Wegener Granulomatosis
Bruce M. Wenig, MD
Key Facts
Terminology
Nonneoplastic, idiopathic, aseptic necrotizing disease characterized by vasculitis and destructive properties
Clinical Issues
In UADT, most common site of occurrence is sinonasal region with nasal cavity > maxillary > ethmoid > frontal > sphenoid
Important adjunct evaluation includes
Elevated antineutrophil cytoplasmic antibody (ANCA)
Elevated proteinase 3 (PR3)
Microscopic Pathology
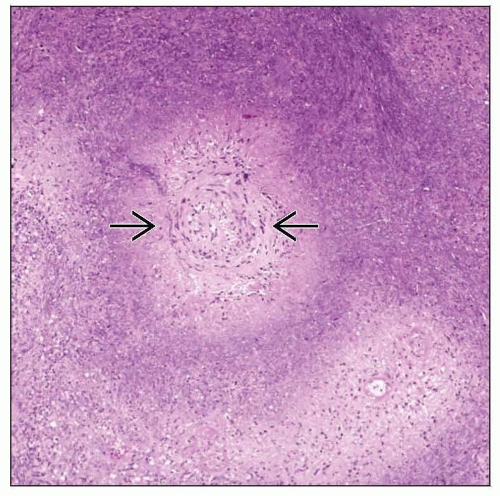
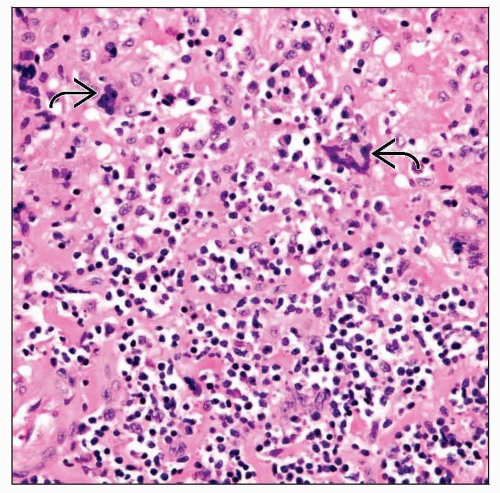
Classic triad includes vasculitis, granulomatous inflammation, tissue necrosis
In practice, finding classic histologic triad in single biopsy or series of biopsies very uncommon
Seen in only 16% of biopsies from patients with proven WG
Inflammatory cell infiltrate angiocentric and angioinvasive
Ischemic– or geographic–type (multifocal necrobiosis) with basophilic smudgy appearance
Well-formed granulomas not typical feature
Characterized by scattered or isolated multinucleated giant cells
Polymorphous inflammatory infiltrate composed of lymphocytes, histiocytes, and plasma cells
Microabscesses ± granuloma formation may be identified
TERMINOLOGY
Abbreviations
Wegener granulomatosis (WG)
Definitions
Nonneoplastic, idiopathic aseptic necrotizing disease characterized by vasculitis and destructive properties
Classic definition calls for involvement of head and neck region, lungs, and kidney
Majority of patients do not exhibit classic clinical triad simultaneously at time of initial presentation
ETIOLOGY/PATHOGENESIS
Idiopathic
Although speculative, an infectious etiology (e.g., bacterial) either as cause or as cofactor in disease suggested based on
Reported beneficial effects of trimethoprim-sulfamethoxazole therapy on initial course of disease
Histologic features of disease similar to that found in infections diseases
CLINICAL ISSUES
Presentation
May be systemic or localized
Extent of disease reflected in clinical manifestations such that limited or localized disease may be asymptomatic
Patients with systemic involvement always sick
Disease may progress from localized to systemic involvement or may remain limited or even regress with treatment
ELK classification includes
E = ear, nose, and throat involvement
L = lung involvement
K = kidney involvement
Patients with E or EL disease are considered to have limited form of WG
Patients with ELK disease correspond to systemic WG
Localized upper aerodigestive tract (UADT) WG
Tends to affect men more than women
Exception in laryngeal WG seen predominantly in women
In UADT, most common site of occurrence is sinonasal region with nasal cavity > maxillary > ethmoid > frontal > sphenoid
Other sites of involvement include
Nasopharynx, larynx (subglottis), oral cavity, ear (external and middle ear including mastoid), and salivary glands
Symptoms vary according to site of involvement, including
Sinonasal tract: Sinusitis with or without purulent rhinorrhea, obstruction, pain, epistaxis, anosmia, headaches
Oral: Ulcerative lesion, gingivitis
Ear: Hearing loss, pain
Larynx: Dyspnea, hoarseness, voice changes
Involvement of larynx most often subglottic region
8-25% of patients with WG will develop disease referable to larynx
Involvement of larynx seen more often in setting of preexisting disease elsewhere
Presentation with laryngeal WG rare event
Laboratory Tests
Important adjunct evaluation includes
Elevated antineutrophil cytoplasmic antibody (ANCA)
Elevated proteinase 3 (PR3)
Elevated ANCA
Reported specificity for diagnosis of WG from 85-98%
ANCA reactivity seen in form of cytoplasmic (c-ANCA) vs. perinuclear (p-ANCA) staining
WG characteristically associated with c-ANCA and only infrequently with p-ANCA
c-ANCA of greater specificity than p-ANCA
Sensitivity of test varies with extent of disease
Patients with limited WG have 50-67% c-ANCA positivity
Patients with systemic WG have 60-100% positivity
Negative test does not rule out WG
May be identified in other vasculitides
Inflammatory bowel disease and hepatobiliary diseases
ANCA titers not elevated in infections or in lymphomas
ANCA titers follow the disease course
Titers revert to normal levels with remission and become elevated with recurrent or persistent disease
Decline in c-ANCA titer may lag behind clinical evidence of remission by up to 6-8 weeks
Proteinase 3 (PR3)
PR3 is neutral serine proteinase present in azurophil granules of human polymorphonuclear leukocytes and monocyte lysosomal granules
Serves as major target antigen of ANCA with cytoplasmic staining pattern (c-ANCA) in WG
ANCA with specificity for PR3 characteristic for patients with WG
Patients with WG demonstrate significantly higher percentage of mPR3(+) neutrophils than healthy controls and patients with other inflammatory diseases
Detection of ANCA directed against proteinase 3 (PR3-ANCA) is highly specific for WG
ANCA positivity found only approximately 50% of patients with localized WG, whereas PR3-ANCA positivity seen in 95% of patients with generalized WG
Pathogenesis of vascular injury in WG ascribed to ANCA directed mainly against PR3
Interaction of ANCA with neutrophilic ANCA antigens necessary for the development of ANCA-associated diseases
ANCA bind to membrane-expressed PR3 and induce full-blown activation in primed neutrophils
In patients with WG, high expression of PR3 on surface of nonprimed neutrophils associated with increased incidence and rate of relapse
ANCA-associated vasculitis (AAV) includes
WG, microscopic polyangiitis (MPA), and allergic granulomatous angiitis (AGA)
Major target antigens of ANCA-associated vasculitis include PR3 and myeloperoxidase (MPO)
PR3-ANCA is marker for WG; MPO-ANCA is related to MPA and AGA
ANCA appears to induce vasculitis by directly activating neutrophils
No immunoglobulins or complement components detected in vasculitis lesions
As such, AAV called pauci-immune vasculitis
Treatment
Options, risks, complications
Once diagnosis and extent of disease is determined
Most patients receive combination of cyclophosphamide and prednisone for remission induction
Patients with limited disease treated with antibiotics (trimethoprim-sulfamethoxazole)
Rituximab therapy
Similar to daily cyclophosphamide treatment for induction of remission in severe ANCA-associated vasculitis
May be superior in relapsing disease
Patients with fulminating disease, especially with renal failure, treated with high doses of prednisone
Maintained until disease under control as evidenced by improved ESR, serum creatinine, or ANCA titer at which time cyclophosphamide therapy begun
Prednisone continued until cyclophosphamide takes effect; occurs approximately 2-3 weeks or following initiation of therapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree