Neurogenic Sarcoma (Malignant Peripheral Nerve Sheath Tumor)
Key Facts
Clinical Issues
Extremely rare tumor
Often associated with neurofibromatosis
Tumors may be central or peripheral
Tumors may arise in endobronchial location
Aggressive behavior with recurrences and metastases
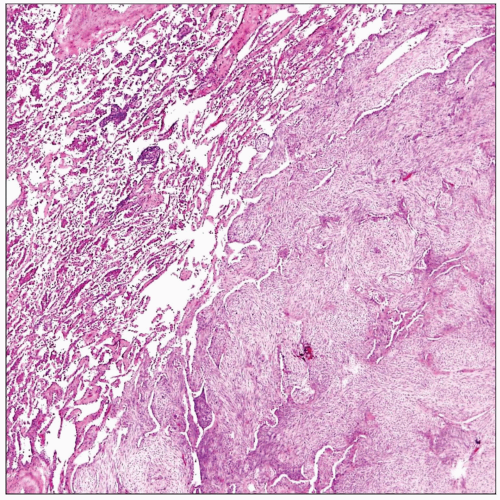
Microscopic Pathology
Fascicular atypical spindle cell proliferation
Frequent “herringbone” pattern of growth
Alternating hyper- and hypocellular areas
Rhabdomyoblastic differentiation may be present (malignant “triton” tumor)
Frequent areas of cystic degeneration, hemorrhage, and necrosis
Prominent myxoid stromal changes
Ancillary Tests
S100 protein is of limited utility for diagnosis because expression is lost or only focal in malignant neural neoplasms
Immunohistochemical staining has very low specificity for diagnosis of neurogenic sarcoma
Shows complex interdigitating cytoplasmic processes covered by basal lamina material on EM
Diagnostic Checklist
Immunohistochemical staining may be of very limited value for diagnosis in neurogenic sarcoma
2 most reliable features for establishing diagnosis are a history of neurofibromatosis and ultrastructural findings
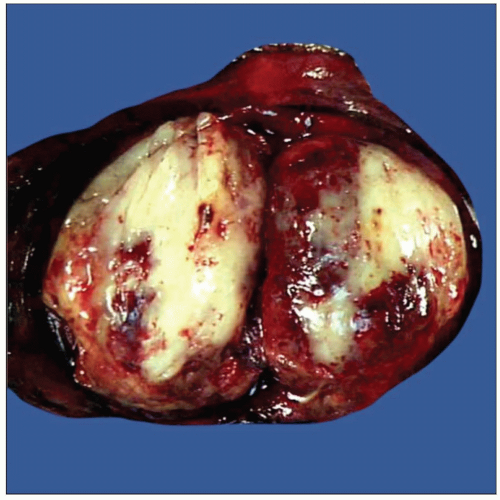 Gross appearance of primary neurogenic sarcoma of the lung in a resected specimen shows a fleshy, well-circumscribed tumor mass with extensive areas of hemorrhage and a glistening cut surface. |
TERMINOLOGY
Synonyms
Malignant peripheral nerve sheath tumor
Malignant schwannoma
Definitions
Primary malignant lung neoplasm showing evidence of peripheral nerve sheath differentiation
CLINICAL ISSUES
Epidemiology
Incidence
Extremely rare tumor
Often associated with neurofibromatosis
Age
Affects all age groups
Most frequent in young adults and middle-aged patients (30-50 years of age)
Gender
No sex predilection
Presentation
Large intraparenchymatous mass
Tumors may be central or peripheral
Tumors may arise in endobronchial location
Shortness of breath
Cough
Chest pain
Small peripheral tumors may be asymptomatic and discovered incidentally
Treatment
Surgical approaches
Surgical excision
Adjuvant therapy
Chemotherapy and radiation therapy may be employed for advanced or unresectable cases
Prognosis
Aggressive behavior with recurrences and metastases
Usually rapidly progressive course with fatal outcome
MACROSCOPIC FEATURES
General Features
Large, fleshy, gray-white, lobulated tumor
May be partially encapsulated
Frequent hemorrhage and necrosis
Sections to Be Submitted
Submit at least 1 section per centimeter of largest tumor diameter
Size
Usually large (> 5 cm in greatest dimension)
MICROSCOPIC PATHOLOGY
Histologic Features
Fascicular atypical spindle cell proliferation
Frequent “herringbone” pattern of growth
Alternating hyper- and hypocellular areas
Well-developed storiform pattern can be sometimes observed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree