Venous Access: External and Internal Jugular Veins
The external and internal jugular veins are frequently used for access to the central venous circulation. In this chapter, external jugular venous cutdown, internal jugular venous cutdown, and percutaneous internal jugular venous cannulation are presented. Because the most common method is percutaneous internal jugular venous cannulation, several approaches (posterior, anterior, and ultrasound-guided) are discussed.
The anatomy of the carotid sheath is introduced. The carotid artery and the anatomy of the carotid region are discussed in greater detail in Chapter 9.
Steps in Procedure—External Jugular Vein Cutdown
Position patient with head turned to one side, slight Trendelenburg positioning
Identify external jugular vein
Small transverse incision in midneck
Identify vein and dissect proximally and distally
Tunnel catheter
Ligate vein cephalad and cannulate vein, directing it centrally
Confirm central location
Tie vein around catheter
Close skin incision and secure catheter
Hallmark Anatomic Complications
Carotid artery puncture
Pneumothorax
Failure of catheter to pass centrally
List of Structures
External jugular vein
Internal jugular vein
Common facial vein
Common carotid artery
Platysma muscle
Sternocleidomastoid muscle
External Jugular Venous Cutdown
The external jugular vein, because of its superficial location, is an easy site for venous cutdown or percutaneous cannulation. Difficulty is often encountered in passing a catheter centrally from this location. In addition, the vein is often thrombosed in patients in whom the procedure has been attempted before. For these reasons, the more difficult internal jugular approaches may be preferred.
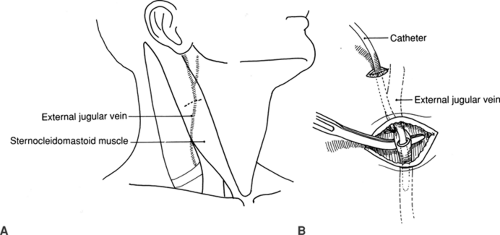
Venous Anatomy of the Neck and External Jugular Venous Cutdown (Fig. 8.1)
Technical Points
Position the patient with the head turned to one side. A slight Trendelenburg position will increase venous pressure in the neck, facilitating identification of the vein and decreasing the chance of venous air embolism. Apply pressure to the platysma muscle just above the clavicle and identify the external jugular vein as it distends with blood. Infiltrate the area overlying the vein with local anesthetic and make a small transverse skin incision over the vein in the midneck. Make the incision with care to avoid injury to the vein, which lies very superficially. Identify the vein and dissect parallel to the vein proximally and distally for a length of about 1 cm. Elevate the vein into the wound with a hemostat. Ligate the vein proximally (cephalad) and place a ligature around the distal vein.
The catheter should enter the skin at a separate site, rather than through the cutdown incision. Make a small incision about 2 cm above the skin incision and tunnel the catheter under the skin to the incision. A Broviac or Hickman-type catheter is tunneled under the skin of the chest wall to an exit site located at a flat, stable location. Generally, the
parasternal region, about 10 cm below the clavicle, is selected as the exit site.
parasternal region, about 10 cm below the clavicle, is selected as the exit site.
Use a number 11 blade for performing a small anterior venotomy, then introduce the catheter. Because of angulation at the juncture of the external jugular vein and the subclavian vein, there may be a tendency for the catheter to “hang up” or to pass out toward the arm rather than centrally. If this occurs, turn the patient’s head back toward the side of cannulation and reattempt to pass the catheter centrally. If necessary, use a floppy-tipped guidewire, under fluoroscopic control, to guide the catheter into the superior vena cava. Tie the catheter in place distally.
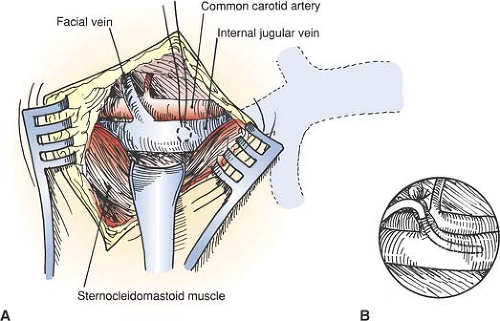
Secure the catheter in position and close the incision with interrupted absorbable sutures. If the external jugular vein cannot be cannulated or the central venous circulation cannot be accessed using this approach, extend the incision medially and proceed to the internal jugular vein (Fig. 8.2).
Anatomic Points
The external jugular vein begins in the vicinity of the angle of the mandible, within or just inferior to the parotid gland. It runs just deep to the platysma muscle. Its course is approximated by a line connecting the mandibular angle and the middle of the clavicle. It crosses the sternocleidomastoid muscle and pierces the superficial lamina of the deep cervical fascia roofing the omoclavicular triangle. It continues its vertical course to end in either the subclavian or, about one third of the time, the internal jugular vein. When it pierces the superficial lamina, its wall adheres to the fascia. This tends to hold a laceration of the vein open and predisposes the patient to air entrance if the vein is severed at this site. The vein can be occluded by pressure just superior to the middle of the clavicle, a point slightly posterior to the clavicular origin of the sternocleidomastoid muscle. The diameter of the external jugular vein is quite variable and appears to have an inverse relation to the diameter of the internal jugular veins. The right external jugular vein is typically larger in diameter than the left, partly because it is more closely aligned with the superior vena cava and thus the right atrium.
At midneck, the external jugular vein is covered only by the platysma muscle and minor branches of the transverse cervical nerve. This branch of the cervical plexus, carrying sensory fibers of C2 and C3, pierces the superficial lamina of the cervical fascia at the posterior edge of the middle of the sternocleidomastoid, then crosses the sternocleidomastoid muscle, passing deep to the external jugular vein to innervate the skin of the anterior triangle of the neck.
Steps in Procedure—Internal Jugular Cutdown
Choose right side if possible, turn head to left, slight Trendelenburg position
Transverse incision centered over division of sternocleidomastoid
Deepen incision through platysma and spread two heads of sternocleido- mastoid
Identify internal jugular vein
Dissect in anterior adventitial plane to free several centimeters of vein
Place pursestring suture
Tunnel catheter
Cannulate vein
Tie pursestring suture around vein
Confirm position of catheter
Close incision
Internal Jugular Venous Cutdown
Dissection to the Internal Jugular Vein (Fig. 8.2)
Technical Points
Choose the right internal jugular vein whenever possible. Position the patient supine with the head turned to the contralateral side. The table should be flat or in a slight Trendelenburg position to distend the veins of the neck and minimize the chances of venous air embolism. Infiltrate the skin of a planned transverse skin incision about 2 cm above the clavicle. Make an incision about 3 cm in length, centered over the triangle formed by the division of the sternocleidomastoid muscle into its medial and lateral heads.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree