Tracheostomy and Cricothyroidotomy
Tracheostomy is necessary when long-term access to the airway for ventilatory support or respiratory toilet is required. This chapter describes formal tracheostomy; percutaneous tracheostomy (Chapter 4) is an alternative in selected patients. Formal tracheostomy is best performed over a previously placed endotracheal tube in a fully equipped operating room where adequate lighting, electrocautery, and suction are available. Percutaneous tracheostomy may be performed at the bedside, generally in the intensive care unit, but requires the same attention to airway control as formal tracheostomy (see Chapter 4).
Steps in Procedure (TRACHEOSTOMY)
Position patient, check equipment, test balloon of tracheostomy tube
Identify five midline landmarks
Transverse or vertical incision centered just below cricoid cartilage
Divide tissues in midline
Retract or divide thyroid isthmus
Expose trachea and count rings down from cricoid
Incision between second and third ring
Pull back endotracheal tube slightly
Spread incision and insert tube
Confirm position of tube by passage of suction catheter; secure tube
Steps in Procedure (CRICOTHYROIDOTOMY)
Position patient, check equipment, check balloon of tracheostomy tube
Transverse incision over cricothyroid membrane
Control bleeding by manual pressure
Stab into membrane
Spread and insert tube, secure tube, pack wound to control oozing
Hallmark Anatomic Complications
Supraglottic tracheostomy
Tracheoinnominate artery fistula (delayed complication)
List of Structures
Larynx
Thyroid cartilage
Cricoid cartilage
Median cricothyroid ligament
Cricothyroid artery
Trachea
Landmarks
Mental protuberance
Hyoid bone
Laryngeal prominence
Manubrium sterni
Jugular (suprasternal) notch
Associated Structures
Thyroid gland
Isthmus
Pyramidal lobe
Anterior jugular vein
External jugular vein
Platysma muscle
Brachiocephalic (innominate) trunk
Brachiocephalic (innominate) vein
Jugular venous arch
Brachial plexus
Tracheostomy may also be required in an emergency when the patient cannot be intubated in the normal fashion (e.g., when massive facial trauma or edema precludes safe intubation). In this situation, cricothyroidotomy (see Fig. 3.8) can be performed more quickly and more safely than formal tracheostomy.
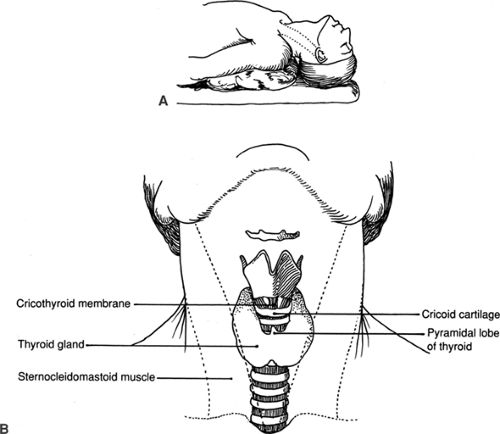
Positioning the Patient (Fig. 3.1)
Technical Points
Slightly hyperextend the neck by placing a small roll under the patient’s shoulders (Fig. 3.1A). If the roll is placed under the neck instead of the shoulders, a larger roll will be needed and the head may be elevated as well, thereby preventing the desired hyperextension. Do not hyperextend the neck in a patient with a known or suspected cervical spine injury because the resulting vertebral motion may cause irreversible damage to the spinal cord.
Select a tracheostomy tube appropriate to the size of the patient; for an average-sized adult, a number 7 or 8 tube will work well. Test the balloon and then deflate and lubricate it with sterile lubricant. Place the obturator inside the tube. Be sure that a soft rubber suction catheter is available on the sterile field for suctioning the tracheostomy after the tube is inserted.
Anatomic Points
The phrenic nerve arises from spinal cord levels C3 to C5, and the brachial plexus is derived from C5 to T1. Spinal cord damage at or above C3 will result in death secondary to paralysis of all respiratory muscles. Damage of the cord at levels involving the brachial plexus can result in quadriplegia. Hyperextension of the neck stretches the cord and may compress the cord against a damaged cervical vertebra; such a maneuver may also result in complete transection as the cord is caught between broken fragments of cervical vertebrae.
Landmark structures of this region are shown in Fig. 3.1B. The thyroid gland, often with a pyramidal lobe, overlies the trachea. The paired sternocleidomastoid muscles are located well lateral to it. The thyroid cartilage and cricoid cartilage are easily palpable above the thyroid gland. The hyoid bone can be palpated above the thyroid cartilage.
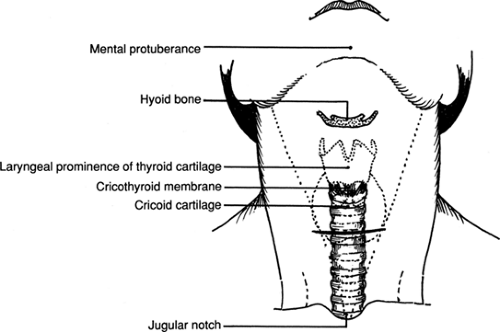
Identification of Landmarks (Fig. 3.2)
Technical and Anatomic Points
Palpate five midline landmarks, including the mental protuberance, or tip of the chin; the body of the hyoid bone; the laryngeal prominence of the thyroid cartilage (Adam’s apple); the cricoid cartilage; and the suprasternal or jugular notch of the manubrium sterni. All of these constant bony or cartilaginous landmarks should be identified with certainty to avoid inadvertent supraglottic incision. Repeated palpation of these readily identifiable midline structures will help ensure that the dissection remains in the midline.