Transanal Endoscopic Microsurgery
Margaret V. Shields
John H Marks
DEFINITION
Transanal endoscopic microsurgery (TEM) is a minimally invasive technique that was originally developed by Dr. Gerhard Buess in 1983 to extend transanal access to benign and select malignant tumors. It is used to treat a variety of rectal lesions including benign adenoma, low-risk carcinoma, and more advanced cancers after neoadjuvant therapy.
This procedure is performed transanally with specially designed microsurgical instrumentation. This surgical approach is both a single-port surgery and a natural orifice transluminal endoscopic surgery (NOTES).
TEM is preferable over radical resection in select patients due to the ability to safely eradicate the disease with a wide full-thickness local excision while simultaneously sparing the morbidity of a major transabdominal surgery and preserving sphincter function.
DIFFERENTIAL DIAGNOSIS
Adenomas and other types of polypoid lesions found in the colon and rectum include hyperplastic polyps, serrated adenomas, flat adenomas, hamartomatous polyps, and inflammatory polyps.
Most colorectal cancers are adenocarcinomas (90% to 96%), but other rare malignancies include signet-ring cell carcinoma, squamous carcinoma, undifferentiated neoplasms, neuroendocrine tumors, gastrointestinal stromal tumors (GISTs), carcinoids, and melanoma.
PATIENT HISTORY AND PHYSICAL FINDINGS
The TEM procedure is primarily used to treat benign or malignant rectal lesions. In order to determine if TEM is the appropriate procedure for the patient, a full history and physical examination must be performed to evaluate both the general health of the patient and the extent of disease. Patients that are medically compromised may not be able to tolerate a radical procedure, making a local excision the only option.
Ideal candidates for TEM are patients with early, nonextensive tumors. This procedure can be used for patients in good health and is also a wonderful option for those who are medically compromised, as the approach is less invasive than radical abdominal surgery and extends the transanal approach up to the level of the rectosigmoid.
The fundamental objectives of rectal cancer management are complete tumor control and patient survival. However, perhaps in no other cancer are quality-of-life issues of such importance as the need for a permanent colostomy hangs in the balance.
There are several secondary goals that are desirable and must be considered when deciding upon the best treatment option for rectal cancer. These include preserving sphincter function, minimizing patient morbidity and mortality, minimizing patient trauma, maintaining bladder and sexual function, and avoiding a permanent colostomy. The primary goal of cancer control along with the secondary goals can be achieved with TEM surgery under appropriate conditions.
It is important to inquire about bowel habits, anal sphincter function, bladder and sexual function, past medical history, and past surgical history. It is important to discuss the genetic risk of colon cancer with the patient so that they can inform their relatives to get proper surveillance colonoscopy. Suspicious symptoms include change in bowel habits, rectal bleeding, rectal pain, or mucous discharge.
A thorough digital rectal exam is the single most important component of the preoperative evaluation for lesions in the bottom half of the rectum. The status of sphincter tone must always be checked as this impacts significantly on treatment decisions.
We recommend using both flexible sigmoidoscopy and rigid proctoscopy as part of the physical examination. Rigid proctoscopy offers a more accurate localization of the lesion’s position, whereas the flexible sigmoidoscope provides a much clearer image of the lesion. The most important tumor characteristics to evaluate are level in the rectum (from the anorectal ring and the anal verge), mobility/fixation, position of mass (midpoint), size of the tumor, circumference involvement, obstruction, ulceration, and the estimation of the clinical stage of disease.
IMAGING AND OTHER DIAGNOSTIC STUDIES
A full colonoscopy should be performed to assess the remainder of the rectum and the entire colon for potential synchronous lesions.
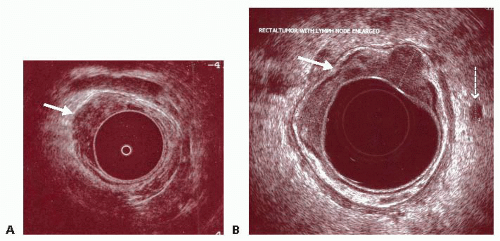
In malignancy, a computed tomography (CT) of the chest, abdomen, and pelvis along with serum testing for carcinoembryonic antigen (CEA) are obtained. Patients should also get an endoscopic rectal ultrasound (ERUS) to view the depth of invasion of the tumor and to evaluate for lymph node involvement (FIG 1). ERUS can predict mesorectal adenopathy (N status) with 70% accuracy and can assess depth of invasion (T status) in early stage rectal cancers with 90% accuracy. The ability to assess lymph node involvement is essential because it could be a cause of locoregional treatment failure.
Rectal protocol magnetic resonance imaging (MRI) is increasingly used in rectal cancer staging due to its ability to assess, in addition to T and N stages, potential adjacent
organ involvement and the relationship with the mesorectal margin (FIG 2). However, MRI, like ERUS, is challenged in trying to differentiate between T1 and T2 stages due to the limited resolution in delineating the layers of the rectal wall.
If the patient has a malignant lesion that is unfavorable (≥T3 or N +) at any level in the rectum or a favorable cancer in the distal one-third of the rectum (0.5 to 6.0 cm above the anorectal ring), neoadjuvant chemoradiation is recommended. Surgical decision making is based on the evaluation of the tumor at 8 to 12 weeks after completion of neoadjuvant chemoradiation in order to maximize the effect of tumor downstaging.
Table 1 summarizes the ideal TEM candidates as well as the absolute contraindications for TEM. In general, local excision is the preferred option for patients with adenoma, or cancer with favorable features (≤3 cm in diameter; T1, grade I or II, and no venous or lymphatic invasion; and no evidence of lymph node metastasis) after chemoradiation. An ideal patient for local excision has a tumor that is small, mobile, located in the distal rectum, and posteriorly based.
Contraindications for patients to undergo a TEM procedure after completion of neoadjuvant radiation include lymph node involvement, T3 or greater cancer after neoadjuvant chemoradiation, or tumors that remain fixed, deeply ulcerated, or have adjacent visceral organ involvement. In general, a maximum size of 4 cm is considered the limit for TEM after chemoradiation. Tumors greater than 3 to 4 cm in size can be challenging to excise transanally after neoadjuvant therapy due to the difficulty in closing the large defect that might be greater than one-half the circumference of the rectal wall.
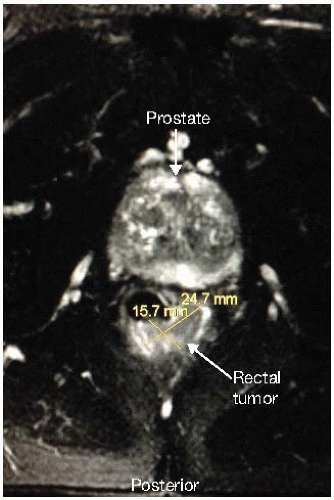 FIG 2 • Rectal-protocol MRI showing a rectal tumor involving the posterior and lateral rectal walls. There is a clear plane of separation from the prostate anteriorly, ruling out a T4 lesion. |
Table 1: Candidates and Contraindications for Transanal Endoscopic Microsurgery and Lymphovascular Invasion | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
SURGICAL MANAGEMENT
Preoperative Planning
Patient preparation for TEM is the same for benign or malignant lesions.
The patient will undergo standard bowel preparation.
Standard preoperative antibiotics are administered.
It is important to have a conversation with the patient preoperatively to discuss the potential need for laparoscopy or laparotomy and a possible diverting stoma.
Patient Positioning
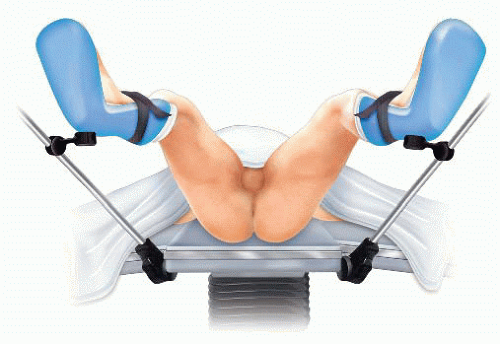
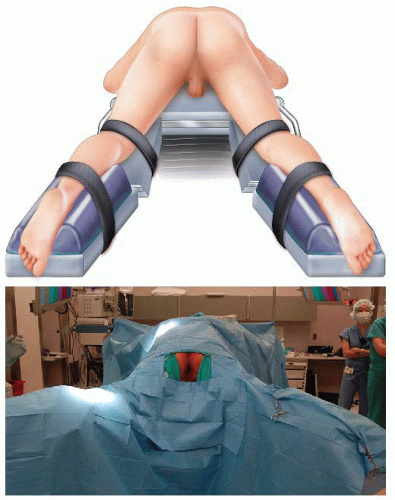
The positioning of the patient depends on the tumor location. In general, the patient is positioned so that the tumor is in the dependent position during the procedure.
The tumor should be at the center of the operating rectoscope throughout the procedure; the bevel of the TEM scope should face down at the tumor. This is essential as the optics reside in the upper portion of the operating proctoscope, limiting the reach of the instruments to the bottom 180 to 210 degrees of the lumen. Therefore, patient positioning becomes very important.
Operating Team Setup
The surgeon should be in a seated position in between the patient’s legs (FIG 5). The assistant should be seated to the left of the surgeon. The scrub nurse is to be positioned opposite the endosurgical unit. The monitors are placed in front of the surgeon.
TECHNIQUES
TRANSANAL ENDOSCOPIC MICROSURGERY SETUP
All of the instruments that we use during the TEM procedure are from the Richard Wolf TEM Instrument System. Some of the instruments used to do the dissection are displayed in FIG 6. However, similar instruments and equipment are offered by Karl Storz and others use standard laparoscopic instruments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree