Upper Extremity Arterial Reconstruction and Revascularization Distal to the Wrist
Michael G. Galvez
James Chang
DEFINITION
Arterial reconstruction and revascularization distal to the wrist requires reconstituting the complex vascular supply to the hand. This includes the ulnar and radial arteries, superficial and deep palmar arches, and common and proper digital arteries. This reconstitution is performed with either end-to-end primary vascular repair, interposition vascular graft bypass with proximal and distal anastomoses, or addressing the digital arteries individually. Additionally, fasciotomy for compartment syndrome following trauma or reperfusion injury may be a necessary adjunct.
DIFFERENTIAL DIAGNOSIS/PRECIPITATING CAUSES OF HAND ISCHEMIA
Arterial injury
Traumatic (laceration, high energy or crush injury, etc.) or iatrogenic injury (including inadvertent or intentional cannulation for vascular access).
Proximal embolization
Intraluminal thrombosis
Hypothenar hammer syndrome occurs when the base of the hypothenar eminence sustains repeated blunt trauma resulting in chronic injury to the distal ulnar artery and the superficial palmar arch. In this scenario, compression occurs between the roof of Guyon’s canal and the hook of the hamate bone, resulting in aneurysmal degeneration of the ulnar artery, luminal thrombus accumulation, and digital embolization (typically the ring and small finger). This typically occurs on the dominant hand of individuals participating in vocational or avocational activities involving repeated palmar impact (e.g., pipe fitters and mountain bike riders).
Spontaneous radial artery thrombosis may be associated with Buerger’s disease and is not as common as ulnar artery thrombosis.
Chronic digital ischemia secondary to vasospastic and rheumatologic disease:
Primary Raynaud’s syndrome refers to cold-induced vasospasm present in the absence of concomitant disease. The etiology of this condition remains uncertain but is likely due to an exaggerated adrenergic receptor-mediated response to cold exposure.
Secondary Raynaud’s syndrome refers to digital vasospasm which occurs in the setting of known autoimmune collagen vascular diseases and related rheumatologic disorders (such as rheumatoid arthritis). In this circumstance, a normal vasospastic response to cold or environmental stimuli is superimposed on chronic digital artery occlusive disease. Differentiation from primary Raynaud’s syndrome is most commonly made based on digital ulceration and tissue loss, conditions which uniformly develop in secondary Raynaud’s syndrome.
CREST syndrome encompasses the most common phenotypic presentation of systemic scleroderma/sclerosis: calcinosis, Raynaud’s phenomenon, esophageal stenosis, sclerodactyly, and associated telangiectasias.
Buerger’s disease, or thromboangiitis obliterans, represents a progressive, recurring necrotizing arteritis of small and medium vessels closely linked to tobacco exposure.
Compartment syndrome occurs in response to increased pressure within a fixed osteofascial anatomic space, leading to decreased arterial perfusion, irreversible myonecrosis, neuropathy, and potential limb loss. In the hand, compartment syndrome most commonly develops following crush injuries; however, intravenous infiltration, external compression, and other mechanisms may also induce increased compartment pressure.
PATIENT HISTORY AND PHYSICAL FINDINGS
Determine the hand dominance of the patient and relevant history of trauma, tobacco use, medical history (coagulopathic disorders), and occupational exposures. Additionally, the presence of palpable masses, pain, sensory changes, or color changes should be evaluated.
An Allen’s test may provide additional information regarding the relative contribution of the ulnar and radial arteries to hand perfusion. This test is performed by manual compression of both the radial and ulnar arteries, with elevation and successive opening and closing performed to drain venous blood from the hand. The time differential to reperfusion, following respective arterial release, provides qualitative insight into relative radial or ulnar dominance. In most cases, however, the ulnar artery is dominant, and modern quantitative arterial perfusion assessment by duplex imaging and digital plethysmography has largely supplanted subjective physical exam findings in the assessment of adequacy of arterial inflow.
Patients with hypothenar hammer syndrome can have complaints of pain and tenderness of the hypothenar mass, with cold sensitivity and numbness of the ring and small finger secondary to digital embolization and direct ulnar nerve compression. A pulsatile mass may, on occasion, be appreciable in the palm. Discoloration of the lateral three fingers of the hand may also be present as a result of chronic digital embolization.
Patients with spontaneous radial artery thrombosis present with pain, numbness, and discoloration of the tips of the
radial-sided digits. The area of occlusion is commonly beneath the first and third extensor compartments and can be related to compression of the radial artery by the extensor pollicis longus.1
Patients with Raynaud’s syndrome report ischemic symptoms and digital discoloration on exposure to cold. Coldinduced vasospasm may be elicited by cold emersion testing in an ice bath. A positive test is elicited by the elimination of plethysmographic pulsatile phasicity on exposure to cold, in addition to the onset of symptoms. Most patients, however, cannot tolerate this provocative test, and the clinical use of eliciting vasospastic symptoms, particularly in the presence of existing digital ulceration, is uncertain.
Compartment syndrome is a clinical diagnosis. Cardinal signs include persistent and progressive pain unrelieved with immobilization/elevation, tightness of skin, pain with passive extension, and decreased sensation. Reduced skin temperature, pallor, and pulselessness are often late findings.
The intrinsic compartments are tested for pain with passive adduction and abduction of the fingers. The thenar compartment is tested by adduction of the thumb. The adductor of the thumb is tested by passive palmar abduction. The hypothenar compartment is tested by adduction of the small finger.
Normal intracompartment pressures are less than 10 mmHg; between 10 and 20 mmHg is considered high but not enough to cause muscle necrosis. An acute compartment syndrome is assumed if the measured interstitial tissue pressures are within 30 mmHg of the mean arterial pressure or 20 mmHg of the diastolic blood pressure.2 Hand pressures are typically difficult to assess on the basis of direct measurement, given the extensive septation of the fascial compartments, underscoring the importance of clinical diagnosis. When in doubt, it is prudent to proceed with operative fasciotomy.
IMAGING AND OTHER DIAGNOSTIC STUDIES
As previously mentioned, noninvasive vascular imaging and physiologic assessment are essential to establishing the diagnosis of hand and digital ischemia as well as providing a physiologic corollary to subsequent arterial imaging studies obtained to outline the relevant anatomy. Noninvasive testing informs and should always precede anatomic imaging studies regardless of modality.
Imaging provides essential identification of normal and variant arterial anatomy, recognition of the location and extent of obstructive and aneurysmal disease, and operative planning.
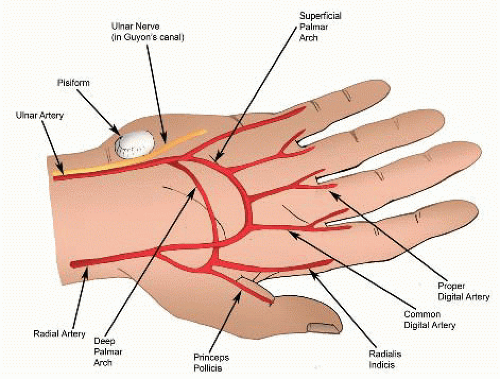
The vascular anatomy of the hand includes the ulnar artery, radial artery, and sometimes a persistent median artery (5% of the population). The ulnar and radial arteries anastomose to form the superficial and deep palmar arches, with the ulnar artery being the main contributor to the superficial arch and the radial artery the main contributor to the deep palmar arch (FIG 1). There is significant variation in the vascular patterns of the superficial and deep palmar arches.
The superficial palmar arch is completed by either the branches of the deep palmar arch, radial artery, or median artery in about 80% of patients. The deep palmar arch is completed by the superior branch of the ulnar artery, the inferior branch of the ulnar artery, or both in about 97% of patients.
The main branches from the superficial palmar arch are the three common digital arteries, which go to the index-middle, middle-ring, and ring-small finger webspaces, as well as the proper digital artery to the ulnar aspect of the small finger. Each digit has a dual blood supply from the radial and ulnar proper digital vessels.
The thumb has blood supply from the princeps pollicis artery, which variably arises from the radial artery, the deep palmar, or superficial palmar arch.
Catheter-directed, contrast-enhanced, digital subtraction hand arteriography provides highly detailed anatomic information and represents the gold standard in vascular imaging (FIG 2). However, there are risks from this invasive procedure, which include contrast allergic reaction, vasospasm, contrast-induced nephropathy, thromboembolic events including digital embolization and stroke, and drug reactions precipitated by intraarterial injection of vasoactive agents including Priscoline and nitroglycerin. Hence, catheter-based arteriography is best suited to operative planning in patients already determined to need reconstructive surgery.
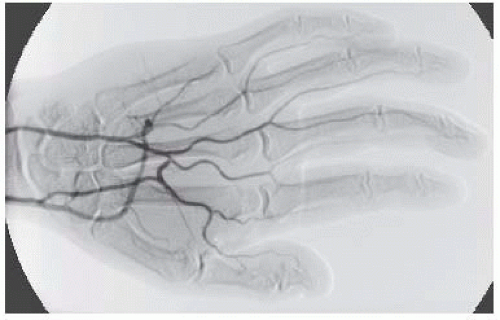
FIG 2 • Hand angiogram: normal hand angiogram demonstrating complete superficial and deep palmar arches.
Magnetic resonance arteriography (MRA) is another option for imaging that is noninvasive, eliminating risks of radiation, contrast reaction, and vasospasm. However, the resolution of MRA is not sufficient for detailed surgical planning.
Computed tomographic arteriography (CTA) is also noninvasive, although contrast and (significant) radiation exposure are required for image acquisition. Similar to MRA imaging, the resolution of CTA is typically not sufficient to support detailed surgical planning.
Measuring compartment pressures of the hand can be performed with the Stryker Intra-Compartmental Pressure Monitor (Kalamazoo, Michigan), which involves placing the device needle perpendicular to the skin and evaluating individual compartments including sites of maximum swelling of the thenar, hypothenar, and interosseous compartments. The compartment being measured should be at the level of the heart. In an intensive care unit setting, using an arterial pressure line connected to a strain gauge, zeroed at the level of needle entry into the hand, can also provide rapid and accurate compartmental measurements. A 20-gauge needle is inserted into the compartment and flushed, with measurement acquired after the flush bolus has disseminated in the compartment and the pressure spike from the flush returns to baseline.
SURGICAL MANAGEMENT
Preoperative Planning
The overall goal is to restore distal blood flow to baseline/maximal levels, given anatomic constraints, available arterial conduit, central arterial perfusion pressure and cardiac output, and end-organ (hand) viability.
Treatment of thromboembolic disease can include medical management and catheter-based chemical and mechanical thrombolysis, angioplasty, and stenting to maximize arteriolar outflow and arterial inflow, respectively. Upper extremity revascularization techniques are discussed in Part 6, Chapter 10.
End-to-end primary vascular repair can be performed if arteries are tension free after mobilization, and the zone of injury is accurately identified to be uninvolved in the site of anastomosis. If there is any difficulty in approximating the vessels ends, then vascular grafts are preferred.
In ulnar or radial artery thrombosis, reconstruction is preferred over ligation. Proximal reconstructions are attempted even in the setting of more distal occlusions, based on the rationale of augmenting collateral flow via direct or indirect means.3
Determining venous or arterial graft harvest site is important for preoperative planning. Dorsal hand or foot veins provide the most appropriate size match for intrinsic arteries of the hand (and feet). Donor sites for arterial graft conduits include the deep inferior epigastric artery, subscapular artery, thoracodorsal artery, or descending branch of the lateral femoral circumflex artery. Typically, arterial grafts patency rates are superior to those obtained with venous grafts.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree