Uterus, Endometrium: Diagnosis
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Determine if carcinoma is present with features indicating need for further staging
Change in Patient Management
Surgeon may perform pelvic &/or paraaortic lymph node dissections if endometrial carcinoma with the following features is present
Grade II or III
Invasion beyond 50% of myometrial thickness
Cervical involvement
Clinical Setting
Diagnosis of carcinoma or endometrial intraepithelial neoplasia (EIN) will usually have been made with a prior biopsy
Occasionally, atypical findings during surgery at time of routine hysterectomy may prompt intraoperative consultation
SPECIMEN EVALUATION
Gross
Orient uterus according to anterior and posterior aspects
Outer surface of uterus is inspected for areas suspicious for direct tumor invasion or serosal implants
Any suspicious areas should be differentially inked
Open uterus along lateral edges using scissors
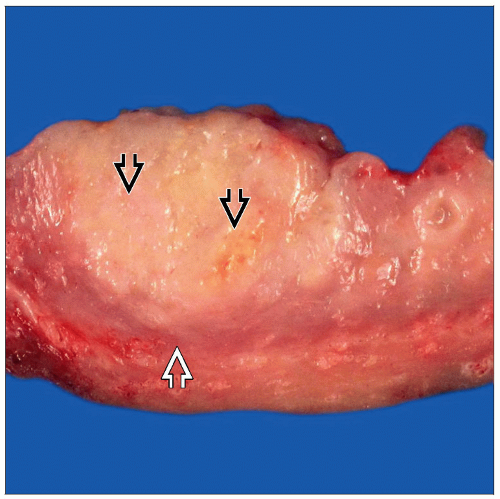
Inspect (but do not touch) endometrial lining for gross evidence of carcinoma
Pale yellow-tan heaped-up and firm areas
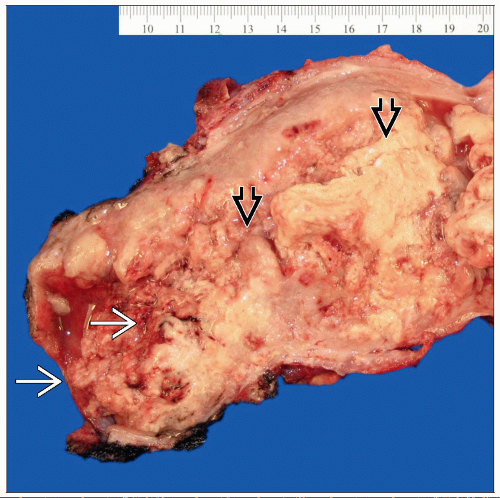
Make serial transverse incisions at 5 mm intervals from mucosal surface to, but not through, serosa
Specimen should be kept intact to maintain orientation
Myometrial invasion grossly appears as effacement of normal myometrial texture
Carcinoma often presents as tan-yellow- white homogeneous mass replacing normal myometrium
Depth of invasion can sometimes be determined grossly
Surfaces of ovaries and fallopian tubes are carefully inspected
Ovaries are serially sectioned and inspected for any mass lesions
Frozen Section
Section of the area of suspected deepest invasion is frozen
Areas of suspected cervical, fallopian tube, or ovarian involvement may be evaluated by frozen section as well
MOST COMMON DIAGNOSES
Endometrial Carcinoma
˜ 50% of cases
Endometrial lining may appear heaped-up
Carcinomas are typically pale yellow to tan and friable
Histologic types
Endometrioid: Most common type, composed of glands lined by columnar epithelium
Clear cell: High-grade carcinoma with variable cytoplasmic clearing, tubulocystic glands with hobnailed cells, and stromal hyalinization
Serous: High-grade carcinoma composed of slit-like glandular spaces lined by highly atypical cells with prominent nucleoli
Carcinosarcoma: Any of the above carcinomas with a malignant mesenchymal (stromal) component
Grade
Grade II or III is an indication for staging biopsies
Depth of invasion
Uterine wall is serially sectioned to identify greatest depth of invasion that can be seen grossly
Myometrial invasion is detected by effacement of normal myometrial texture
Endometrial Stromal Sarcoma
Usually diffusely infiltrative
Lymphovascular invasion can be seen as worm-like masses in myometrium
Irregular nests or tongues of malignant stromal cells or solid growth pattern
Endometrial Polyp
˜ 10-15% of cases
Usually, broad-based finger-like projection from endometrial wall
Central portion consists of fibrous stroma, and surface is covered by endometrium
Adenomyosis
˜ 10% of cases
Normal endometrium is deeply embedded within myometrium
Can mimic invasion when involved by carcinoma
Consists of thick, trabeculated muscle fibers with small, pinpoint hemorrhages
Endometrial Intraepithelial Neoplasia (EIN)
Generally not grossly evident
Closely packed glands with intervening stroma
REPORTING
Frozen Section
In cases of EIN or atypical hyperplasia, frozen section diagnosis of “at least EIN in 1 examined section” is appropriate with a note deferring further classification to more extensive sampling of endometrium
If carcinoma is present, the following features are reported
Type (endometrioid, clear cell, serous, or carcinosarcoma)
Grade
Depth of invasion
Cervical involvement
Serosal, ovarian, or fallopian tube involvement
Attempted diagnosis of type of carcinoma and depth of invasion should be made for each case
If cervix and adnexa are grossly negative, this should be reported
Reliability for Carcinoma
Grade is accurate in 67-96% of cases
Depth of invasion is accurate in 85-95% of cases
Cervical involvement is accurate in 65-96% of cases
False-positive diagnoses
In ˜ 9% of cases, > 50% myometrial invasion is reported but not confirmed on permanent sections
False-negative results
In ˜ 10% of cases, myometrial invasion is not reported but is found on permanent sections
PITFALLS
Carcinomatous Involvement of Adenomyosis
Depth of invasion can be difficult to determine when adenomyosis is present
Lymphovascular Invasion vs. Myometrial Invasion
Tumor in deep lymphatics can be mistaken for myometrial invasion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree