Carcinoma Ex-Pleomorphic Adenoma
Lester D. R. Thompson, MD
Key Facts
Terminology
Presence of carcinoma arising from pleomorphic adenoma
Clinical Issues
Usually 6th to 7th decades, about 10 years older than PA
Parotid > > minor salivary glands
Long clinical history of painless mass with recent rapid enlargement and nerve palsy
Complete surgical resection
Local recurrence is common (up to 50%)
Local or distant metastases are common (up to 70%)
Poor overall survival
Prognostically significant factors include grade, stage, proportion of carcinoma, extent of invasion
Microscopic Pathology
Carcinoma may be specific tumor type
Carcinoma shows significant pleomorphism, increased mitoses, necrosis, destructive growth
Relative proportions of carcinoma and adenoma vary widely
Separated into low and high grade
PA is very frequently extensively hyalinized (fibrotic, scarred)
Reporting Considerations
Must report extent of invasion
Noninvasive (encapsulated) carcinoma without evidence of capsular invasion
Minimally invasive (≤ 1.5 mm)
Invasive (> 1.5 mm)
TERMINOLOGY
Abbreviations
Carcinoma ex-pleomorphic adenoma (Ca ex-PA)
Synonyms
Carcinoma ex benign mixed tumor
Malignant mixed tumor
Definitions
Presence of carcinoma arising from pleomorphic adenoma (PA)
Requires concurrent pleomorphic adenoma histologically or history of pleomorphic adenoma at same site
Carcinoma can be any epithelial neoplasm
ETIOLOGY/PATHOGENESIS
Pathogenesis
There is malignant transformation of epithelial component
Areas of transition help to substantiate a continuum
CLINICAL ISSUES
Epidemiology
Incidence
Accounts for about 4% of all salivary tumors
12% of all salivary malignancies
7% of all pleomorphic adenomas
Age
Usually in 6th and 7th decades
About 10-12 years older than age at presentation of pleomorphic adenoma
Exceptional in children
Gender
Probably equal gender distribution
Site
Major salivary glands most often (80%)
Parotid (80%) > submandibular (18%) > > sublingual gland (< 2%)
May be due to large tumor size and increased recurrence rate for major gland location
Minor glands (20%)
Palate > > nasopharynx > nasal cavity > > larynx
Presentation
Long clinical history of pleomorphic adenoma
The greater the length of time with tumor, the higher the risk of malignant transformation
5 years: 1.6%; 15 years: 9.6%
Symptoms/mass present for up to 44 years
Need to have well-documented previous tumor in same anatomic site if there is no histologic evidence of benign PA
Some tumors are slow growing and asymptomatic, so long history of mass by itself is insufficient
May have had multiple surgeries
About 20% have had previous surgery
Usually, recent rapid enlargement
Nerve palsies are common (40%)
Majority are painless
Rare: Skin ulceration, soft tissue attachment, bone invasion
Treatment
Surgical approaches
Complete surgical eradication
Lymph node dissection often required (˜ 20%)
Some recommend neck dissection for all major gland tumors
Lymph node dissection may not be necessary for low-grade carcinomas or those with limited invasion
Radiation
Prognosis
Local recurrence can be seen (range of 25-50%)
Majority are seen within 5 years of diagnosis
Many patients experience more than 1 recurrence
Recurrence rates tend to be lower for minor salivary gland primaries
Higher percentage of patients die with disease if they have local recurrence
Local or distant metastases are common (range of 50-70%)
Local lymph node metastases: Up to 25%
May be higher if there was previous surgery
Distant sites: Lung, bone (spine), liver, brain, skin
Most common in patients with local recurrence
Poor overall survival
Majority die of disease (60%)
5-year survival (30%)
Prognostically significant factors (order of importance)
Grade
Low grade: Tend not to die of tumor
High grade: Majority die from tumor
Stage
Proportion of tumor that is carcinoma
Extent of invasion
Noninvasive (encapsulated): Excellent long-term outcome (identical to conventional PA)
Minimally invasive tumors (≤ 1.5 mm): Good outcome (75-85% at 5 years)
Widely invasive (> 1.5 mm): Poor outcome (25-65% at 5 years)
Large tumor size
Histologic subtype
Polymorphous low-grade adenocarcinoma: 96% 5-year survival
Salivary duct carcinoma: 62% 5-year survival
Myoepithelial carcinoma: 50% 5-year survival
Undifferentiated carcinoma: 30% 5-year survival
High proliferation index
Margin status
Positive margins predict higher recurrence rate and higher death rate from tumor
IMAGE FINDINGS
Radiographic Findings
Location, extent, and lymph node status can be established
Areas of benign PA may be identified
Areas of calcification more common in PA
Ill-defined margin or loss of sharp margin is often a clue to malignancy
Low T2 MR signal in solid mass is worrisome for malignancy
Perineural spread along CN VII in temporal bone
Facial nerve plane separating superficial and deep lobes of parotid may be lost
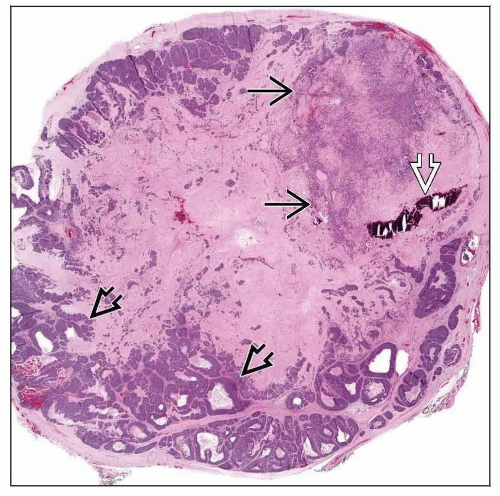
MACROSCOPIC FEATURES
General Features
Circumscribed and encapsulated tumors may be seen
Most tumors are poorly circumscribed with invasion easily identified
Area of circumscription may represent residual PA
Area of scarring may also represent residual PA
Necrosis and hemorrhage may be present
Benign areas: Translucent gray-blue
Carcinoma areas: Firm, white, tan or gray
Sections To Be Submitted
Must submit areas of transition between possible benign and malignant zones
Must submit from periphery to be able to measure extent of invasion
Size
Range: Up to 25 cm
Mean: About 5 cm
Average size is about 2x that of PA
MICROSCOPIC PATHOLOGY
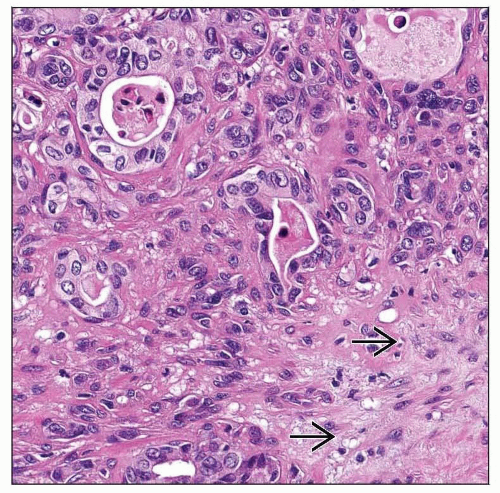
Histologic Features
Carcinomatous component may be part of specific tumor type
Adenocarcinoma, NOS, salivary duct carcinoma, adenoid cystic carcinoma, mucoepidermoid carcinoma, myoepithelial carcinoma, polymorphous low-grade adenocarcinoma, epithelial-myoepithelial carcinoma
Epithelial and myoepithelial components together
Epithelial component only
Carcinoma shows
Significant pleomorphism (enlarged pleomorphic cells with hyperchromatic nuclei, prominent nucleoli)
Increased mitotic figures
Areas of necrosis
Destructive growth
Relative proportions of carcinoma and adenoma vary widely
Malignant and benign juxtaposed
Malignant and benign blended
Sclerotic nodule in malignant tumor suggests residual PA
Multifocal, distinct and separate malignant nodules
Carcinoma ranges from focal to diffuse
In majority of cases, carcinoma represents > 50% of tumor volume
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree