the eye, including lids, lashes, conjunctivae, and lacrimal apparatus, should have been performed to detect any deviations from normal. The corneal reflex should have been tested and the cornea inspected for superficial irregularities. Pupil size and contour, as well as pupillary reaction, both direct and consensual, should be noted. Shallow anterior chamber depth alerts staff members to the potential for high pressures resulting from angle closure with dilation of the pupil.
The function of the extraocular muscles should have been determined. Movement should be synchronous, and visual lines should meet on a fixed object. Documentation of this examination must be descriptive, accurate, and concise. It is of value later in assessing the outcome of the procedure. The following observations are also important:
• Symptoms of irritation (itching, burning)
• Position of eyelids (opened and closed), condition of upper and lower lid surfaces, eyelid spasm
• Current medication history, including anticoagulants, analgesics, herbs, and nutritional supplements
After the assessment information has been compiled, nursing diagnoses are identified and the plan of care for the entire perioperative period is developed.
Nursing Diagnosis
Nursing diagnoses related to the care of patients undergoing ophthalmic surgery might include the following:
Outcome Identification
Outcomes identified for the selected nursing diagnoses could be stated as follows:
Planning
Plans of care are the framework for organizing activities in the perioperative period. Although ophthalmic surgery is often perceived as minor because of the small incision site and relatively short surgery period, the perioperative nurse must be fully prepared for potential complications or emergencies. Patients who are admitted for ophthalmic surgery often have complex medical histories. After a review of the patient’s record, supplemented by a patient or family interview or collaboration with colleagues, the data collected are incorporated into an individualized perioperative plan of care. A Sample Plan of Care for a patient undergoing ophthalmic surgery can be found on page 586.
Implementation
Managing and Monitoring Patient Safety Needs.
A key aspect of the perioperative nurse’s role is patient safety. Because many ophthalmic procedures are performed with local anesthesia, the circulating nurse or an additional perioperative nurse must be prepared to monitor the patient and provide supportive care. Reassurance is especially important for patients who are awake because they can usually see and hear the surgery progressing. Ophthalmic patients, like other surgical patients, have increased sensitivity to noise and activities within the operating room (OR). The OR should be kept quiet and peaceful to decrease anxiety and increase cooperation, thereby reducing the need for deep sedation.
Both the scrub person, who may be a registered nurse or surgical technologist, and the perioperative nurse, must also manage additional patient safety needs. Foreign substances must not be introduced intraocularly. Lint-free drapes should be used to create the sterile field. Gloved hands should not touch the portion of an instrument used in an intraocular wound, and debris should be cleansed from instruments with cellulose sponges.
Members of the perioperative team have several important responsibilities in the preparation of the room and the equipment. Technologic advances in ophthalmic surgery require that perioperative nurses be familiar with equipment and check each piece carefully before the patient arrives in the OR. Organization and grouping of the outlet cords must be checked to ensure clear walking areas. The availability of specially ordered intraocular lens implants or prostheses needs to be checked to prevent delay or cancellation of the procedure. Scrupulous attention to aseptic technique is essential in preventing endophthalmitis (infection within the eye) and possible blindness. Safety-focused communication within the perioperative nursing team includes the following:
• Verifications: The patient or family member should also state which eye is the operative site and which procedure is being performed. The nurse reviews the surgical consent, surgeon’s preoperative orders, and OR schedule to determine if the correct operative eye has been prepared (including verification of operative eye using the word “right” or “left” [abbreviations are not accepted], marking of operative site, and dilation, if appropriate) and other procedures have been carried out according to facility policies on correct-site surgery. Such a policy may require that before the administration of eyedrops or medication, the nurse asks the awake patient which eye is the operative site. If there is any discrepancy among the patient’s response, the informed consent, the physician’s orders, ophthalmic history, and exam, the discrepancy is corrected during the preoperative verification process. Immediately before the incision, this information, along with any implants or special needs, is reconfirmed during the time-out (Patient Safety).