Total Thyroidectomy
Saïd C. Azoury
Martha A. Zeiger
DEFINITION
Total thyroidectomy involves removal of all thyroid tissue, including both lobes and isthmus, while preserving the parathyroid glands, the recurrent laryngeal nerve (RLN), and the external branch of the superior laryngeal nerve.
ANATOMY
The thyroid gland typically weighs 20 g and has a right and left lobe bridged by a narrow isthmus.
The thyroid gland is located in the central compartment of the anterior neck below the thyroid cartilage.
The thyroid cartilage forms the laryngeal prominence or the “Adam’s apple.”
The thyroid lobes lie medial to the carotid sheaths and sternocleidomastoid muscles.
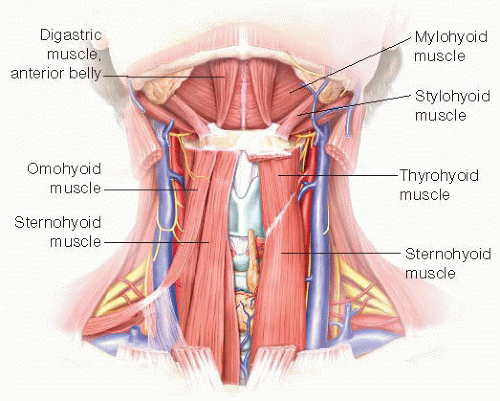
The anterolateral surface of the gland is covered by the sternothyroid and sternohyoid muscles (FIG 1).
The “thyroid sheath” is a connective tissue expansion of the pretracheal fascia and envelops the thyroid, condensing posteromedially into the ligament of Berry.
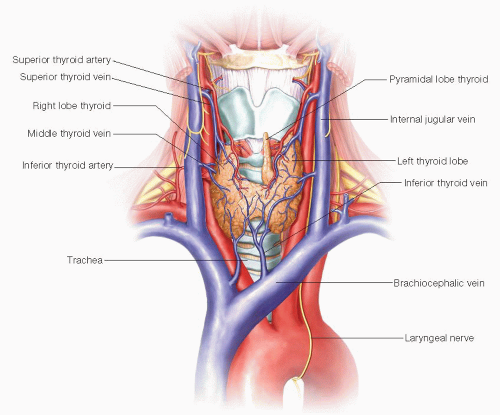
The thyroid gland receives its blood supply from the superior and inferior thyroid arteries.
The superior thyroid artery arises from the ipsilateral external carotid artery and the superior thyroid vein runs with the artery.
The middle thyroid vein drains into the ipsilateral internal jugular. The inferior thyroid artery originates from the thyrocervical trunk. The left RLN arises from the vagus at the level of the aortic arch and loops around the ligamentum arteriosum; the right RLN loops around the right subclavian artery (FIG 2).
The right RLN may be nonrecurrent in 0.5% to 1% of individuals.
The RLN innervates all the intrinsic muscles of the larynx except the cricothyroid muscles.
The internal branch of the superior laryngeal nerve is the sensory nerve for the supraglottic larynx. The external branch of the superior laryngeal nerve lies on the inferior pharyngeal constrictor muscle and descends alongside the superior thyroid vessels before innervating the cricothyroid muscle.
The superior parathyroid glands are generally located posterior to the superior thyroid lobe and the RLN. The inferior parathyroid locations are more variable but oftentimes are located anterior to the inferior thyroid lobes and RLN or on the inferolateral aspect of the lobes.
INDICATIONS FOR TOTAL THYROIDECTOMY
Thyroid Cancer
PATIENT HISTORY AND PHYSICAL FINDINGS
History
Thyroid cancer is more common in extremes of age, younger than 20 or older than 60 years.
Most thyroid nodules are asymptomatic, and most patients are euthyroid.
Thyroid nodules are more common in females, but there is a greater risk of malignancy in males.
One must inquire about a history of radiation therapy and family history of thyroid cancer: Nearly 90% of radiationassociated thyroid cancers are papillary.
Personal or family history of other endocrine disorders such as a history of thyroid cancer, primary hyperparathyroidism, pancreatic islet cell tumors, pituitary tumors, or adrenal tumors is essential to understand a patient’s risk.
Medullary thyroid cancer is a known component of multiple endocrine neoplasia 2 (MEN2).
Weight gain, fatigue, depression, constipation, dry skin, and brittle nails are symptoms of hypothyroidism; weight loss, weakness, anxiety, palpitations, and diarrhea are symptoms of hyperthyroidism; both are key elements of the review of systems portion of a history.
One should inquire about symptoms of dysphagia, dyspnea, voice change, cough, or trouble breathing.
Physical Exam
Size of thyroid nodules, firmness of the nodules, and the presence of substernal extension are important to assess.
Findings suggestive of cancer include nodule fixation, hard texture, and associated cervical lymphadenopathy.
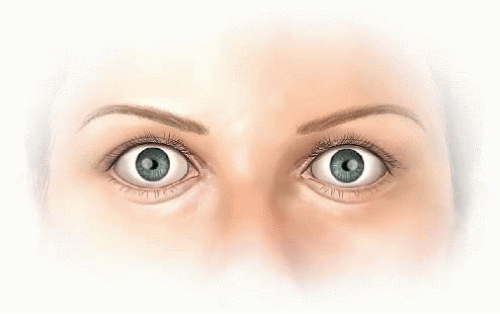
Important eye signs include stare, lid lag, dryness, diplopia, or exophthalmos (FIG 3); all of which can suggest Graves’ disease.
Extremities should be examined for pretibial myxedema (waxy, discolored induration, and swelling) that can be associated with severe hypothyroidism.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Thyroid-Stimulating Hormone (Normally 0.5 to 5 µU/mL)
A serum thyroid-stimulating hormone (TSH) should be measured to determine if the patient is hypo-, hyper-, or euthyroid. There is an inverse relationship between the free thyroxine (T4) level and the TSH concentration.
Free Thyroxine (Normally 12 to 28 pmol/L)
Free T4 is a sensitive and accurate measurement of biologically active thyroid hormone.
In early hyperthyroidism, total T4 levels are normal but free T4 levels are elevated.
Hyperfunctioning nodules are much less likely to harbor malignancy.
Fine Needle Aspiration Biopsy
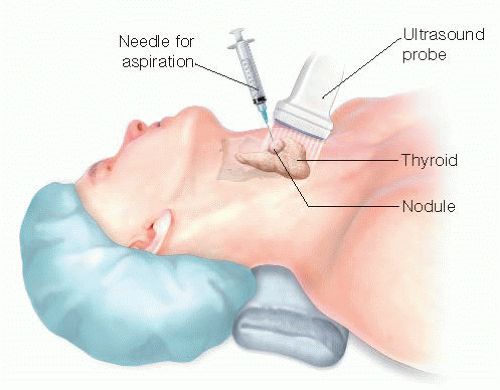
Ultrasound-guided needle aspiration is performed using 23- to 27-gauge needles and a 10-mL syringe (FIG 4).
FNAB specimens are classified as malignant, benign, indeterminate (atypical cells of undetermined significance, suspicious for follicular or Hürthle cell neoplasm, or suspicious for malignancy), or insufficient for diagnosis.
Overall sensitivity of FNAB is 95% to 98%.7
Iodine Scintigraphy
Elevated iodine uptake with diffuse uptake and enlargement is consistent with Graves’ disease.
The risk of malignancy in “hot” lesions is extremely low. Iodine scintigraphy should only be used if the patient is hyperthyroid and has nodular disease to determine if a nodule is responsible for the hyperthyroidism.
Antithyroglobulin and Antithyroid Peroxidase Antibodies
Anti-thyroid peroxidase (anti-TPO) antibodies are associated with Hashimoto’s thyroiditis. Antithyroglobulin (anti-Tg), if present, makes following patients with thyroid cancer for Tg elevation unreliable.
High-Resolution Ultrasonography
Ultrasound is recommended to determine the number, size, and characteristics of the thyroid nodules.
Increased intranodular vascularity, irregular margins, the so-called “halo sign” or anechoic rim, microcalcifications, and hypoechogenicity are generally associated with a malignancy.
Cervical ultrasound to assess for lymphadenopathy is recommended for suspicious or malignant thyroid nodules.
Computed Tomography
Computed tomography (CT) imaging is indicated for substernal goiters or if a cancer is large or appears fixed to surrounding anatomic structures.
NONOPERATIVE MANAGEMENT
Antithyroid Drugs: Propylthiouracil and Methimazole
When used for Graves’ Disease, generally, propylthiouracil (PTU) (100 to 300 mg three times daily) or methimazole (10 to 30 mg three times daily) are the antithyroid drugs of choice.
Both drugs inhibit the organic binding of iodine and thyroperoxidase coupling of iodotyrosines. PTU also inhibits the peripheral conversion of T4 to triiodothyronine (T3).
Radioactive Iodine Therapy
Radioiodine therapy has been the preferred treatment for most patients with Graves’ disease.
Radioiodine therapy is indicated postoperatively for patients with thyroid cancer who have a high risk of recurrence.
Close Follow-up
Patients with asymptomatic and benign thyroid nodules should be followed with serial neck ultrasounds and repeat fine needle aspiration (FNA) as needed.
Patients may need longitudinal neck ultrasounds and repeat FNA.
SURGICAL MANAGEMENT
The use of total thyroidectomy for benign disease has increased over the last 15 years in the United States from 17.6% (1993-1997) to 39.6% (2003-2007) compared with 82.4% and 60.4% for partial thyroidectomy over the same periods.11
Total thyroidectomy for Graves’ is the gold standard advocated by endocrine surgeons.
In one study of patients with Graves’ disease, reasons for having thyroid surgery were persistent disease despite medical therapy (46.6%), patient preference (24.1%), MNG/cold nodules (20.3%), failed radioactive iodine (RAI) treatment (16%), and ophthalmopathy (12.1 %).12
In general, the indication for total thyroidectomy should be considered in cases of suspicious or definite malignant nodules; the presence of thyroid nodules; and a history of head and neck irradiation, Graves’ disease, large or substernal goiter, or symptomatic goiter (dysphagia, pressure, dyspnea).
The most important goals of surgery for MNG are to prevent recurrence after surgery and to definitively diagnose thyroid nodules that were indeterminate or suspicious preoperatively.
The advantage of total thyroidectomy, compared to subtotal thyroidectomy, for treatment of Graves’ is the avoidance of recurrent hyperthyroidism, which has been reported to be as high as 22% following subtotal thyroidectomy.7,13,14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree