Vascular Access for Hemodialysis
Beth A. Ballinger
The creation of an arteriovenous fistula is a common procedure for surgeons involved in dialysis programs. The goal of this procedure is to create an accessible, high-flow (300 mL/minute) conduit that can withstand repeated puncture by large-bore (16-gauge) needles and yet remain patent and uninfected. The most common access procedures are performed in the forearm. The Brescia-Cimino arteriovenous fistula is the preferred form of access because it is constructed from the patient’s own tissue, making it durable and resistant to infection. When a fistula cannot be constructed, an arteriovenous hemodialysis graft using polytetrafluoroethylene (PTFE) is then created.
Steps in Procedure
Preoperative venous marking with ultrasound—optional
Brescia-Cimino
Create longitudinal incision lateral to radial artery at wrist
Identify and mobilize vein, ligating collaterals—vein should be 2.5 mm in diameter
Divide forearm fascia to expose radial artery
Mobilize sufficient length for proximal and distal control and 8- to 10-mm anastomosis
Divide vein and ligate distal end
Spatulate proximal end of vein
Create end vein to side artery anastomosis with running 8-0 or 8-0 polypropylene
Access with Prosthetic Graft
Horizontal incision one fingerbreadth below the antecubital joint crease
Expose brachial artery, medial antebrachial vein, median basilica vein, and median cephalic vein
Mobilize brachial artery
Choose a large vein from among those encountered
Create subcutaneous tunnel for graft
Anastomose spatulated ends of graft to artery and vein
Hallmark Anatomic Complications
Steal syndrome from excess flow through fistula
Sore thumb syndrome from venous hypertension
Injury to median nerve in antecubital fossa
List of Structures
Radial artery
Cephalic vein
Basilic vein
Superficial fascia
Median basilic vein
Median cephalic vein
Median antebrachial vein
Brachial artery
Median nerve
Biceps brachii tendon
Bicipital aponeurosis
Brachioradialis tendon
Supinator muscle
Radial nerve
Superficial radial nerve
Lateral antebrachial cutaneous nerve
Medial antebrachial cutaneous nerve
Musculocutaneous nerve
Anatomic snuffbox
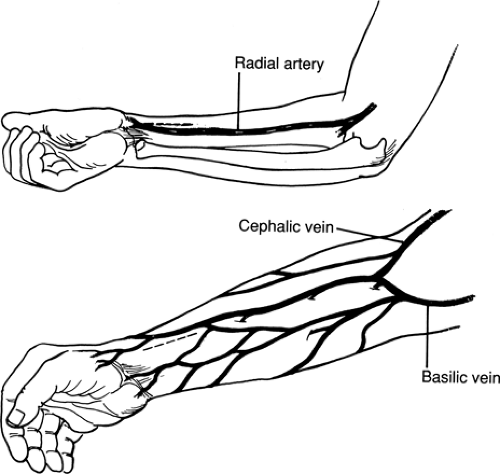
Incision and Identification of a Suitable Vein (Fig. 36.1)
Technical Points
The radial artery and the cephalic vein may be exposed through a single incision placed 1 cm lateral to the longitudinal axis of the radial artery. The nondominant upper extremity is preferred for dialysis access, presuming the vessels are of good quality because this allows freedom of movement for the dominant hand during the considerable hours spent undergoing hemodialysis.
Establish the position of the wrist joint crease by inspecting the skin folds of the flexed wrist. Place a tourniquet above the elbow to facilitate inspection of the distended veins of the forearm. When available, preoperative duplex Doppler ultrasound provides useful information regarding quality and patency of venous conduits. Phlebitic, occluded, or stenotic veins, whether at the forearm, brachial, or axillosubclavian level, will mandate selection of an alternate site. Large side-branch tributaries of the cephalic vein may be identified on ultrasound; these should be ligated to promote fistula maturation. A straight vein that is confined to the anterior surface of the arm and has few tributaries is ideal for the creation of a fistula.
Place the incision proximal to the mobile areas of the wrist to prevent normal joint motion from affecting the anastomosis. A longitudinal incision, placed parallel to the vessels, allows the vein to be dissected far enough distally to reach the artery easily. Sharp dissection will minimize adventitial loss and destruction of the vasa vasorum when dissecting the vein. Bathing the vein in a dilute papaverine solution minimizes vasospasm and allows more accurate assessment of conduit quality and size.
Anatomic Points
The goal of this procedure is to anastomose the cephalic vein, located in the superficial fascia lateral (or dorsal) to the brachioradialis tendon, to the radial artery, located deep to the deep fascia and medial to the brachioradialis tendon. An incision 1 cm lateral to the axis of the radial artery, or directly over the brachioradialis tendon, will provide access to both of these vessels. A longitudinal incision carries less risk of dividing the sensory nerves in this area, which are branches of the superficial branch of the radial nerve. These branches frequently communicate with branches of the lateral antebrachial cutaneous nerve, a sensory branch of the musculocutaneous nerve. This incision can also easily be extended. The cephalic vein begins on the dorsum of the hand over the anatomic snuffbox, draining the lateral aspect of the dorsal venous arch. At approximately the junction of the distal and medial thirds of the forearm, it courses from the lateral aspect of the forearm to lie on its anterolateral surface. Distal to the cubital fossa, it has a wide communication with the median cubital vein, which is an oblique communication with the basilic vein. In the cubital region, there is typically a large communication between the superficial cephalic or median cubital vein and the deep venous drainage in the cubital fossa. The cephalic vein usually is accompanied by branches of the superficial radial nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree