Transverse Colectomy: Open Technique
Y. Nancy You
DEFINITION
The transverse colon is the segment of the abdominal colon between the hepatic and the splenic flexures. The transverse colon is an intraperitoneal organ of variable length, bound by the two flexures, which are secondarily retroperitoneal areas of the colon typically fixed in position.
The main blood supply to the transverse colon is the middle colic vessels. The transverse colon, with transverse mesocolon and middle colic vessels, lies in intimate proximity to the lesser sac, which is in turn bound by the quadrate lobe of the liver, the stomach, the pancreas, and the omentum. The operative surgeon must be fully familiar with these anatomic relations in order to avoid injury to these nearby structures.
Transverse colectomy is a relatively uncommon procedure, as pathology in the proximal transverse colon is often addressed by an extended right hemicolectomy, whereas pathology in the distal transverse colon is often addressed by an extended left hemicolectomy.
Indications for transverse colectomy may be broadly divided into benign and malignant reasons.
Benign diseases with pathology focally located within the segment of the transverse colon represent the most natural indication for transverse colectomy. Examples may include focal inflammatory processes, localized trauma, or local perforation.
Transverse colectomy for primary malignancies of the transverse colon has been controversial.1 Because of the varying contributions to the lymphatic drainage of the transverse colon cancer from the ileocolic, the right colic, and the left colic blood vessels, extended right or extended left hemicolectomy has been preferred over segmental transverse colectomy for primary tumors of the transverse colon.2
Transverse colectomy may be required as a part of a curative en bloc resection of a noncolonic malignancy arising from a nearby organ due to the close proximity of the transverse colon to other structures around the lesser sac. Surgeons must be cognizant of anatomic relations in order to safely carry out the intended operation.
DIFFERENTIAL DIAGNOSIS
Endoscopic tissue biopsy is a key step in the diagnostic workup of patients with both benign and malignant diseases involving the transverse colon.
In patients presenting with a locally advanced tumor mass that obliterates the lesser sac and involves adjacent organs such as the stomach, the pancreas, and the transverse colon, care must be undertaken to differentiate malignancies of the colonic origin versus those that arose from adjacent organs but involves the transverse colon secondarily. Tissue diagnosis by biopsy should be secured in order to execute the optimal treatment regimen according to the primary malignancy.
PATIENT HISTORY AND PHYSICAL FINDINGS
The goals of preoperative assessment should include determining whether urgent versus elective intervention is needed, facilitating intraoperative planning, and assessing the benefits versus risks toward a sound surgical decision.
The patient should be examined for fitness to undergo an operation through a detailed assessment of patient’s medical history, performance status, medication regimens, other medical needs, and psychosocial competency.
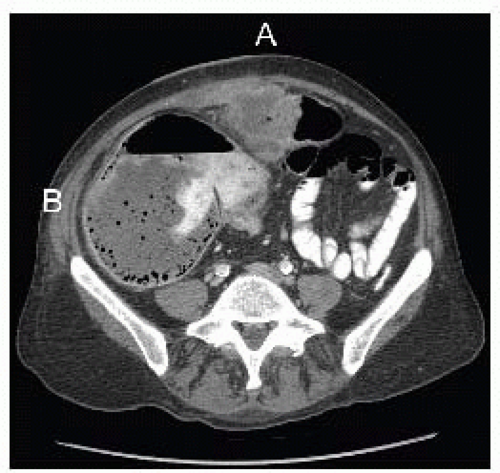
Symptoms such as abdominal cramping, difficulty with passage of stool or flatus, bleeding, or severe pain should be queried. Conditions that would necessitate urgent/emergent rather than elective surgical intervention must be ruled out. Patients with an obstructing transverse colonic lesion and a competent ileocecal valve can rapidly develop a closed loop obstruction with high risks for ischemic colon and perforation and must be attended to emergently (FIG 1).
Elements of prior surgical history that may present intraoperative difficulties such as previous stomach, pancreas, or colonic operations, and prior antecolic or retrocolic bowel bypass reconstructions, must be elicited. Prior operative reports should be obtained and reviewed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
All patients should ideally undergo both abdominal-pelvic cross-sectional imaging as well as endoscopic examination with possible biopsies.
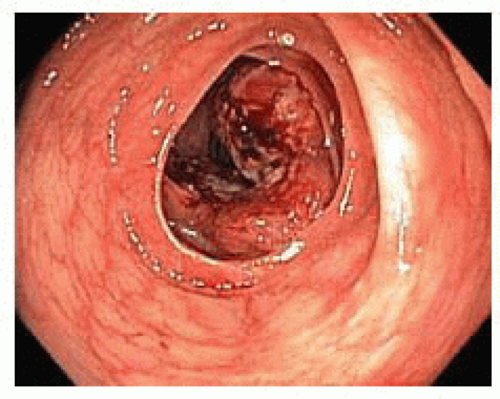
Endoscopic examination of the colon should be undertaken preoperatively to confirm the location and the focality of the pathology within the transverse colon (FIG 2).
Endoscopically, the transverse colon can be recognized by the triangular shape of the bowel lumen as well as by the anchoring landmarks of the splenic and hepatic flexures.
If there is any doubt as to whether the lesion will be able to be localized with confidence intraoperatively, then the lesion should be marked with endoscopic tattooing. If there is any concern for involvement of adjacent organs, such as the stomach, an esophagogastroscopy should also be performed.3
Cross-sectional imaging of the abdomen is performed through computed tomography (CT) or magnetic resonance imaging (MRI) scans. Imaging characteristics may supplement histologic data and aid in the differential diagnosis. In addition, percutaneous biopsy may be needed.
In cases of malignant disease, imaging will help differentiate between colonic and noncolonic origin of the disease.
Presence of distant metastatic disease and evidence of direct local invasion to adjacent organs should be assessed and appropriate intraoperative management plans should be made.
Finally, any abnormal-appearing adenopathy along vessels other than the middle colic vascular should be specifically assessed in order to determine whether the particular malignancy would be better managed through an extended right or extended left colectomy rather than a transverse colectomy.
SURGICAL MANAGEMENT
Thorough preoperative preparation, confirming that the diagnosis is correct, the indication is appropriate, and that possible intraoperative findings have been anticipated and planned for, is the basis for successful intraoperative management and the speedy postoperative recovery.
Preoperative Planning
The operative surgeon should thoroughly review the patient’s history and diagnostic workup to minimize any unexpected and unplanned for intraoperative finding.
Diagnostic biopsy and histologic results should be verified. A malignant diagnosis should be particularly noted in order to help determine the extent of the bowel resection and lymphadenectomy.
Documentation from preoperative endoscopy should be reviewed, particularly if the operative surgeon did not perform the procedure. The presence and location of a marking tattoo should be confirmed.
Preoperative imaging is used to help anticipate any involvement of the adjacent organs and the possible need for en bloc resection intraoperatively. Any need for additional technical assistance from other surgeons should be planned for.
In cases of perforation and anticipated significant intraperitoneal contamination that may render bowel anastomosis unsafe, plans should be made for ostomy marking and education preoperatively.
Preoperative bowel preparation, whether antimicrobial and mechanical, mechanical only, or no preparation, is a highly variable practice and is left to the discretion of the practicing surgeon.
Prophylactic intravenous antibiotics with coverage against gram-positive, gram-negative, and anaerobic flora of the skin and gut are typically administered prior to incision and continued for the first 24 hours.
Prophylaxis against deep venous thrombosis is typically administered prior to incision and during the hospital stay.
Positioning
Patients are usually placed in a supine position. If there is any possibility of extending the resection to the left colon or any possible need for intraoperative endoscopy, consideration should be given for placing the patient in lithotomy position.
TECHNIQUES
INCISION AND ABDOMINAL EXPLORATION
A midline incision extending from the epigastrium to below the umbilicus is made.
The abdominal cavity is explored for the presence of other pathology not identified by preoperative imaging. In cases of malignant disease, peritoneal lining, omentum, and hepatic and bowel surfaces are inspected and palpated for any evidence of metastatic disease. In women, the pelvic organs, including the ovaries, should be inspected. Any suspicious nodule should be biopsied for pathologic assessment as findings may affect the decision of proceeding to the remaining of the procedure.
OMENTUM DISSECTION AND EXPOSURE OF THE LESSER SAC
The relationship between the transverse colon pathology and the lesser sac is assessed.
Exposure to the lesser sac is gained in one of two ways, depending on whether omentectomy is performed or not.
If disease pathology does not necessitate en bloc omentectomy or if there is desire to preserve as much of the omentum as possible, then greater omentum is retracted cephalad and the transverse colon is retracted caudad. This reveals the avascular plane between the greater omentum and the transverse mesocolon (FIG 3). The pale yellow omental fat is distinguished from the fat of the appendices epiploicae of the transverse colon (FIG 4). As this plane is dissected, the greater omentum is freed from the transverse colon and mesocolon and entrance into the lesser sac is gained. This can be confirmed by visualization of the posterior wall of the stomach dorsally and of the anterior surfaces of the duodenum, pancreas, and transverse mesocolon ventrally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree