■ Advantages of CT imaging for the evaluation of incisional hernias are multifactorial: accurate diagnosis in cases of obscure or small defects; proper identification of hernia contents (small bowel, colon, solid organs, omentum, etc.); definition of defect size; location of previously placed mesh; distinction from other or concomitant potential diagnoses (seroma, abscess, hematoma, etc.); identification of bowel incarceration; obstruction or possible ischemia, necrosis, or perforation; and planning of where to enter the abdomen safely.
■ When feasible, it is helpful for the operating surgeon to review the actual CT images, as the information discussed earlier may not be included in a radiologist’s reading of the films. It is also helpful to have CT images available to be viewed intraoperatively as they can serve as a reference during the operative procedure.
■ Colon cancer screening with colonoscopy or other appropriate means is often considered for those patients who have reached appropriate age for screening, have a significant family history, or other colonic symptoms prior to hernia repair.
SURGICAL MANAGEMENT
Preoperative Planning
■ For elective procedures, in the weeks leading up to repair, attempts should be made at optimization of preoperative patient factors associated with increased risk of postoperative wound complications: smoking cessation, evaluation and maximization of nutrition status, tight blood glucose control, weight loss in the obese, or elimination of open wounds through local wound care.8
■ Appropriate intravenous antibiotic prophylaxis should be administered prior to incision and repeated as needed to provide adequate prophylactic coverage depending on length of procedure and drug half-life.9
■ Venous thromboembolism prophylaxis should be provided, such as lower extremity serial compression devices or subcutaneous prophylactic dose heparin prior to induction of anesthesia, assuming no contraindications.9
■ Following induction of anesthesia, the abdominal wall is reexamined to confirm the borders of the defect in question and to identify the presence or location of previous mesh, signs of infection, or other issues.
■ Intraoperative urinary and gastric decompression are recommended.
■ Iodophor-impregnated adhesive skin drape may be used to minimize mesh contact with skin surfaces and therefore reduce the risk of mesh infection, although this has not been proven in randomized clinical trials.
Positioning
■ The patient should be positioned supine with arms adducted and tucked at sides of body with adequate padding of pressure points to avoid neurologic pressure injury. This allows movement of the surgeon and the assistant on each side of the table during the operation (FIG 2).
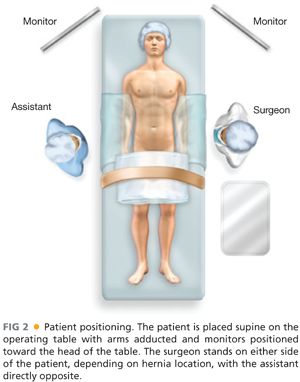
■ Semilateral or lateral decubitus position may be favored for repair of flank or lumbar hernias.
■ The patient should be secured to the operating table to allow steep positioning or rolling of the table as required during the procedure.
■ Laparoscopic monitors should be positioned over the working space to allow direct vision by both the primary surgeon and assistant.
TECHNIQUES
INITIAL ACCESS
■ A safe window of intraperitoneal access is usually available in areas distant from site(s) of previous surgery, although an open, “cut-down” technique can be performed near or within a hernia if the surgeon prefers.
■ Often, safe entry is found just inferior to the tip of the 11th rib, between midclavicular and anterior axillary lines (FIG 3).
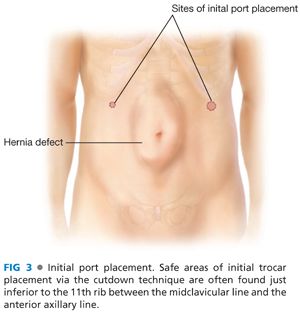
■ Open cut-down technique is most often performed with identification of individual abdominal wall layers as each is entered, but some surgeons use a port that allows visualization of the abdominal wall layers with the laparoscope as the trocar is slowly advanced into the abdomen.
■ Pneumoperitoneum is established at 12 to 15 mmHg.
PLACEMENT OF WORKING PORTS
■ Using an angled (30- or 45-degree) scope, a brief general inspection of the abdominal cavity checking for organ injury, which may have occurred during initial access, is performed.
■ Working port placement is based on target defect location, optimization of working space, and triangulation of working instruments, if possible. Ports that are too far caudal or cephalad may limit freedom of motion of the port due to the hip or rib cage (FIG 4).
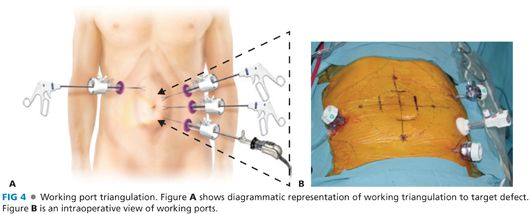
■ Ideal port placement allows sufficient working space between ports and target defect. The distance between individual ports should allow a range of motion that prevents ports from colliding or limiting motion. Ports should not be too close to the hernia defect as this limits visualization for mesh placement or mesh fixation.
■ Additional 5-mm trocars are placed under direct visualization (FIG 5).
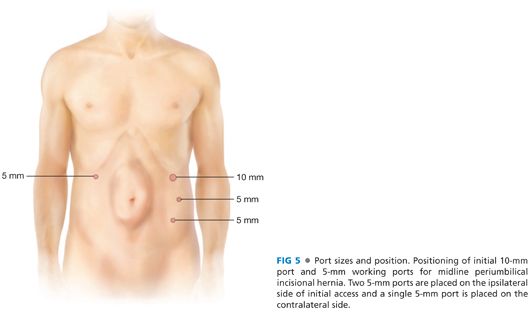
■ Often, two 5-mm trocars are placed laterally on same side as initial access port, usually between anterior and midaxillary lines.
■ One or two 5-mm trocars can be placed on the contralateral side of initial access port for adhesiolysis or to facilitate mesh fixation.
LYSIS OF ADHESIONS AND DEFINITION OF HERNIA DEFECT
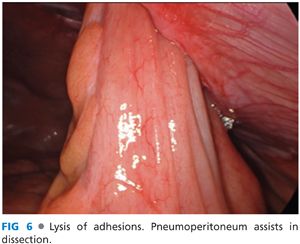
■ Pneumoperitoneum assists in dissection as countertraction is provided by weight of dependent omentum and bowel to expose safe tissues planes (FIG 6).
■ Meticulous lysis of adhesions is performed using sharp dissection with minimal judicious electrocautery to avoid thermal spread and bowel injury (FIG 7).
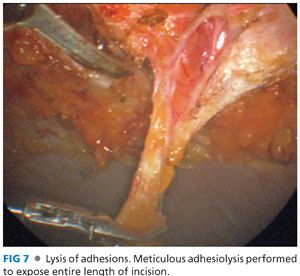
■ The majority of operative time is often spent performing the adhesiolysis. An enterotomy can increase the risk of mesh infection and, in cases of gross spillage, placement of prosthetic mesh is contraindicated. A bowel injury may result in the need for conversion to an open procedure, may necessitate the use biologic mesh or hernia closure without mesh, or the need for staged repair.
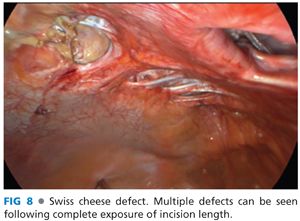
■ Freeing the adhesions along the entire length of incision often allows the surgeons to identify all defects (“Swiss cheese” or buttonhole abdominal wall defects), which otherwise may have gone unnoticed and therefore unrepaired (FIG 8).
■ Hernia contents can be reduced by applying gentle traction using nontraumatic graspers.
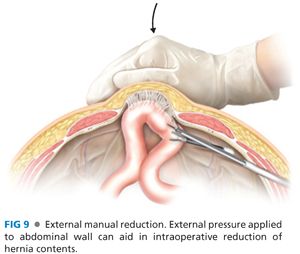
■ Simultaneous external manual compression of the hernia sac is helpful in reducing contents (FIG 9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


