Blood pressure is a measure of the pressure in the systemic cardiovascular system and is reported as central arterial pressure (i.e. equivalent to that in a large artery at the height of the heart). The higher value is the systolic blood pressure as the left ventricle contracts and ejects, and the lower value is the diastolic blood pressure when the heart is not contracting. In a healthy adult, normal values are 120 mmHg (systolic) and 80 mmHg (diastolic), and mean arterial pressure is reported as:
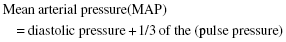
where pulse pressure is the difference between systolic pressure and diastolic pressure.
MAP in a healthy adult is approximately 93 mmHg. The mean arterial pressure is the time-averaged pressure experienced by the systemic circulation.
Blood pressure is determined by cardiac output (CO) × total peripheral resistance (TPR) and is tightly controlled to ensure appropriate tissue perfusion. Hypertension is pathological and is a sustained increase in blood pressure at rest, such that diastolic blood pressure is ≥90 mmHg and systolic is ≥140 mmHg. In the healthy adult, blood pressure is tightly regulated by nervous and hormonal mechanisms.
Nervous control of blood pressure and baroreceptor control
Blood pressure is regulated in the short term by the autonomic nervous system, with sympathetic innervation of arterial smooth muscle leading to α1-adrenoceptor-mediated vasoconstriction and an increase TPR (Chapter 31). To ensure maintenance of blood pressure, baroreceptors in the carotid sinus and aortic arch sense pressure, and as pressure increases there are increased impulses to the nucleus of the solitary tract (nucleus tractus solitarius; NTS) in the brain. Increases in pressure inhibit the ‘pressor’ area in the rostral ventrolateral medulla to reduce sympathetic output from the vasomotor centre. Increases in pressure also stimulate the ‘depressor’ area in the caudal ventrolateral medulla to inhibit sympathetic output from the vasomotor centre (Figure 32.1). This is accompanied by increased vagal output to lower blood pressure. Decreases in blood pressure lead to the ‘pressor’ centre dominating and decreased vagal output to restore blood pressure (Figure 32.2).
Postural control of blood pressure
Changes in posture lead to alterations in pressure due to the hydrostatic influence on the blood. For example, when changing from lying down to standing up, the change in fluid distribution would tend to cause a reduction in central blood pressure. The reduction in central arterial pressure would tend to lead to less pressure in the cerebral circulation and could lead to ‘light headedness’. However, the baroreceptor reflex aims to maintain a relatively constant blood pressure with any change in posture. An initial drop in blood pressure would initiate a baroreceptor reflex, resulting in increased sympathetic activity (with peripheral vasoconstriction) and decreased vagal activity to maintain a relatively constant blood pressure. Autonomic dysfunction or drug treatments that interfere with volume control (diuretics) or α1-adrenoceptor-mediated vasoconstriction (α1-adrenoceptor antagonists) can impair these responses and lead to postural or orthostatic hypotension (i.e. when systolic blood pressure drops >20 mmHg) when changing from lying or sitting down to standing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


