Wire Localized Breast Biopsy
Michael S. Sabel
DEFINITION
The wire-localized excisional biopsy (or needle-localized biopsy) is used to obtain tissue for the diagnosis of a nonpalpable, image-detected abnormality. There are various methods for localizing breast lesions for excision, including wire localization, cutaneous markers, and radiocolloid occult lesion localization (ROLL). Wire localization is the most frequently used method and is described in this chapter.
It is preferable to use image-guided biopsy as a first step (stereotactic biopsy or ultrasound or magnetic resonance imaging [MRI]-guided biopsy), as this avoids surgery in patients with benign disease and allows for a definitive oncologic operation in patients with malignant disease. Thus, the wirelocalized excisional biopsy should be limited to patients who failed image-guided biopsy or are not suitable candidates. Wire-localized lumpectomy is a similar procedure for patients who have already been diagnosed with breast cancer, where the goal is a complete excision of the cancer with an adequate margin of surrounding normal tissue. For wire-localized lumpectomy, often, two wires are needed to “bracket” the cancer in order to assure complete removal.
PATIENT HISTORY AND PHYSICAL FINDINGS
A bilateral breast exam should be performed in all patients for whom wire-localized breast biopsy is being contemplated for two reasons. First, to assess whether or not the lesion is truly nonpalpable. If the abnormality is palpable, then wire localization will not be necessary. If an abnormality is palpated, it is critical to review with the radiologist to be sure that the palpable abnormality corresponds to the imaging abnormality being recommended for biopsy. The second reason for bilateral breast examination is to make sure there are no other palpable occult abnormalities that may also require biopsy.
For patients with biopsy-proven cancer who are to undergo wire-localized lumpectomy, a thorough history and physical examination is necessary to make sure they are suitable candidates for breast conservation therapy (BCT). Contraindications to BCT include prior radiation, collagen vascular disease, first or second trimester of pregnancy, multicentric cancer, or widespread calcifications (see Part 5, Chapter 5, Lumpectomy).
IMAGING AND OTHER DIAGNOSTIC STUDIES
The preoperative imaging is essential to the procedure. Prior to the decision to perform a wire-localized breast biopsy, the breast imaging should be reviewed to determine whether the patient is a suitable candidate for an image-guided biopsy, as this is the preferable first step. The patient’s allergies, medications (specifically aspirin or anticoagulants), or the presence of a bleeding diathesis should be reviewed. Contraindications to stereotactic core needle biopsy include an inability to adequately visualize the target lesion or an inability of the patient to remain in the position required for the procedure. Some patients may exceed the weight limit for the stereotactic table. Other factors that may preclude stereotactic core needle biopsy include higher breast density; lesions close to the skin, chest wall, or axilla; or the presence of breast implants.
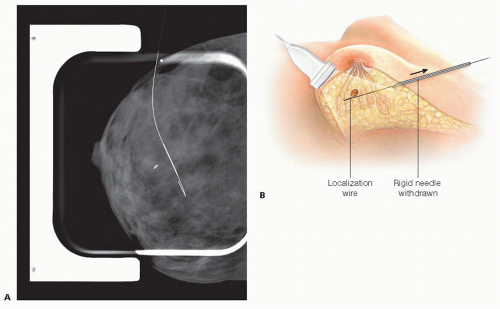
Prior to coming to the operating room (OR), the patient undergoes needle localization under image guidance. After local anesthesia, a rigid introducer needle with a hooked wire within it is directed toward the site of the abnormality using biplanar mammography (FIG 1A) or ultrasound (FIG 1B). The rigid needle is then removed, leaving the wire secured by the hook so it is not easily withdrawn or redirected (FIG 2A,B).
In many cases, a wire-localized excision is recommended after an image-guided core needle biopsy-demonstrated atypia (lobular carcinoma in situ [LCIS], atypical ductal hyperplasia [ADH], atypical lobular hyperplasia [ALH], or flat epithelial atypia [FEA]). It is also often recommended after a needle biopsy of papilloma or radial scar. In these cases, a fraction may upstage to in situ or invasive cancer.1, 2, 3, 4, 5, 6 It is good to review the pathology and indications for the biopsy prior to the procedure.
SURGICAL MANAGEMENT
Preoperative Planning
Performing a breast exam after the localization will be difficult, as the wire will be secured by a variety of methods that will preclude physical exam. These should not be removed until the patient is positioned in the OR to minimize the chance of dislodging the wire during transport.
Prior to taking the patient back to the OR, the localization films should be reviewed. Specifically, the surgeon should note the proximity of the abnormality to the wire, the direction of the wire from the point of skin entry, and how far the lesion is from the skin, as this may impact the degree of sedation (if any).
Although the risk of infection after breast surgery is low, it tends to be higher than average for a clean surgical procedure, and several studies have shown that antibiotic prophylaxis significantly reduces the risk of postoperative infection.7
Positioning
The patient should be positioned supine. Often, the localization wire is placed laterally, so the ipsilateral arm may need to be at 90 degrees.
Once the patient is on the OR table and positioned, the tape and dressings securing the wire should be removed carefully as not to dislodge the wire. A gentle breast exam can be performed at this point to see if the lesion is palpable. In addition, light palpation while watching the external portion of the wire can give the surgeon an idea of what direction the wire is heading.
The localization wire is often quite long and with a significant portion outside of the skin. The case will be facilitated by cutting the wire to a more workable length. Care must be taken not to advance the wire or pull the wire back (or out). It is also important not to cut the wire so close to the skin that it disappears. Secure the wire at the level of the skin prior to cutting with a wire cutter (FIG 3).
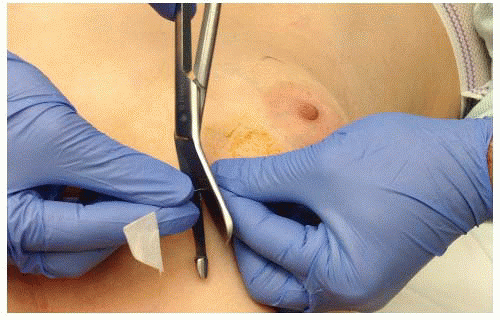 FIG 3 • The wire is secured at the level of the skin while excess wire is cut. It is important not to dislodge the wire as well as to leave an adequate amount. |
TECHNIQUES
ANTICIPATING THE LOCATION OF THE ABNORMALITY
After the dressings have been removed, the surgeon uses the site and direction of the wire along with the craniocaudal (CC) and lateral-medial (LM) views to determine the location of the abnormality in the breast. A small BB is usually placed at the site where the wire enters the skin, so it is possible to estimate how far through the breast tissue the wire extends. Remember, the breast is compressed during the mammography but not on the OR table, so the measurement on the film may not be exact. It is often helpful to identify the nipple on the mammogram as an additional landmark.
The CC view (FIG 4A) demonstrates both the anteriorposterior and the lateral-medial location of the abnormality but gives no information regarding the superior-inferior location. With a laterally placed wire, the CC view can be used to estimate how deep the lesion is and how medial (especially when also using the nipple as an additional landmark).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree