Tuberculosis
Francisco G. Bravo, MD
Patricia J. Alvarez, MD
Key Facts
Etiology/Pathogenesis
Mycobacterium tuberculosus is etiologic agent
Mechanism of propagation is by direct inoculation, contiguous infection, and hematogenous spread
Clinical Issues
Multibacillary forms
Primary inoculation TB, scrofuloderma, TB periorificialis, acute miliary TB, and gumma
Paucibacillary forms
TB verrucosa cutis, lupus vulgaris, erythema induratum of Bazin, lichen scrofulosorum, papulonecrotic tuberculid, lupus miliaris disseminatum faciei, and granulomatous mastitis
Microscopic Pathology
3 main histological patterns
Superficial tuberculoid granulomatous with pseudoepitheliomatous hyperplasia; granulomas are very close to epidermis
Deep tuberculoid granulomas without pseudoepitheliomatous hyperplasia
Superficial and deep tuberculoid granulomas with caseous necrosis without pseudoepitheliomatous hyperplasia
Top Differential Diagnoses
Leprosy
Leishmaniasis
Sporotrichosis
Actinomycosis
Atypical mycobacterial infections
Nodular vasculitis
TERMINOLOGY
Abbreviations
Tuberculosis (TB)
Definitions
Cutaneous TB is chronic infectious disease caused by Mycobacterium tuberculosis, same bacteria that causes TB of lungs
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Mechanism of propagation is by direct inoculation, either through contiguous infection and hematogenous dissemination
CLINICAL ISSUES
Epidemiology
Incidence
Rare disease
Represents 0.5-1.4% of all tuberculosis cases even in endemic countries such as India, China, South Africa, Peru, and Bolivia
Presentation
Multibacillary forms
Primary inoculation TB (tuberculous chancre)
Patients are healthcare workers or children with no BCG immunization exposed to M. tuberculosis through household member with pulmonary TB
Lesions are usually located on face, hands, and feet
Lesion is a papule or nodule that becomes ulcerated after 2 or 3 weeks of exposure
Scrofuloderma
Most common form of cutaneous TB in developing countries (patients have pulmonary or pleural TB)
Caused by contiguous propagation of bacteria from lymph node or bone
Most commonly affected areas are neck, axillae, thorax, and groin
Lesion is an abscess that becomes an ulcer surrounded by keloid tissue with underlying fistulae formation
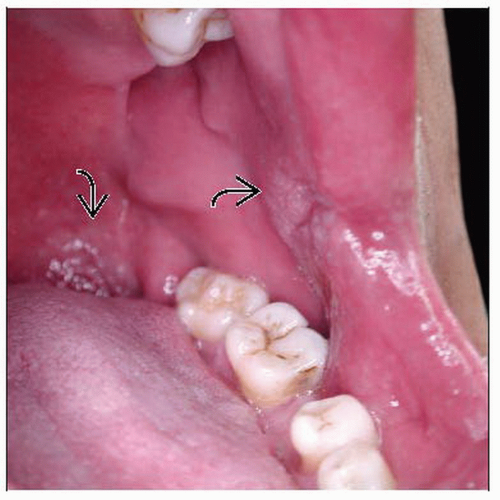
Tuberculosis periorificialis
Oral TB is secondary to active TB, which affects the upper airway or lungs, and perineal TB is secondary to intestinal or genitourinary disease
Involved areas are buccal mucosa, around anus, vulva, or penis
Lesion is painful ulcer with pseudomembranous fibrinous base or occasionally a plaque similar to those seen in lupus vulgaris or TB verrucosa cutis
Acute miliary TB
Usually seen in patients with advanced pulmonary or disseminated TB
Trunk is most common location
Lesions are small macules or papules that become necrotic
Gumma
Secondary to hematogenous spread of bacteria that remain latent
Lesions are cold abscesses in extremities or on trunk
Paucibacillary forms
TB verrucosa cutis
Caused by reinoculation to M. tuberculosis in individual with previous exposure
Affects adults and children
Lesion is solitary, verrucose plaque on hands or feet
Lupus vulgaris
Most common form in India and Europe
Lesions due to hematogenous spread are found on face, and those located on extremities occur by reinoculation
Lesion is plaque with verrucous border and central atrophy; plaque is result of multiple coalescent papules and has classic apple-jelly appearance
Tuberculids: Erythema induratum of Bazin (EIB), lichen scrofulosorum, papulonecrotic tuberculid, lupus miliaris disseminatum faciei, and granulomatous mastitis
Erythema induratum of Bazin: Most common form of tuberculid; ulcerated subcutaneous nodules on posterior aspect of legs are classic
Papulonecrotic tuberculid: Lesions are found on extensor areas of extremities but can occur on lower abdomen, trunk, or buttocks; multiple symmetric papules with umbilicated, necrotic center
Lichen scrofulosorum: Occurs mostly in children as multiple miniature follicular or parafollicular lichenoid papules; almost always affects trunk
2 controversial diseases; some consider both to be tuberculids
Granulomatous mastitis: Unilateral, ulcerated plaques or nodules on breast of female with positive contact of TB; has chronic course
Lupus miliaris disseminatus faciei: Multiple necrotic lesions on face, usually around eyelids, that leave varioliform scar
Laboratory Tests
Intradermal reaction to purified protein derivative (PPD) test or Mantoux test
> 5 mm in immunocompromised patients, HIV-positive patients, and patients with recent TB contact or x-ray changes consistent with healed TB
> 10 mm considered positive in adults and children from endemic areas or in setting of high risk (i.e., laboratory personnel involved with testing of TB)
> 15 mm considered positive in immunocompetent individuals with no known risk factor for TB infection
Treatment
Drugs
Standard therapy regiment
2 months of quadruple therapy (isoniazid, rifampicin, pyrazinamide, and ethambutol)
Followed by 4 months of isoniazid plus rifampicin
Clinical response should be expected by week 4 or 6 of treatment
Some cases require longer than 6-month regiment
MICROSCOPIC PATHOLOGY
Histologic Features
3 main patterns
Superficial tuberculoid granulomas with pseudoepitheliomatous hyperplasia (PEH), granulomas localized immediately below epidermis
Pattern seen in verrucous TB and lupus vulgaris of extremities
Deep tuberculoid granulomas that can show caseous necrosis localized in reticular dermis with normal, ulcerated, or acanthotic epidermis
Pattern seen in scrofuloderma
Superficial &/or deep tuberculoid granulomas with caseous necrosis (not always present); pseudoepitheliomatous hyperplasia is not present
Pattern seen in gummas, tuberculous chancre, TB periorificialis, facial lupus vulgaris, and lupus miliaris disseminatus faciei
Some important points
Scrofuloderma
Sometimes epidermis is normal and base of dermis is ceiling of granulomatous reaction
Lupus miliaris disseminatus faciei
Perifollicular granulomas as in rosacea can be seen
Erythema induratum of Bazin
Lobular panniculitis, necrosis of fat tissue, vasculitis of small or large vessels, and granulomatous formation
Papulonecrotic tuberculid and lichen scrofulosorum
Normal or ulcerated epidermis with superficial &/ or deep granulomas
ANCILLARY TESTS
PCR
Available and allows detection down to species level
Molecular Genetics
16S rRNA gene sequence analysis
Currently very expensive, but another option for definitive identification down to species level
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree