Total Abdominal Colectomy: Open Technique
Tarik Sammour
Andrew G. Hill
DEFINITION
Total abdominal colectomy is defined as the removal of the entire colon, following which the distal ileum is anastomosed to the rectum or an end ileostomy is created.
DIFFERENTIAL DIAGNOSIS
Inflammatory bowel disease (IBD)
Severe acute colitis (various etiologies)
Polyposis syndromes, including familial adenomatous polyposis (FAP) and hereditary nonpolyposis colorectal cancer (HNPCC)
Slow-transit constipation
Malignancy
PATIENT HISTORY AND PHYSICAL FINDINGS
Specific history and examination findings will depend on the indication for total abdominal colectomy.
History of previous abdominal surgery is important, particularly in the setting of IBD. If the patient has had multiple small bowel resections and is at risk of short-gut syndrome, then total abdominal colectomy is contraindicated.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Endoscopy: Colonoscopy is required to diagnose the disease for which total colectomy is required, and an up-to-date flexible sigmoidoscopy is needed to assess the state of the rectum and ensure it is disease/polyp-free.
Patients with IBD also require small bowel imaging (preferably computed tomography [CT] or magnetic resonance imaging [MRI] enteroclysis) to ensure that the small bowel is free of diseased segments.
Patients with severe constipation require a colonic transit study to confirm functional colonic disease.
Patients with malignancy require a staging CT scan of the chest/abdomen/pelvis.
SURGICAL MANAGEMENT
Preoperative Planning
The surgeon obtains informed consent from the patient, explaining the procedure, expected recovery, and risks and benefits of the operation. Consent should also be obtained for a stoma should this be required.
The patient’s nutritional status should be optimized prior to surgery.
A suitably qualified nurse should carry out preoperative stoma marking.
Blood crossmatching is performed (at least two units available).
A preoperative sodium phosphate enema is administered.
A midthoracic epidural should be inserted preoperatively.3
An indwelling Foley catheter is inserted preoperatively.
Appropriate intravenous antibiotic prophylaxis is given on induction.4
Consideration should be given to intravenous steroid supplementation if the patient is steroid-dependent.
Subcutaneous low-molecular-weight heparin is given on induction.
Calf compression stockings are applied.
Note: Mechanical bowel preparation is not recommended.5
Positioning
The patient should be placed on a supine position with the arms out. Ensure that the arms are not hyperabducted to avoid brachial plexopathy.
The patient should be as far down the bed as possible (to provide access to the anus). Ensure that the buttocks remain well supported on the bed.
The legs should be placed in lithotomy braces with adequate padding. Ensure that there is no pressure on the common peroneal nerves bilaterally.
A strap should be placed across the pelvis to hold the patient on the bed.
Once the patient is positioned, a digital rectal examination and proctoscopy should be performed to ensure that there is no rectal abnormality.
The patient’s skin is prepped and draped from the xiphisternum to the pubis, ensuring access to the anus.
The surgeon stands on the patient’s left side, and the first assistant stands on the opposite side.
TECHNIQUES
INCISION AND ACCESS
A generous midline laparotomy is performed.
A suitable laparotomy retractor is inserted.
After general inspection, the small bowel is packed with moist, large swab packs into the upper abdominal cavity.
ASCENDING COLON MOBILIZATION
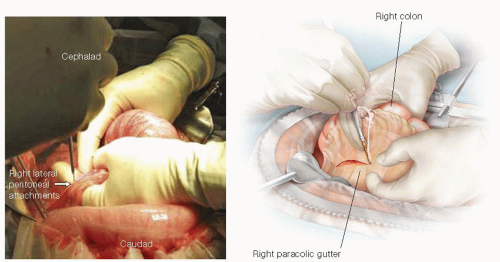
The ascending colon is mobilized by medial traction and dissection along the right paracolic gutter using diathermy (FIG 1).
Care is taken to identify, and avoid damage to, the right gonadal vessels, the right ureter, and the duodenum.
TRANSVERSE COLON MOBILIZATION
The hepatic flexure is mobilized by dividing adhesions between the gallbladder and liver. Gentle traction on the hepatocolic ligament exposes the hepatocolic ligament, which is then transected with electrocautery (FIG 2).
The gastrocolic ligament is exposed as the assistant retracts the greater omentum superiorly while the surgeon retracts the transverse colon anteroinferiorly.
Diathermy is used to separate the greater omentum from the anterior leaf of the transverse mesocolon.
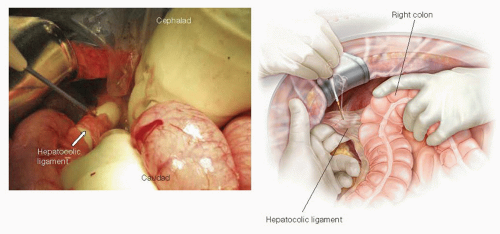
FIG 2 • Hepatic flexure mobilization. Gentle traction on the hepatic flexure of the colon exposes the hepatocolic ligament, which is then transected with electrocautery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree