Alimentary canal contrast agents
Water-soluble agents (e.g., Gastrografin, Gastroview, Hypaque sodium oral powder)
Water-insoluble agents (e.g., BaSO4, Polibar Plus, Esophotrast, Anatrast)
Gases (CO2 gas, gas-producing calcium citrate and magnesium citrate)
Injectable contrast agents
Nonionic iodinated contrast (low osmolar agents; e.g., Omnipaque, Optiray)
Ionic iodinated contrast (high osmolar agents; e.g., Renavest, Hypaque, Conray)
Specific-use agents
Bile agents (Cholebin, Conray)
Iodized oil contrast agents
TABLE 10.1 Signs, Symptoms, and Incidence of Reactions to Iodine Contrast Media | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Know the patient’s age and health status. Children and elderly people, especially those with medical problems, may be especially sensitive to contrast agents. This sensitivity may increase the chance for side effects.
The presence of other medical problems may increase the risk for side effects.
Individuals with asthma or hay fever are at a greater risk for having an allergic reaction to the contrast agent.
Diabetic patients have a greater risk for developing kidney problems.
Those with severe hypertension may experience a dangerous rise in blood pressure and tachycardia.
Patients with kidney and liver disease may experience exacerbation of their disease.
Individuals with multiple myeloma may develop severe kidney problems.
Those with overactive thyroid may experience a sudden increase in symptoms or thyroid storm.
Those with sickle cell disease may experience the formation of abnormal blood cells.
Patients using β blockers may have a higher risk for developing anaphylactoid reactions.
Patients with chronic obstructive pulmonary disease (COPD) have an increased risk for postinjection dyspnea.
Patients who are allergic to iodine contrast media must have this information documented in their health care records. The risk for subsequent reactions increases three to four times after the first reaction; however, subsequent reactions will not necessarily be more severe than the first. The patient must be made aware of the implications of the situation. Assess for and document allergies to iodine-containing substances (e.g., seafood, cabbage, kale, raw leafy vegetables, turnips, iodized salt). Also determine each person’s reaction to penicillin or skin test for allergies because these patients have a greater chance of having a reaction.
Check the patient’s fasting status before the x-ray procedure has begun. Except in an extreme emergency, iodine contrast media should never be administered intravenously sooner than 90 minutes after the patient has eaten. In most instances, the patient should fast the night before undergoing any x-ray procedure using an iodine contrast agent.
Death from an allergic reaction can occur if severe symptoms go untreated. Staff in attendance must be qualified to administer cardiopulmonary resuscitation should it be necessary. Emergency equipment and supplies must be readily available.
Promptly administer antihistamines per physician’s order if mild to moderate reactions to iodine contrast substances occur (see Table 10.1).
When coordinating x-ray testing with a contrast agent, keep in mind that studies using iodine and those using barium should be scheduled at different times.
Some physiologic change can be expected when an iodine contrast substance is injected, as during an intravenous pyelogram (IVP). Physiologic responses to iodine given intravenously include hypotension, tachycardia, and arrhythmias. For this reason, always check blood pressure, pulse, and respiration before and after these tests are performed.
If appropriate for the patient, encourage intake of large amounts of oral fluids after the test to promote frequent urination. This flushes the iodine out of the body.
Possible contraindications to the administration of iodine contrast substances include the following conditions:
Hypersensitivity to iodine
Sickle cell anemia (use may increase sickling effect)
Syphilis (use may lead to nephrotic syndrome)
Long-term steroid therapy (iodine substances may render part of the drug inactive)
Pheochromocytoma (may produce sudden, potentially fatal rise in blood pressure)
Hyperthyroidism
COPD
Multiple myeloma
Acute asthma
History of renal failure
Pregnancy
Diabetes mellitus
Severe dehydration
Congestive heart failure
Drug therapy known to be nephrotoxic (e.g., cisplatin)
Nonionic contrast agents tend to produce fewer side effects than do ionic materials.
Patients with renal failure may develop acidosis when iodine contrast is administered.
Careful patient preparation considers patient safety, prevents complications, and can prevent repeat procedures. Assess for the following risk factors associated with a higher incidence of undesirable contrast agent reactions:
Allergy
Asthma
Previous reactions to contrast media
Repeat and high dosages administered
Diabetes mellitus
Renal failure (preexisting); many laboratories require preprocedural assessment of creatinine levels in older adults
Liver insufficiency
Multiple myeloma
Dehydration
Older adult (>65 years)
Newborns
History of seizures
Pheochromocytoma
No contrast agent is without risk for causing reactions. Benefit versus risk must be considered. For example, in a workup to detect cancer, the benefits of early detection far outweigh the dangers of cumulative radiation exposure. The patient must be informed of the risk-to-benefit ratio; the patient has a legal right to this knowledge. In instances in which contrast must be delivered to high-risk patients, prophylactic premedication with prednisone may be ordered. Consult the radiology department for further information.
Never inject iodized oils or barium into the bloodstream.
Contrast agent-induced acute renal insufficiency is a rare and dangerous complication that occurs 1 to 5 days following intravenous injection of a contrast medium. Dehydrated patients and those with serum creatinine levels >1.4 mg/dL (>123.8 µmol/L) are at greatest risk.
Intravascular iodinated contrast may interact with certain intravenous (IV) medications. These interactions produce insoluble precipitates that may lead to embolism. For that reason, an existing IV line should be flushed with saline before using this line as the mechanism for delivering contrast.
Special attention is necessary for diabetic patients because of their increased potential for renal failure and development of lactic acidosis. Diabetic persons taking oral hypoglycemic metformin (Glucophage) should have this drug withheld the day of and 48 hours following the
injection of iodinated contrast. In addition, advise the patient that his or her serum creatinine level should be rechecked 24 to 48 hours after he or she has received parenteral contrast. Examinations requiring extremely small volumes of contrast (myelography, arthrography) may not require such stringent precautions. Check with the radiology department for specific instructions.
Tests for thyroid function (serum tests as well as nuclear medicine studies) are adversely affected for several weeks to months following iodinated contrast injection.
Late reactions (2-3 days after procedure) most often occur with the use of agents such as iotrolan and iodohexane for intravascular procedures such as angiography.
Barium radiography may interfere with many other abdominal examinations. A number of studies—including other x-rays, tests using iodine, ultrasound procedures, radioisotope studies, tomograms, computed tomography (CT), and proctoscopy—must be scheduled before or several days following barium studies. Consult with the radiography department for the proper sequencing of studies.
Increased consumption of fluids will help to clear the bowel of barium.
Elderly, inactive persons should be checked for stool impaction if they fail to defecate within a reasonable length of time after a barium procedure. The first sign of impaction in an elderly person is fainting.
Observe and record findings regarding stool color and consistency for at least 2 days to determine whether barium has been evacuated. Stools will be light in color until all barium has been expelled. Outpatients should be given a written reminder to inspect their stools for at least 2 days following barium administration.
If possible, avoid giving narcotics, especially codeine, when barium x-rays are ordered because these drugs can cause decreased bowel motility that can compound possible barium-associated constipation.
Rare instances of severe allergic reactions to barium sulfate have been reported. All patients should be questioned regarding their allergic history before administration of any type of contrast agent. A history of hay fever, asthma, and other allergies places the patient at higher risk for reactions to all types of contrast agents.
The risk for postprocedure constipation or blockage of the bowel is increased in patients with the following conditions:
Cystic fibrosis
Dehydration
Acute ulcerative colitis
Barium should not be used for intestinal study in the following circumstances:
When a bowel perforation is suspected
Following sigmoidoscopy or colonoscopy, especially if a biopsy was performed, because leakage of barium from the alimentary canal can cause peritonitis. Iodinated contrast should be used in these cases.
 PROCEDURAL ALERT
PROCEDURAL ALERT
Enemas and laxatives should not be given to a person with an ileostomy in preparation for x-rays or endoscopy (see Chapter 12) because this puts the person at risk for dehydration and electrolyte imbalance. The person with a sigmoid colostomy requires irrigation of the stoma the night before and the morning of the study. Consequently, it is important to identify the type of surgical procedure the patient has undergone. Moreover, not all colostomies need irrigation. For example, a person with an ascending right-sided colostomy will usually pass a liquid, pasty stool high in water content and digestive enzymes—such a patient may only require laxatives.
Notify the radiology department that the person has an ostomy.
Advise all patients to bring extra ostomy supplies and pouches for use after the procedure is completed.
TABLE 10.2 Principal Early Effects of Radiation Exposure on Humans and Approximate Threshold Dose | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
TABLE 10.3 Relative Risk for Childhood Leukemia After Irradiation in Utero by Trimester | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
The patient’s medical records should be reviewed for previous radiological studies to minimize the potential for unwarranted repeat studies.
The size or area irradiated must be carefully adjusted so that no extra tissue than necessary is exposed to the x-irradiation. Collimators (shutters), cones, or lead diaphragms can ensure proper sizing and x-ray exposure area.
Fluoroscopy yields a higher dose than radiographs or CT studies. Significant dose reduction is achieved by employing pulsed digital fluoroscopy.
The gonads should be shielded in both female and male patients of childbearing age unless the examination involves the abdomen or gonad areas.
The primary x-ray beam should pass through layers of aluminum adequate to filter out low energy radiation while still providing detailed images.
Staff in the radiology department should wear lead aprons (and gloves if indicated) when not within a shielded booth during x-ray exposures. Patients should be shielded appropriately insofar as the procedure allows.
The x-ray tube housing should be checked periodically to detect radiation leakage and to indicate when repairs or adjustments are necessary.
TABLE 10.4 Summary of Effects After 10-rad in Utero | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
TABLE 10.5 Representative Radiation Quantities From Various Diagnostic X-Ray Procedures | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Women of childbearing age who could possibly be in the first trimester of pregnancy should not have x-ray examinations involving the trunk or pelvic regions. A brief menstrual history should be obtained to determine whether a possible pregnancy exists. If pregnancy is possible, a pregnancy test should be done before proceeding with x-ray examination.
All pregnant patients, regardless of trimester, should avoid radiographic, fluoroscopic, and serial film studies of the pelvic region, lumbar spine, and abdomen if at all possible.
Should x-ray studies be necessary for obstetric regions, repeat images should be avoided.
If x-ray studies of nonreproductive tissues are necessary (e.g., dental x-rays), the abdominal and pelvic region should be shielded with a lead apron.
First day: intravenous pyelogram (IVP) and barium enema
Second day (or subsequent day): upper GI (UGI) series
Abdominal or pelvic ultrasound examination
Lumbar-sacral spine x-rays
Pelvic x-rays
Hysterosalpingogram
IVP
examinations that do not require preparation can be performed at any time. Such examinations include the following:
X-rays of the head, spine, and extremities
Noncontrast abdominal x-rays (e.g., kidney, ureters, bladder [KUB], abdomen series)
Mammograms
Remember that routine chest radiography consists of two images: a frontal view (posteroanterior [PA]) and a left lateral view. Upright chest radiographs (digital images) are preferred and are of utmost importance because images taken in the supine position do not demonstrate fluid levels. This observation is especially important when testing patients on bed rest.
Street clothing that is covering the chest is removed to the waist. Allow only cloth or paper hospital gowns free of buttons and snaps to be worn during the x-ray. Remove jewelry on or adjacent to the chest.
Ensure that monitoring cables and patches do not obscure the chest area, if possible.
Instruct the patient to take a deep breath and to exhale; then to take another deep breath and to hold it while the x-ray image is taken. After the x-ray is completed, the patient may breathe normally.
The actual procedure takes only a few minutes.
Follow guidelines in Chapter 1 regarding safe, effective, informed intratest care.
Abnormal chest x-ray results may indicate the following lung conditions:
Presence of foreign bodies
Aplasia
Hypoplasia
Cysts
Lobar pneumonia
Bronchopneumonia
Aspiration pneumonia
Viral pneumonia
Lung abscess
Middle lobe syndrome
Pneumothorax
Pleural effusion
Atelectasis
Pneumonitis
Congenital pulmonary cysts
Pulmonary tuberculosis
Sarcoidosis
Pneumoconiosis (e.g., asbestosis)
Coccidioidomycosis
Abnormal conditions of the bony thorax include the following:
Scoliosis
Hemivertebrae
Kyphosis
Trauma
Bone destruction or degeneration
Osteoarthritis
Osteomyelitis
Cardiac enlargement
Obesity
Severe pain
Congestive heart failure
Scarring of lung tissues
No special preparation is required. However, the patient should be given a brief explanation of the purpose of and procedure for the test and assured that there will be no discomfort. Screen for pregnancy status of female patients. If positive, advise the radiology department.
Remove all jewelry and other ornamentation in the chest area before the x-ray.
Remind the patient of the need to remain motionless and to follow all breathing instructions during the procedure.
Follow guidelines in Chapter 1 regarding safe, effective, informed pretest care.
Interpret test outcomes and monitor for pulmonary disease and chest disorders. Explain changes in therapy based on chest x-ray results (e.g., diuretics for pulmonary edema, endotracheal tube repositioning, starting or stopping mechanical ventilation), although the attending physician will ultimately make all decisions in the treatment plan.
Follow guidelines in Chapter 1 regarding safe, effective, informed posttest care.
To detect clinically nonpalpable breast cancer in women >40 years of age, younger women at high risk, or those with a history of breast cancer
When signs and symptoms of breast cancer are present
Skin changes (e.g., “orange peel” skin associated with inflammatory-type cancer)
Nipple or skin retraction
Nipple discharge or erosion
Breast pain
TABLE 10.6 Likelihood of Breast Cancer
Age (yr)
Odds
30-39
1 in 233
40-49
1 in 69
50-59
1 in 38
60-69
1 in 27
Source: National Cancer Institute, 2006.
“Lumpy” breast; multiple masses or nodules
Pendulous breasts that is difficult to examine
Survey of opposite breast after mastectomy
Patients at risk for having breast cancer (e.g., family history of breast cancer)
Adenocarcinoma of undetermined origin
Previous breast biopsy
Tissue samples removed from the breast may be imaged using detailed mammography techniques
Follow-up studies for questionable mammographic images
Mammogram
Perform mammograms with the person in an upright position, preferably standing. Make accommodations for patients using wheelchairs.
Expose the breast. Elevate the inframammary fold to its maximum height. Lift onto a cassette or digital plate to the level of the inferior surface of the patient’s breast. Adjust the breast tissue by hand, smoothing out all skin folds and wrinkles. Lower a movable paddle onto the breast, rigorously compressing the breast tissue.
Make an x-ray exposure quickly and immediately lift the compression.
Typically, take two views (craniocaudal [CC] and mediolateral oblique [MLO]) of each breast.
Before or after the x-ray examination, the technologist visually observes and manually palpates the breasts.
Tell patient that the complete examination takes about 30 minutes.
Follow guidelines in Chapter 1 regarding safe, effective, informed intratest care.
X-ray-guided biopsy (stereotactic technique)
Administer a local anesthetic.
Have the patient lie on her abdomen, allowing her breast to protrude through an opening in a special table.
Take two stereo-view mammograms, allowing precise positioning of the biopsy needle.
Insert the needle into the breast at precise locations using sterile lacerations. Take multiple core tissue samples because tumors have both benign and malignant areas. In vacuumassisted biopsy procedure, a probe is inserted directly into the suspicious area, and tissue is gently vacuumed out for subsequent analysis. See Chart 10.1 for comparison of these two methods.
Cleanse the breast and apply a sterile dressing.
Needle x-ray localization and surgical biopsy
Administer a local anesthetic.
Insert a needle that holds a fine wire, clip, or biodegradable marker into the breast tissue, using stereotactic or sonographic guidance. When the needle point is at the tip of the lesion, the device is released. It stays there until the surgeon, guided by the wire, removes a specimen of the abnormal tissue.
Computer software (computer-assisted diagnosis [CAD]) scans the image and notes suspicious areas that a radiologist could miss, thus acting as a second opinion.
Many radiologists double-read all mammograms.
Comparison with old mammograms is very important. Consequently, patients are advised to have all mammograms performed at the same facility or retrieve old mammograms and bring them along when having a new study performed.
Mammographic examination of augmented breasts requires additional views that add to procedure time. The presence of implants should be communicated to the radiology department when scheduling the procedure.
Breast mass
Benign breast masses (e.g., cysts, fibroadenomas) are usually round and well demarcated.
Malignant breast masses are often irregularly shaped with extensions into adjacent tissue, generally with an increased number of blood vessels (Fig. 10.1).
When a mass is detected, additional studies are performed to help differentiate the nature of the mass. These studies may include the following:
Special x-ray magnification views of the area in question
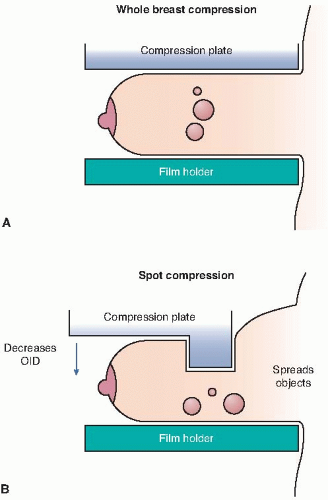
Spot compression views performed using a special paddle that isolates the suspicious tissue (Fig. 10.2)
Ultrasound of the area to help differentiate a cystic (fluid-filled) mass from a solid lesion
Calcifications present in the malignant mass (duct carcinoma) or in adjacent tissue (lobular carcinoma) are described as innumerable punctuate calcifications resembling fine grains of salt or rodlike calcifications that appear thin, branching, and curvilinear. Macrocalcifications (large mineral
deposits) generally represent benign degenerative processes. Microcalcifications (<1/50 inch) are of more concern and require close examination.
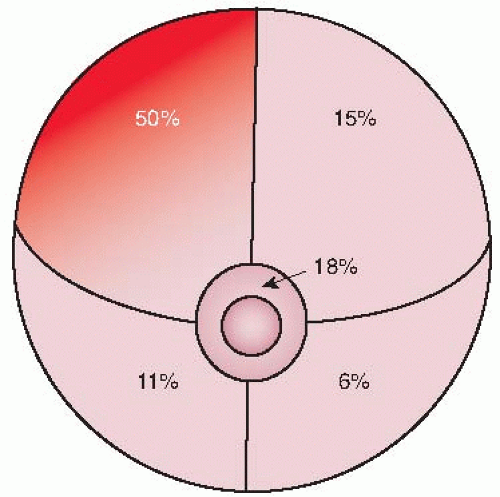
FIGURE 10.1. Half of all breast cancers develop in the upper outer section. (Courtesy of Department of Health and Human Services, 1994.)
The likelihood of malignancy increases with a greater number of calcifications in a cluster. However, a cluster with as few as three calcifications, particularly if they are irregular in shape or size, can occur in cancer.
Typical parenchymal patterns are as follows:
N1: normal
P1: mild duct prominence on less than one fourth of the breast
P2: marked duct prominence
DY: dysplasia (some diagnosticians believe that the person who exhibits dysplasia is 22 times more likely to develop breast cancer than the person with normal results)
Findings of breast cancer when contrast is injected are associated with extravasation of contrast, filling defects, obstruction, or irregular narrowing of ducts (Chart 10.2).
Core Needle Biopsy | Technique | Disadvantages | Advantages |
ABB1 Site-select Centrica | Automated gun Large core needle | Requires multiple passes into tissue | Excellent for dense lesions Relatively inexpensive equipment |
Vacuum-Assisted Biopsy (VAB) | |||
M1BB Mammotome ATEC | Dual lumen needle/probe with rotating cutter | Increased potential for postprocedural bleeding Expensive equipment | Single pass into tissue yields multiple samples Larger tissue sample |
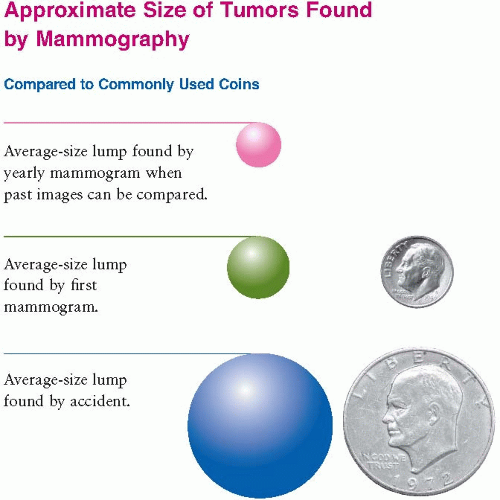
Explain the purpose, procedure, benefits, and risks of mammograms. Mammography is the single best method for detecting breast cancer while it is still in a curable stage (Fig. 10.3). Some discomfort is to be expected when the breast is compressed.
Assess pregnancy status of female patients. If positive, advise radiology department.
Instruct the patient not to apply deodorant, perfume, powders, or ointment to the underarm area on the day of the examination. Residue from these preparations can obscure optimal visualization.
Advise the patient to wear separates rather than a dress because clothing must be removed from the upper body.
Suggest that patients who have painful breasts refrain from caffeinated foods and beverages (e.g., coffee, tea, cola, chocolate, some over-the-counter medications, and most antiasthmatic medication) for 2 to 4 weeks before testing.
Follow guidelines in Chapter 1 regarding safe, effective, informed pretest care.
Contrast mammography (ductogram, galactogram) is a valuable aid for diagnosing intraductal papillomas. Mammary duct injection is used when cytologic examination of breast fluid or discharge is abnormal. In contrast mammography, after careful cannulation of a discharging duct, about 1 mL of a radiopaque substance (e.g., 50% sodium diatrizoate) is injected into the breast duct with a blunt, 25-gauge needle.
Ductal lavage is a technique in which the milk ducts are cannulated. Saline is injected and, when withdrawn, will “wash out” ductal cells. These cells are examined in the laboratory, in much the same way as a Pap test is reviewed. (See Chapter 11 for additional information.)
Interpret test outcomes and counsel appropriately. If a biopsy is necessary, see procedures for biopsy using x-ray technology.
Follow guidelines in Chapter 1 regarding safe, effective, informed posttest care.
A mammogram detects abnormalities that could warn of cancer. The actual diagnosis of cancer is made by biopsy. Only one in five biopsies tests positive for cancer.
Several methods can be used to provide a breast tissue sample necessary for cancer diagnosis. These include core needle biopsy, surgical biopsy, and vacuum-assisted biopsy. Any of these methods can utilize either x-ray mammography or ultrasound for image guidance.
red marrow storage, calcium storage, and protection of underlying soft tissue and organ structures. Orthopedic radiography is performed on the following structures:
The extremities (e.g., hand, wrist, shoulder, foot, knee, hip)
The bony thorax (e.g., ribs, sternum, clavicle)
The spine (e.g. cervical, thoracic, lumbar, sacrum, coccyx)
The head and skull (e.g. facial bones, mastoids, sinuses)
Inform the patient that dietary restrictions are not necessary.
Have the patient assume the positions most favorable to capturing the best images. However, the degree of patient mobility and physical condition may also need to be considered. Typically, the anatomic structures being studied are examined from several angles and positions. This may require the technologist to manipulate the body area physically into a position that will allow optimal visualization.
Jewelry, zippers, snaps, monitoring cables, and so forth interfere with proper visualization. These objects must be removed from the visual field if possible. Skull x-rays require removal of dentures and partials.
Removal of any surgical-type hardware used to stabilize a traumatized area should be done only under the direction of the attending physician.
Follow guidelines in Chapter 1 regarding safe, effective, informed intratest care.
Fractures
Dislocations
Arthritis
Osteoporosis
Osteomyelitis
Degenerative joint disease
Hydrocephalus
Sarcoma
Abscess and aseptic necrosis
Paget’s disease (excessive formation and breakdown of bone tissue)
Gout
Acromegaly (excess growth hormone leading to severe disfigurement)
Metastatic processes
Myeloma
Osteochondrosis, for example,
Legg-Calvé-Perthes disease (excessive loss and growth of bone in the hip joint)
Osgood-Schlatter disease (irritation of the knee joint)
Bone infarcts
Bone tumors (benign and malignant)
Foreign bodies
Explain the purpose and procedure of the test. No preparation or dietary restrictions are necessary. Screen for pregnancy status of female patients. If positive, advise the radiology department.
Assure the patient that the procedure in and of itself causes no pain. However, necessary manipulation of the body may cause discomfort. If appropriate, pain medication may be administered before the procedure.
Advise the patient that all dentures, partials, jewelry, and other ornamentation worn in the anatomic area being examined must be removed before the study. If possible, simple clothing should be worn, and the previously mentioned items should be left at home or in the patient’s room.
Emphasize the importance of not moving during the procedure unless specifically instructed otherwise. Movement distorts or “blurs” the image and often requires repeat exposures.
Follow guidelines in Chapter 1 regarding safe, effective, informed pretest care.
Advise the patient to monitor for fractures, dislocations, and other orthopedic disorders. Counsel the patient about need for follow-up procedures and treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree