Ophthalmic Surgery
LEARNING OBJECTIVES
After studying this chapter the reader will be able to:
• Describe the anatomy of the eye
• Correlate physiology to conditions requiring surgical intervention
• Describe the risk factors associated with ophthalmic surgery
• Compare diagnostic methods for determination of surgical interventions
• Understand and explain ophthalmic surgical procedures
• Identify potential sources of surgical site infection
• List the pharmacologic and hemostatic agents utilized during ophthalmic surgery
• Explain the purpose and expected outcomes of ophthalmic surgical procedures
Overview
Statistics about vision loss are staggering: throughout the world, more than 161 million people have significant vision loss and that number is expected to double by 2020; more than 37 million people are completely blind, with someone going blind every 5 seconds. Ninety percent of eye accidents, thousands of which occur daily, are preventable with the use of proper safety eyewear (Prevent Blindness America [PBA], 2005). Preventable or treatable conditions cause 80% of blindness worldwide (Lighthouse International, 2007).
Early detection of eye disease through regular eye exams can provide the most effective treatment and ultimately preserve vision (Figure 9-1). However, a national telephone survey of more than 3000 adults found that most Americans are not aware of risks and warning signs of the diseases that could blind them. Over 70% said that losing their eyesight would have the greatest impact on their daily life. Many considered losing their eyesight to be worse than losing an arm or leg, or losing hearing or the ability to speak (National Eye Institute [NEI], 2008a). As a result of the survey, the National Eye Institute is increasing its efforts to educate healthcare professionals about methods of communicating with patients to better maintain eye health (NEI, 2008a). At the same time, outpatient surgeries have been increasing: cataract is the leading diagnosis for ambulatory surgery visits, with more than 3 million lens extractions performed yearly (Cullen et al, 2006). The surgical technologists must keep abreast of changes in technology, procedural techniques, safety issues, and patient education resources to provide optimal care to ophthalmic surgery patients.
Surgical Anatomy
The major eye structures and normal eye function will be reviewed here; conditions requiring surgery will be discussed under Surgical Interventions. The surgical technologist uses this combined knowledge to understand the surgeon’s plan of treatment and to prepare the patient, instrumentation, supplies, and equipment for the procedure.
Bony Orbit
The two orbital cavities are situated on either side of the midvertical line of the skull between the cranium and the skeleton of the face. The seven bones that form the orbit are the maxilla, palatine, frontal, sphenoid, zygomatic, ethmoid, and lacrimal bones.
Each orbit is in the shape of an irregular, four-sided pyramid, with its base at the front of the skull and its axis pointing posteromedially toward the apex. The orbit contains the globe; orbital fat; extraocular muscles, nerves, and blood vessels; and part of the lacrimal apparatus. The orbit also acts as a distribution center for certain vessels and nerves that supply the facial areas around the orbital aperture.
The orbital septum is a sheet of connective tissue that descends from the periosteum of the orbital margin to the eyelid retractors near the skin surface. The septum protects the contents of the bony orbit, and divides the area into anterior (preseptal) and posterior (postseptal) spaces.
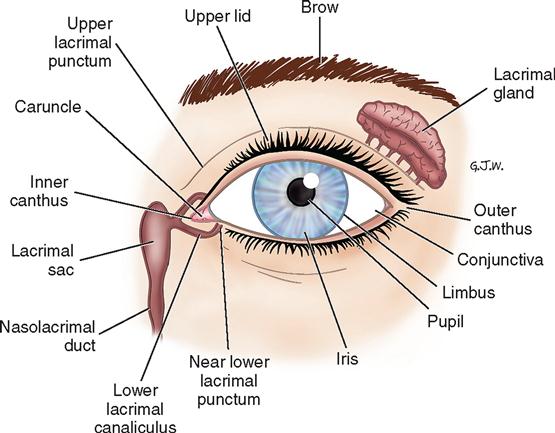
Lacrimal Apparatus
The lacrimal apparatus effectively functions like a sink, with a faucet (main and accessory lacrimal glands) and drain (lacrimal puncta, canaliculi, sac, and nasolacrimal duct). The lacrimal gland produces tears and secretes them through a series of ducts onto the anterior ocular surface, thereby keeping the cornea moist and washing away any debris. The tears then flow inward to the puncta, from which they are conducted by the canaliculi to the lacrimal sac and finally pass into the nasolacrimal duct (Figure 9-2).
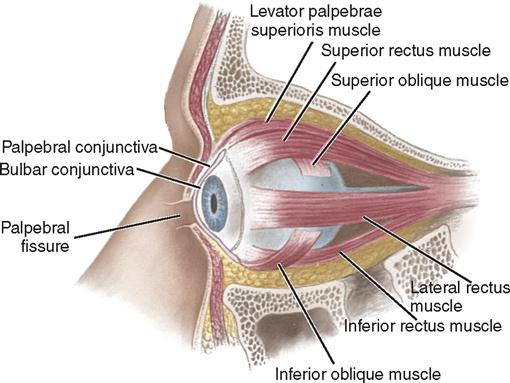
Eyelids
The palpebral fissure refers to the space between the margins of the two eyelids (Figure 9-3). When the eye is closed, the fissure becomes a mere slit and the cornea is completely covered by the upper eyelid. The upper eyelid is more mobile and larger than the lower. The upper and lower lids meet at the medial and lateral angles (canthi) of the eye. The eyelids are closed by the orbicularis oculi muscle, innervated by the seventh cranial nerve. The upper lid is opened by the levator muscle, which is innervated by the third cranial nerve.
The anterior eyelid layers contain the eyelid skin, ocular adnexa (eyelashes and associated glands), and subcutaneous tissue, lymphatics, and muscles.
The tarsus is a plate of dense fibrous tissue that forms the main scaffolding of the eyelids. The tarsus is anchored to the walls of the orbit by the medial and lateral palpebral ligaments. Within the tarsus are the meibomian glands, which secrete the oily component (sebum) of the tear film. The orifices of these sebaceous glands are found at the eyelid margin just posterior to the eyelashes.
Conjunctiva
The conjunctiva is a thin, transparent mucous membrane divided into a palpebral portion (lining the inside of the eyelids) and a bulbar portion (lining the surface of the globe) (see Figure 9-3). The junction between the palpebral and bulbar conjunctivae forms a forniceal sac.
Muscles
Named according to their relative position on the eyeball, the extraocular muscles of the eyeball include the four recti (the superior rectus, inferior rectus, medial rectus, and lateral rectus) and two oblique muscles (the superior oblique and inferior oblique) (see Figure 9-3). Except for the inferior oblique muscle, these muscles originate from the back of the orbit. The muscles work in yoked pairs, with ocular movements generated by an increase in the tone of one set of muscles and a decrease in the tone of the antagonistic muscles. The extraocular muscles are supplied by cranial nerves III (oculomotor, supplying the superior, inferior, and medial recti), IV (trochlear, supplying the superior oblique), and VI (abducens, supplying the lateral rectus).
Globe
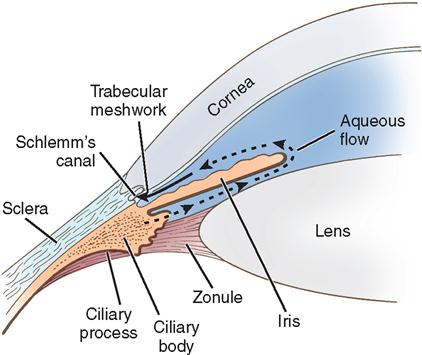
The eyeball (globe) is supported in the orbital cavity on a cushion of fat and fascia. The fibrous external layer includes the clear cornea and white sclera; the middle, vascular pigmented layer comprises the iris, ciliary body, and choroid; and the internal layer is the sensory retina. The globe is filled with two clear liquids: the aqueous humor (anterior to the lens) in the anterior segment and the vitreous humor (behind the lens) in the posterior segment. Light and images are focused (refracted) by the lens, suspended behind the pupillary opening of the iris, and the cornea (Figure 9-4).
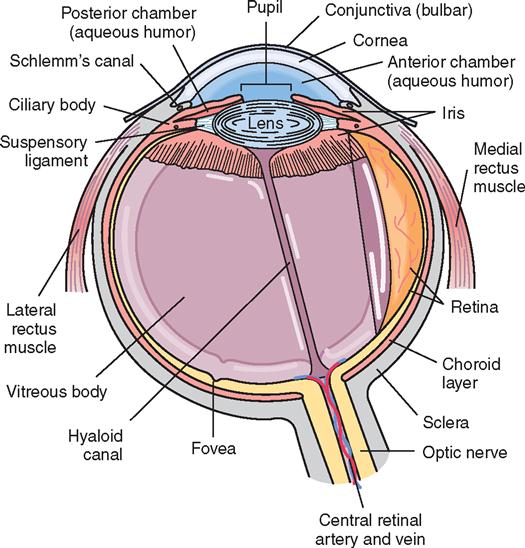
Refractive Apparatus
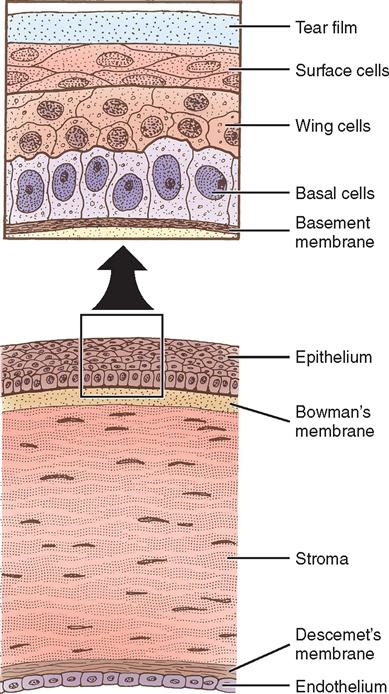
Cornea.
The cornea is the transparent, avascular window through which light rays pass to the retina; it joins the sclera at a transitional zone called the limbus. Corneal sensation is provided via ophthalmic branches of the fifth cranial nerve. The cornea is composed of five layers: the epithelium, Bowman’s membrane, the stroma, Descemet’s membrane, and the endothelium (Figure 9-5). The epithelium consists of constantly renewing cell layers with many nerve endings, accounting for the cornea’s great sensitivity to foreign bodies and abrasions. Bowman’s membrane is connective tis sue thickening that forms a barrier to trauma and infection under the epithelium. If damaged, Bowman’s membrane does not regenerate and a permanent scar is formed. The stroma accounts for 90% of the corneal thickness and is composed of precisely layered fibers. If this layering is disrupted (for example, by edema), the corneal clarity decreases. Descemet’s membrane is a thin layer between the endothelial layer of the cornea and the stroma. The corneal endothelium is a single layer of hexagonal cells that acts as a fluid pump to keep the cornea clear by maintaining the proper level of stromal dehydration. Because corneal endothelial cells do not regenerate, damage to this layer may cause persistent corneal edema and loss of transparency.
The sclera is the opaque “white” part of the external layer, and is made up of collagenous fibers loosely connected with fascia. The sclera receives attachments of the extraocular muscle tendons, and is pierced by the ciliary arteries and nerves posteriorly by the optic nerve.
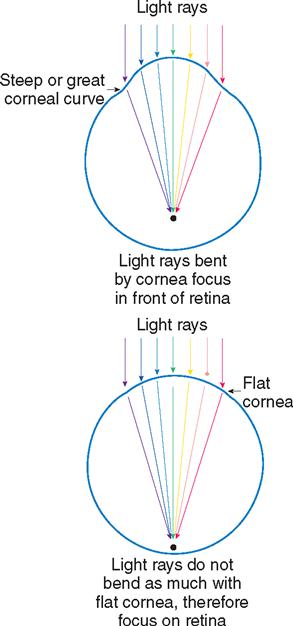
Visual images are refracted (focused) by the cornea, the aqueous humor, the lens, and the vitreous body. The cornea has the greatest refractive power of the ocular structures. Variations in the curvature of the cornea change its refractive power (Figure 9-6).
Lens.
The biconvex lens is suspended behind the iris and connected to the ciliary body by delicate collagenous strings called zonules (Figure 9-7). The lens changes shape and focus (accommodation) by relaxation and tightening of the zonular fibers. Over time (particularly after age 40), the lens and lens zonules become progressively less elastic, resulting in presbyopia. This loss of accommodative power is typically corrected with reading glasses or bifocals.
Vitreous.
The vitreous body is a glasslike, transparent, gelatinous mass composed of 99% water and 1% collagen and hyaluronic acid. It fills the posterior four fifths of the eyeball and is adherent to the retina at the vitreous base.
The eye functions similarly to a camera. Light rays from an object pass through the system of refractory devices—the cornea, aqueous humor, lens, and vitreous—and are refracted (bent) so that the rays strike the retina. For information to be received correctly and sent to the cerebral cortex, all structures must function together to focus the light rays. The lens must be able to bend the light waves correctly and bring an object into clear focus. Refractive errors, or errors in focusing ability, occur when the cornea is misshapen or when the lens cannot appropriately change shape to focus images.
Nerve and Blood Supply
The optic nerve (second cranial nerve) extends between the posterior eyeball and the optic chiasm. This cranial nerve carries visual impulses, as well as the sensations of pain, touch, and temperature, from the eye and its surrounding structures to the brain. The third cranial nerve (oculomotor) is the primary motor nerve to the inferior oblique as well as all rectus muscles except the lateral rectus, which is innervated by the sixth cranial nerve (abducens). The fourth cranial nerve (trochlear) innervates the superior oblique muscle.
The ophthalmic artery, the main arterial supply to the orbit and globe, is a branch of the internal carotid artery. It divides into branches supplying the globe, muscles, and eyelids. The central retinal artery and central retinal vein travel through the optic nerve and provide a separate blood supply for the retina.
Physiology of Vision
Clear vision requires all of the following: healthy, functioning eye structures; adequate light; intact neurovascular communication with the brain; and the brain’s effective interpretation of the images relayed. Since the eye is similar to a camera with a lens system, the following cycle, if completed in the full sequence, leads to accurate visual images:
Since early treatment for various eye diseases can potentially save sight, people 60 years of age or older should have a comprehensive dilated eye exam every 2 years as a minimum (NEI, 2008b). Any condition that disrupts eye health or the process of these steps impairs vision. Other structures within the eye exist, but it is beyond the scope of this chapter to adequately cover all details of the complex organ of sight. Specific conditions requiring surgical intervention will be explained under Surgical Interventions.
Surgical Technologist Considerations
With surgical refraction an option, the field of optometry is ever changing. Of the many surgical specialties, ophthalmic surgery can seem overwhelming to many new surgical technologists. The apprehension to this type of surgery may be related to the delicate and specialized instrumentation required or the uncomfortable image of part of the patient’s face being exposed as well as invasive work being performed on parts of the globe.
Preparation for Surgery
Preparing for eye surgery involves a great deal of planning to ensure a successful surgical day. There are numerous specialty blades and irrigating tips, suture, and an assortment of implants available to the surgeon. Planning for surgery begins well in advance of the actual surgery date. Some specialty packs require several weeks to be ordered, built, and delivered. When ordering lenses for cataract surgery, several types are needed for each eye. Generally, a surgeon will require a primary and a secondary lens. When ordering lenses, two of each type should be ordered for each eye. In other words, four lenses will be ordered for each cataract patient. Imagine what would happen if only one lens was ordered and it was damaged or otherwise rendered unusable during surgery.
Depending on where the surgical technologist is employed, he or she will have varied levels of responsibility in ordering supplies and equipment for surgical days. In some facilities, only registered nurses order the supplies and lenses.
Because of the fast pace of the surgical day, on the morning of surgery the surgical technologist will have supplies for numerous procedures prepared and ready to open for each surgical procedure. It is very important to have everything ready to go and to develop a system to do so.
Specialized equipment such as the phacoemulcification unit and the operative microscope must be in the room and checked for proper operation before the first procedure. Check that there is a back-up bulb for the microscope available so that surgery is not delayed, which can have serious consequences for the patient. Special positioning equipment must be ready for the day and any other equipment requested by the surgeon should be ready and operationally checked.
Most surgeons have a specific arrangement for the equipment and foot pedals. Be sure to look at the preference cards and confirm placement of these items with the surgeon if time allows.
Surgical instruments for ophthalmic surgery are very small and delicate. Extra care should be taken when handling these instruments. Care should also be taken to protect the blade edges because they are easily damaged.
When scrubbed for surgery, be sure to wipe any residual powder from the surgical gloves and restrict the use of linen to prevent small fibers from contaminating the eye as well as the various fluids on the field. These small particles are irritating to the eye and can potentially scratch the cornea or the lens implant.
Intraoperative Considerations
Make sure that lint from the surgical towels and drapes is controlled and that any powder is rinsed from the surgical gloves. During surgery, be aware of your equipment at all times so that it does not get bumped or jarred. Most patients are awake for these procedures and any sudden movement will startle them. Sudden movement under the microscope, especially when the surgeon has instruments in the eye, can be very dangerous. Be sure all medications and solutions are properly labeled and easily recognized. This is very important since the room lights are normally dimmed to very low levels during the procedure.
When handling implants, especially the intraocular lenses, be sure of the orientation so that it can be inserted correctly. There are newer lenses that do not have a specific orientation.
Have all ointments and dressings ready for the surgeon. It is good to develop a set routine to provide a consistent pace for each procedure.
Postoperative Considerations
Assist with the patient as needed. After the procedure, be sure to rinse all instruments thoroughly with water, especially any cannulated tips or handles. If this is not done, salt crystals from the irrigating solution can crystallize in the instruments, making them malfunction on future procedures. Be very careful to protect the tips of delicate instruments and dispose of any single-use items on the field. If an item is labeled for single use, that means per patient not per day.
Safety Measures in Administering Medications.
Medications used in the perioperative period are extremely important to the outcome of the procedure and the safety of the patient. Drugs for diagnosing and treating eye disorders are potent. One error could result in total, irreversible blindness.
The patient’s medical and ocular histories determine the selection of an appropriate ophthalmic agent. The surgical technologist should be knowledgeable about specific medication and contraindications.
The nurse checks the medication label for name, strength, and expiration date during preparation and before medication administration. This precaution is especially important because many ophthalmic drugs are distributed in single-dose units that closely resemble one another. The patient must be positively identified, and the site of the administration must be clearly translated from the physician’s orders. Abbreviations should not be used. The words “right eye,” “left eye,” or “both eyes” should be used in writing orders. Handwashing between patients when administering eyedrops is imperative, and Standard Precautions should be followed.
All solutions on and off the sterile field must be clearly labeled. To meet The Joint Commission’s 2009 National Patient Safety Goals, medications in a procedural setting must have labels that include drug name, strength/concentration, and amount (TJC, 2009). Medication errors are the most common medical errors. Compliance with requirements can be an issue. One facility found that staff are more likely to label medications when preprinted labels are provided (Jennings and Foster, 2007). Preprinted labels are commercially available. Sterile waterproof pens and labels are also available to avoid smearing from liquids.
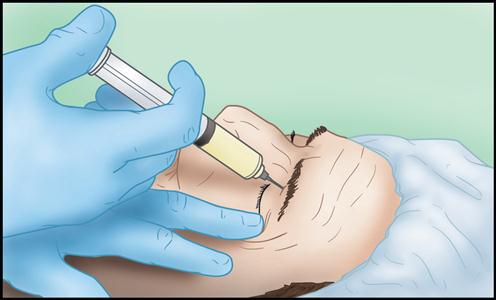
Instillation of Eyedrops.
Hand hygiene should be performed before administering eyedrops. The patient may be supine or sitting, with the head tilted back slightly. The patient will then look upward while the lower eyelid is pulled to expose the lower conjunctival sac (Figure 9-8). The prescribed number of drops is then administered without touching the tip of the dropper to the eye or the administer’s fingers. The natural blinking of the lids distributes the drug evenly onto the eye surface. When anesthetic eyedrops are instilled for topical anesthesia, they are placed on the cornea.
To minimize systemic absorption of certain eyedrops, such as atropine, the nurse may instruct the patient to press on the nasolacrimal duct for 1 minute to prevent absorption into the circulatory system.
Ophthalmic Pharmacology.
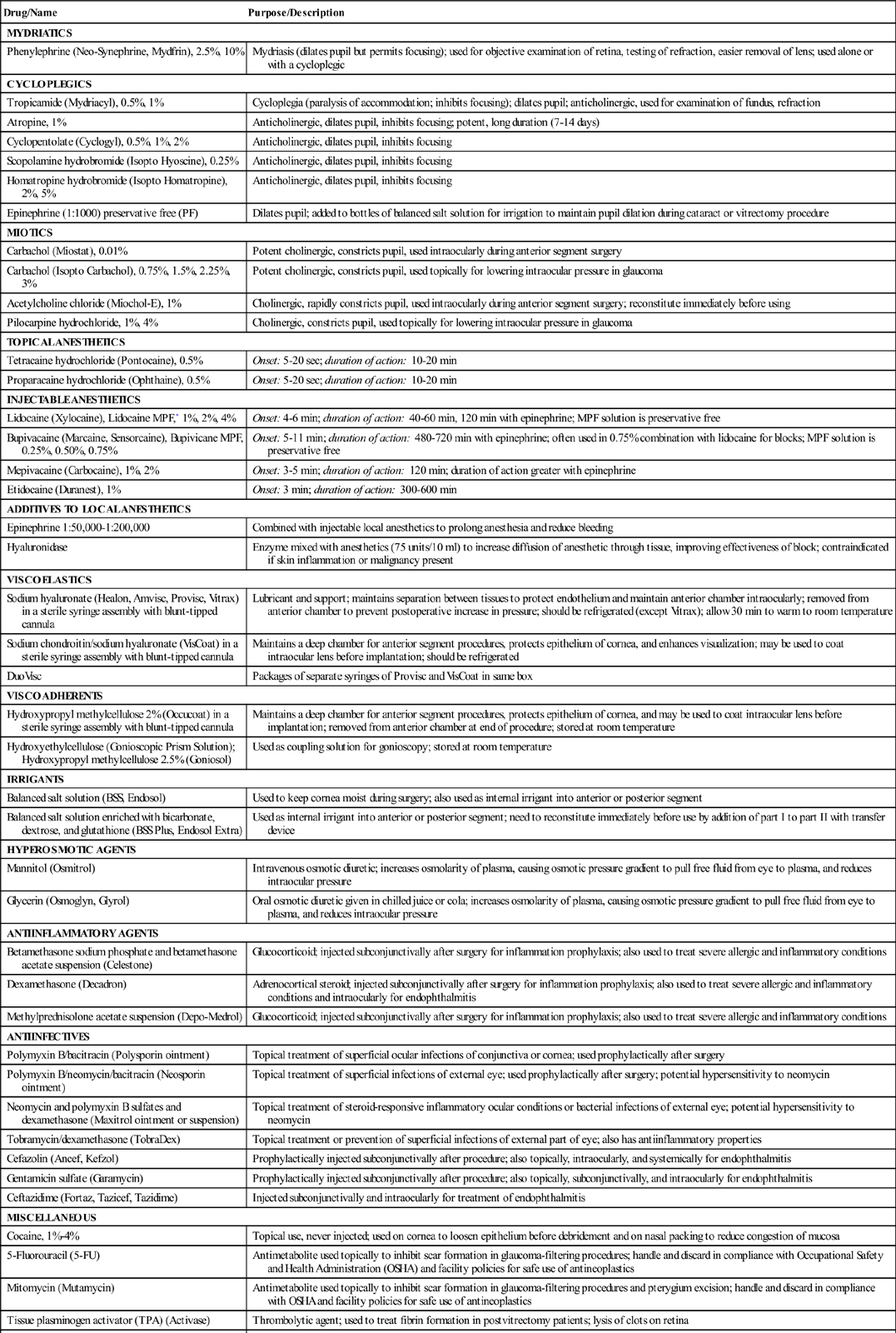
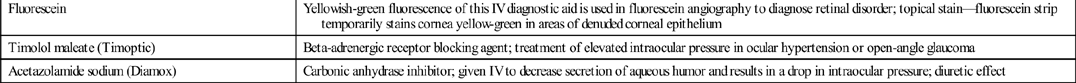
Numerous medications are used during ophthalmic surgery. See the Surgical Pharmacology table on pp. 337–339 for the purpose and description of each.
Anesthesia
GENERAL ANESTHESIA.
Youth, deafness, language barriers, dementia, severe anxiety, specific systemic diseases, known sensitivity to local anesthetics, potential of blood entering the airway (such as in tear duct procedures), and long duration of the operative procedure are among the conditions that may dictate use of general anesthesia.
LOCAL ANESTHESIA.
Local anesthesia or monitored anesthesia care (MAC) is used for most eye surgery. Consideration must be given to the patient’s age, systemic condition, and discharge plan in determining whether to use preoperative sedation, such as sublingual or oral midazolam hydrochloride (Versed). Intraoperative sedation, when indicated, may be prescribed and managed by either the anesthesia provider or the surgeon. The perioperative nurse, however, is often accountable for monitoring the patient’s response to the sedation and the local anesthetic in the perioperative period.
The perioperative nurse assembles the sterile local anesthesia setup as required by the surgeon before the patient enters the OR, checking to ensure correct medications, proper concentrations and dosages, and appropriate sizes and gauges of needles and syringes. Local anesthetics should not be mixed far in advance of the time of intended use, because they may deteriorate, producing a reduced effect for the patient. The addition of epinephrine prolongs the duration of action of most local anesthetics and the vasoconstrictive effect can reduce bleeding, often present in eyelid procedures.
Administration Methods of Local Anesthesia.
The topical method of local anesthesia has gained popularity for cataract-extraction procedures. A combination of anesthetic eyedrops is instilled into the eye and may be supplemented with infiltration of preservative-free anesthetic into the anterior chamber. Selection of patients for the topical method requires that they can cooperate and follow verbal commands to keep their eyes open and look up or down. Conditions that render the patient a poor candidate for topical anesthesia include inability to tolerate eyedrops, Alzheimer’s disease, extreme anxiety, and communication problems (e.g., language barriers, hearing impairment, auditory aphasia).
The infiltration method involves the surgeon injecting the anesthetic solution beneath the skin, beneath the conjunctiva (subconjunctival), or into Tenon’s capsule, depending on the type of surgery.
The most common technique for regional anesthesia in eye surgery is a peribulbar block. The anesthetic is injected around the soft tissue of the globe after the needle is directed to the floor (inferior) or roof (superior) of the orbit (Figure 9-9).
Retrobulbar block is injection of anesthetic solution into the base of the eyelids at the level of the orbital margins or behind the eyeball to block the ciliary ganglion and nerves (Figure 9-10). The surgeon administers the retrobulbar injection 10 to 15 minutes before surgery to produce temporary paralysis of the extraocular muscles. Since the tip of the needle cannot be visualized, training and experience are key. Potential complications of retrobulbar injection are brainstem anesthesia and death, oculocardiac reflex, perforation of the globe, and retrobulbar hemorrhage (Bollinger and Langston, 2008). Additional risks include ptosis, conjunctival or eyelid bruising, optic nerve damage, and central vein and artery occlusion. A systematic review found no evidence of difference in pain perception in surgery with retrobulbar or peribulbar anesthesia; both were largely effective. Similarly, the review found no evidence of difference in complete akinesia or need for further injections of the local anesthetic. Retrobulbar hemorrhage was uncommon; severe local or systemic complications were rare in both approaches. Overall, retrobulbar and peribulbar anesthesia were found to be equal in efficacy and safety, including acceptability to patients (Alhassan et al, 2008).
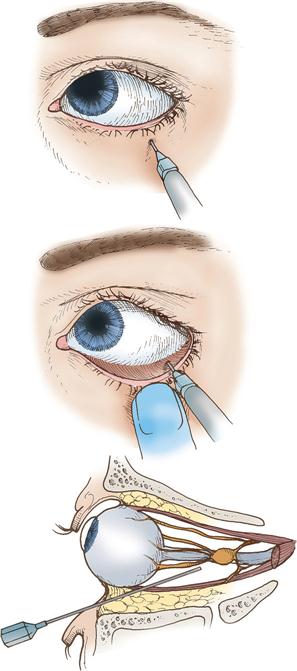
For eyelid repairs, the surgeon injects the solution through the upper or lower lid. For operations on the lacrimal apparatus, the anesthetic is injected at the level of the anterior ethmoidal foramen to anesthetize the internal and external nasal nerves. Injection of local anesthetic into the lateral adipose compartment from an inferior temporal needle insertion blocks the nasociliary, lacrimal, frontal, supraorbital, and supratrochlear branches of the ophthalmic division of the trigeminal nerve and infraorbital branch of the maxillary division; this may be used before retrobulbar block.
Positioning.
Positioning the patient for ophthalmic surgery generally requires additional devices for stabilizing the head, protecting bony prominences, and providing appropriate alignment to prevent peripheral neurovascular injury. The ophthalmology stretcher, which is a combination transport device and OR bed, is often used for convenience and comfort as the surgical bed. This special bed, with a tapered head end, allows for closer access to the patient’s face and eliminates sev eral transfers for the patient. The surgical technologist positions the patient with a foam donut or headrest under the head and a pillow under the knees. The nurse tucks the patient’s arms at the side, padding the elbows to protect the ulnar nerve, facing the palms inward and maintaining the wrists in a neutral position (Denholm, 2009). A drape secures the arms. It should be tucked snuggly under the patient, not under the mattress. This prevents the arm from shifting downward intraoperatively and resting against the OR bed rail.
If patients are to be sedated, the nurse asks if they are comfortable and offers reassurance that there are ways to increase comfort. Some elderly patients prefer not to discuss their discomfort for fear of being bothersome.
Intraocular surgery is usually carried out with the use of a microscope. A special wrist rest may be used to stabilize the surgeon’s hands and may include a perforated tubing or bar to provide oxygen under the drapes. The nurse or surgical technologist should attach it to the bed and secure it approximately 2.5 cm below the patient’s lateral canthus before draping. The wrist rest may be placed unilaterally or may encircle the head. A strip of tape may be placed over the patient’s forehead (avoiding the eyebrows) and secured to the operative bed to stabilize the head.
Prepping.
The operative site is prepped under aseptic conditions, usually after the anesthetic is administered. A sterile prep tray commonly contains sterile normal saline solution, irrigation bulb, basins, gauze sponges, cotton-tipped applicators, towels, and antimicrobial skin disinfectant.
Some surgeons order one or two drops of 5% povidone-iodine solution administered to the eye surface before the prep of the face and eyelids to decrease the number of surface microbes. Unless the patient has been administered a general anesthetic, a topical anesthetic drop is placed to minimize the stinging sensation. Povidone-iodine solution may be contraindicated in patients with allergic reactions to topical iodine. For these patients, hexachlorophene can be used as the agent for the facial prep; however, it is not applied directly to the ocular surface because of its surface toxicity.
The nurse or surgical technologist cleans the patient’s lid margins by everting the lids and cleaning with cotton-tipped applicators moistened with antimicrobial skin disinfectant, taking care to prevent the solution from entering the patient’s ears. The eye or eyes may be then irrigated with normal saline solution using an irrigating bulb. When toxic chemicals or small particles of foreign matter must be removed, the eye surface and conjunctival sac are thoroughly flushed with tepid sterile normal saline solution using an irrigation bulb or an Asepto syringe. The prep area is dried so the drape will adhere.
Draping.
Special concerns for eye surgery draping include repelling water, eliminating lint and fiber particles, and providing adequate air exchange for patients receiving local anesthetics. A cardboard bridge that adheres to the sides of the patient’s face may be used to support the drape above the patient’s mouth and nose. The surgeon may request that the nurse place a Mayo stand above the patient before the draping process to provide a platform to decrease the weight of the drapes and surgical handpieces/tubing on the patient. The use of a one-piece disposable drape, with a self-adherent, fenestrated plastic section for the eye, eliminates the need to lift the patient’s head during draping and facilitates drape removal at the end of the procedure. The eyelids may be separated when applying the self-adherent plastic eye drape to keep the eyelashes out of the operative eye. A fluid drainage bag with wicking strip may also be adhered to the plastic eye drape.
In an alternative method, the surgeon may drape the head with a half-sheet and two towels, use a large sheet or U-drape/split sheet to cover the patient and OR bed, and place a fenestrated plastic eye drape over the operative site.
Instrumentation.
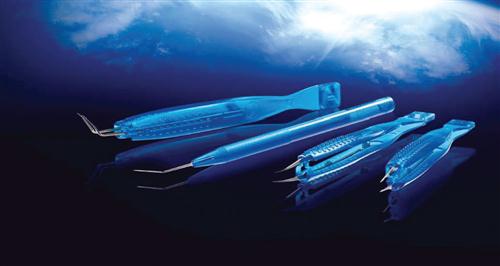
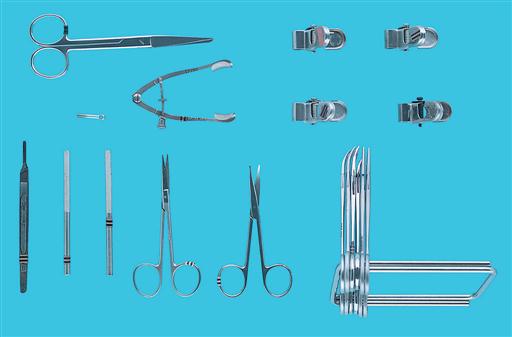
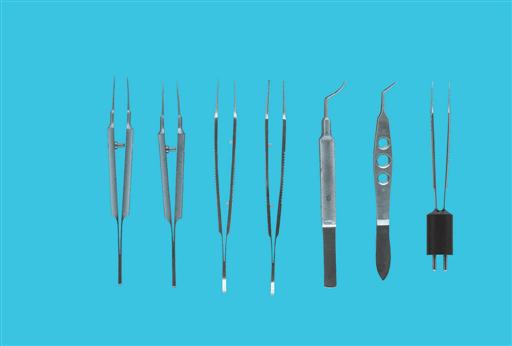
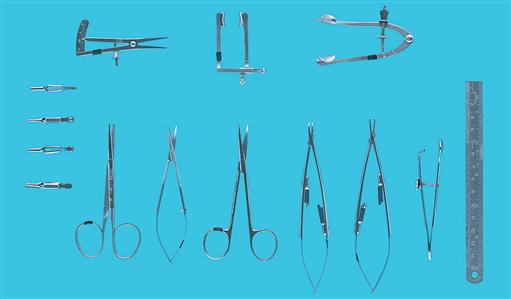
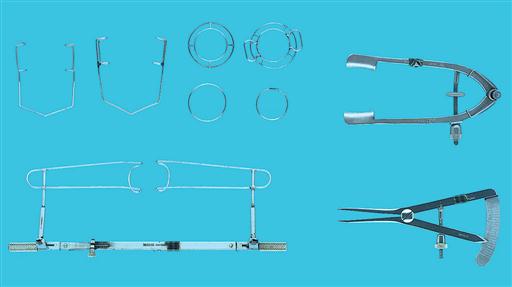
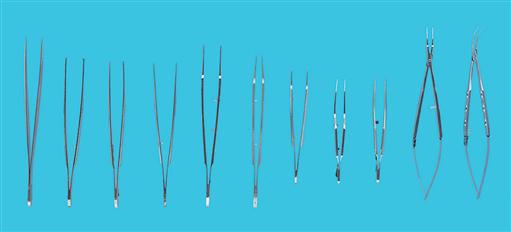
Basic eye instruments are shown in Figures 9-11 through 9-20. Additional instruments, depending on the type of procedure, can be added to the basic instrument set. Special surface finishes are used to reduce light reflection. Instruments are designed with round handles for smoother motion and rotation under the microscope. The instruments to be placed on the Mayo stand and the order of their use can also be listed on the preference card or computerized picklist.
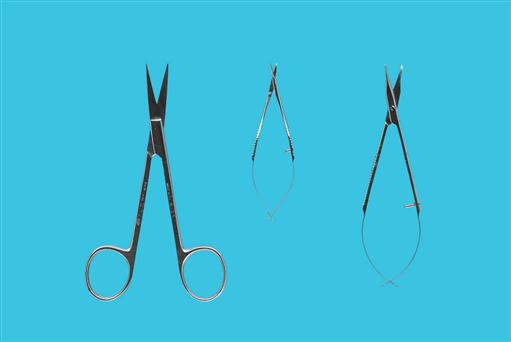
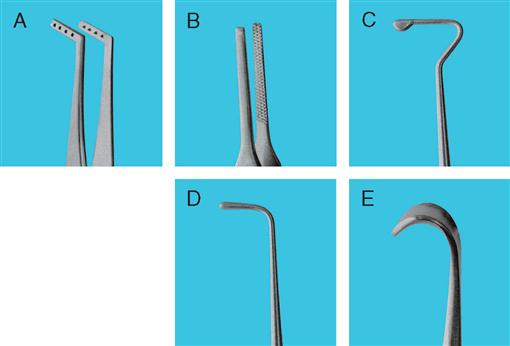
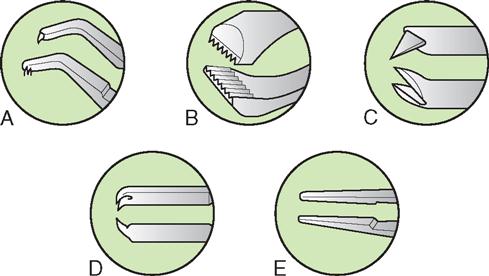
A variety of ophthalmic forceps are designed for specific use with different tissues of the eye. Fixation forceps, used to hold tissue firmly in place or provide traction before incision, have an angled tooth that overlaps for secure fixation. Suturing forceps, used to pick up wound edges for dissection or suturing, are single-toothed forceps with the tooth at a right angle to the shank of the forceps. Tying forceps have a flat platform for holding suture as it is tied. The tips of the most commonly used forceps are illustrated in Figure 9-21.
CARE AND HANDLING.
To maintain the quality and precision of all ophthalmic instruments, including microsurgi cal instruments, strict criteria for care and handling must be followed. Storage cases protect instrument tips and cutting surfaces. The instruments should be inspected under magnification when purchased and before and after each use, observing for burrs on tips, nicks on cutting surfaces, and alignment of jaws. Eye instruments should be cleaned during use with nonfibrous sponges to avoid damaging delicate instrument tips. Personnel handling instruments should know the name and purpose of each instrument. Tissue can be damaged by the use of an inappropriate instrument, and instruments can be damaged by inappropriate use. After use, the instruments should be cleaned, thoroughly dried, and terminally sterilized before storage in protective containers. A broader and more rigorous look at the entire flash sterilization process—from cleaning, decontaminating, and sterilizing to transporting—is found in The Joint Commission’s focus on optimal patient outcomes. This coincides with the AORN Perioperative Standards and Recommended Practices (AORN, 2009) in that “flashing or abbreviated cycles should not be performed for convenience, as an alternative to purchasing additional instrument sets or to save time” (Mitchell, 2009).
It is recommended that microsurgical instruments undergo ultrasonic cleaning with distilled water and an appropriate enzymatic cleansing agent. They can be individually handheld or immersed together in the ultrasonic cleaner as long as they are not touching each other. Instruments should be rinsed with distilled water and thoroughly dried. A hot air blower (never a towel) should be used for drying instruments. Instrument lubricant should not be used on irrigating cannulae because residue can be introduced into the eye and cause damage (Risk Reduction Strategies).
In addition to basic care and handling, a routine preventive maintenance program should be established for sharpening, realigning, and adjusting the precision eye instruments. Keeping an instrument in good repair is much less expensive than buying a new one. Disposable instruments (Figure 9-22) are becoming popular with surgeons because of accessibility and quality assurance; for example, forceps are properly aligned for each use because they have not been used on other procedures. Benefits for the institution include elimination of costs related to repairs. Knives are available that have safety features of retractable blades to be in compliance with the Needlestick Safety and Prevention Act, requiring implementation of safer medical devices to minimize occupational exposure to bloodborne pathogens from accidental sharps injuries, which remains a serious problem (Harris, 2008).