Xanthogranulomatous Pyelonephritis/Renal Malakoplakia
Satish K. Tickoo, MD
Mahesha Vankalakunti, MD
Victor E. Reuter, MD
Key Facts
Terminology
Xanthogranulomatous pyelonephritis (XGP), renal malakoplakia (RMP)
XGP: Subacute and chronic pelvicalyceal and renal parenchymal inflammatory mass-like lesion predominantly composed of histiocytes
RMP: Renal inflammatory mass-like lesion showing histiocytes with abundant eosinophilic cytoplasm and containing Michaelis-Gutmann bodies
XGP and RMP morphologically and possibly causally closely related
Etiology/Pathogenesis
Gram-negative bacteria are most often associated with both disorders
XGP, consistently associated with obstruction, calculi, and recurrent urinary tract infections
RMP believed to be due to defective macrophage lysosomal digestion of phagocytosed bacteria
(particularly coliforms)
Clinical Issues
Both XGP and RMP affect more females than males
Microscopic Pathology
XGP: Aggregates of foamy histiocytes forming small clusters below urothelium to large, destructive, nodular lesions
RMP: Dominant feature is aggregates of histiocytes with eosinophilic cytoplasm (von Hansemann histiocytes)
Some histiocytes contain targetoid, calcific, basophilic inclusions (Michaelis-Gutmann bodies)
Most characteristic feature of RMP
TERMINOLOGY
Abbreviations
Xanthogranulomatous pyelonephritis (XGP)
Renal malakoplakia (RMP)
Definitions
XGP: Subacute and chronic pelvicalyceal and renal parenchymal inflammatory mass-like lesion predominantly composed of histiocytes
RMP: Renal inflammatory mass-like lesion showing histiocytes with abundant eosinophilic cytoplasm and containing Michaelis-Gutmann bodies
Term derived from Greek words malakos (soft) and plakos (plaque)
XGP and RMP morphologically, and possibly causally, closely related
ETIOLOGY/PATHOGENESIS
Infectious Agents
Gram-negative bacteria are most often associated with both disorders
Escherichia coli is found in most cases
Proteus, Klebsiella, and Pseudomonas other less common pathogens
Very occasional cases associated with Mycobacterium
tuberculosis, Shigella, Paracoccidioides, Rhodococcus, Yersinia enterocolitica, Staphylococcus aureus, and Enterobacter
XGP: Consistently associated with obstruction, calculi, and recurrent urinary tract infections
RMP: Believed to be due to defective macrophage lysosomal digestion of phagocytosed bacteria (particularly coliforms)
Decreased levels of intracellular cyclic guanosine monophosphate (cGMP) might be cause of defective phagocytosis in RMP
Inadequate elimination leads to accumulation of partially digested bacteria/bacterial glycolipids
Deposition of calcium and iron occurs on residual bacterial glycolipid in monocytes or macrophages, forming Michaelis-Gutmann bodies
Patients with XGP usually have underlying systemic disease
e.g., systemic lupus erythematosus, diabetes mellitus, myotonic dystrophy, or chronic active hepatitis
CLINICAL ISSUES
Epidemiology
Incidence
XGP present in approximately 20% of specimens in which nephrectomy is performed for chronic pyelonephritic renal disease
RMP very uncommon; mostly as case reports
Age
Typically, patients are in their 40s or 50s
Both entities have been described in children and in older people (range: 4 weeks to 84 years)
Gender
Both XGP and RMP affect females more than males
Presentation
Most patients are symptomatic
Common presenting symptoms include fever, flank or abdominal pain, anorexia, weight loss, lower urinary tract symptoms, and gross hematuria
Other rare presentations of RMP
Acute renal failure with bilateral disease
End-stage renal disease
Unilateral diffuse renal enlargement
Treatment
Most patients receive antibiotics before nephrectomy
Improving immunodeficient states and use of bethanechol chloride (urecholine) are medical treatment options for RMP
Urecholine: Cholinergic agonist that improves bactericidal activity of monocytes against E. coli
Disease often only diagnosed in nephrectomy specimens in both XGP and RMP
Partial nephrectomy may be option for segmental XGP and localized RMP, if diagnosed before surgery
Prognosis
If unilateral or localized, usually cured by surgery
But, primary cause of urinary tract obstruction may need to be addressed in XGP
Immunodeficient state in RMP needs to be improved to prevent recurrences in genitourinary or other organ systems
MACROSCOPIC FEATURES
General Features
Changes may be diffuse, segmental, or focal
Pelvicalyceal system is usually outlined by thick bands of often friable, partially necrotic yellow tissue
Irregular yellow masses, usually centered on renal medulla
Masses are ill defined and at least partly necrotic
Hydronephrosis or pyonephrosis is common accompanying feature
Renal calculi, often staghorn type, very frequently associated, particularly in XGP
MICROSCOPIC PATHOLOGY
Histologic Features
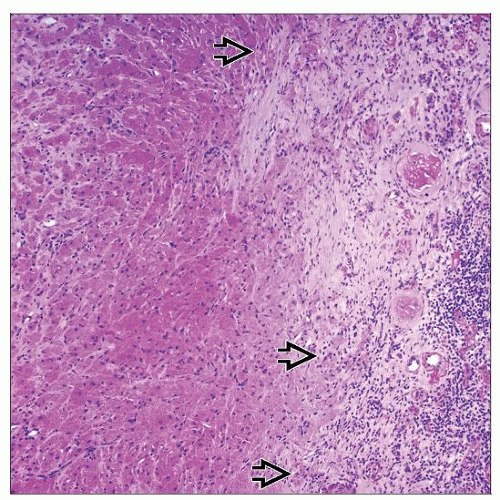
Xanthomatous pyelonephritis
Foamy histiocytes with abundant clear cytoplasm as small clusters below urothelium to large, destructive, nodular lesions
Lesions may involve pelvicalyceal tissues with secondary involvement of renal parenchyma
Histiocytes with eosinophilic cytoplasm may be present but usually not prominent finding
Admixed polymorphous inflammation with presence of lymphocytes, plasma cells, and neutrophils
Microabscesses almost always present
Variable number of multinucleated histiocytic giant cells often observed
Background of chronic pyelonephritis, characterized by
Often patchy or segmental, renal tubular atrophy, fibrosis, chronic inflammation, and tubular dilatation
Extension of process to ureter &/or perirenal fat is commonly present
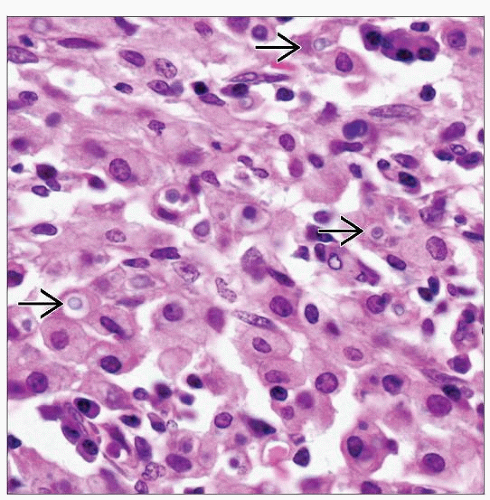
Malakoplakia
Dominant feature is aggregates of histiocytes with eosinophilic cytoplasm (von Hansemann histiocytes)
Cytoplasm often PAS(+)
Some histiocytes contain concentrically lamellar or targetoid, basophilic, often calcified inclusions (Michaelis-Gutmann bodies)
Usually equal to size of surrounding nuclei
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree