Lesion |
Gross Features |
Morphologic and Immunolabeling Features |
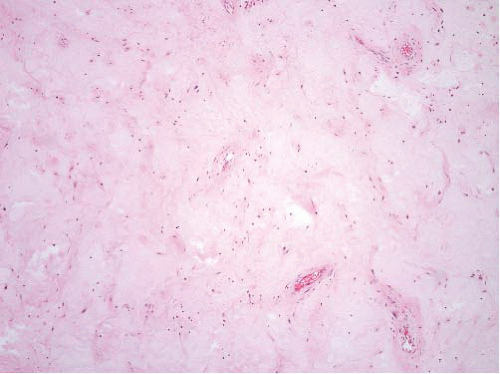
Aggressive angiomyxoma |
Usually large (>5 cm), infiltrative |
Infiltrative, myxoid. Medium to large-sized vessels with clusters of smooth muscle cells “spinning off” from the main vessel wall. Variable ER, PR, desmin, actin, CD34. |
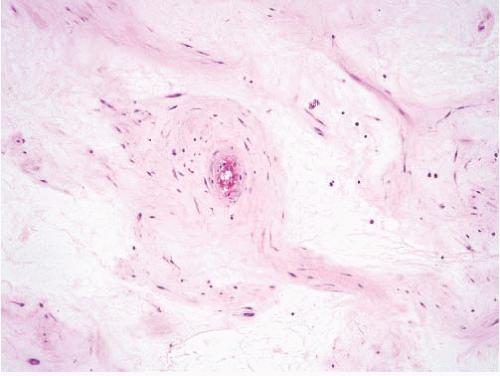
Angiomyofibroblastoma |
Well marginated and small |
Plump, epithelioid cells concentrated around vessels. Variable ER, PR, desmin, actin, CD34. |
Cellular angiofibroma |
Well marginated and small |
Uniform short spindleshaped cells proliferating in edematous to fibrous stroma, wiry collagen akin to that in spindle cell lipomas. Variable ER, PR, desmin, actin, CD34. |
Fibroepithelial polyp |
Under mucosal surfaces, small |
Spindled and stellate with pale tapering cytoplasmic processes. Multinucleate cells common. Variable ER, PR, desmin, actin, CD34. |
Superficial myofibroblastoma of the lower female genital tract |
Small subepithelial lesions |
Bland ovoid, stellate, or spindled cells in a delicately collagenized stroma just under the epithelium. |
Mammary-type myofibroblastoma |
Inguinal region, buttock, abdominal wall
Painless, slowgrowing, rarely >6 cm diameter |
Circumscribed. Irregular fascicles of spindle cells, collagenous bands, adipose tissue, mast cells. Resembles spindle cell lipoma. Atypical and epithelioid variants occur.
CD34+, desmin+, SMA+/−, h-caldesmon negative. |
ER, estrogen receptor; PR, progesterone receptor; CD, cluster of differentiation; SMA, smooth muscle actin. |
|