Total Abdominal Colectomy: Laparoscopic Technique
Matthew G. Mutch
DEFINITION
Total abdominal colectomy (TAC) is the removal of the abdominal colon, which extends from the cecum to the top of the rectum. The upper rectum is an intraperitoneal structure and the top of the rectum can be identified as the point where the teniae coli splay out. After resection, an end ileostomy or ileorectal anastomosis can be created. The determination to perform an ileostomy versus an anastomosis is based on the diagnosis and indication for the resection.
PATIENT HISTORY AND PHYSICAL FINDINGS
There are several indications for a laparoscopic TAC:
Ulcerative colitis or Crohn’s colitis
Refractory to medical management
Complications
Acute colitis
Stricture
Perforation
Dysplasia
Neoplasm
Colon cancer
Synchronous cancers
Colon cancer in a patient younger than age 40 years
Familial adenomatous polyposis (FAP) with rectal sparing
Colonic inertia
A thorough history and physical examination are necessary prior to surgery. Prior abdominal surgery is not an absolute contraindication for the laparoscopic approach.
In colitis patients, the extent of medical management is dependent on previous regimens with immunomodulators and response to intravenous steroids. Typically, failure to respond after 7 days of intravenous steroids is considered failure of medical management.
Patients with acute colitis can be safely approached laparoscopically. However, if they have peritonitis or are showing signs of hemodynamic instability, the laparoscopic approach should not be attempted.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Each indication for surgery has unique or specific evaluations that are necessary to determine the optimal treatment.
Acute colitis
Endoscopic examination of the colon is necessary to confirm the diagnosis.
For patients that are hospitalized for acute colitis, stool cultures to rule out Clostridium difficile and cytomegalovirus (CMV) infections are very helpful.
Colon cancer
Pathologic confirmation of adenocarcinoma is necessary.
Review of the colonoscopy report to confirm the number and locations of the lesions. Ideally, the lesion(s) are tattooed with a vital dye to mark the location. It is best to inject the ink distal to the most distal lesion and in at least three different locations around the circumference of the lumen.
Preoperative staging is completed with a computed tomography scan of the chest, abdomen, and pelvis and a serum carcinoembryonic antigen (CEA) level.
Patients younger than age 50 years and/or with a strong family history of colorectal cancer should be considered for genetic counseling.
FAP
Endoscopy and pathology: confirming the presence of more than 100 adenomatous polyps
Genetic testing confirming the diagnosis of FAP is desirable, but not all patients with endoscopic findings consistent with FAP will have an identifiable mutation.
If the patient is going to be considered for a rectal sparing procedure, the rectum needs to be examined and cleared of all polyps. If there are 10 or fewer polyps in the rectum that can be removed or destroyed, rectal sparing can be considered.
Colonic inertia
Normal bowel function ranges from three bowel movements a day to one bowel movement every 3 days. These patients give a long history of constipation that is no longer responsive to laxatives. When the patient gets to the point where his or her abdominal complaints and bowel function are not responsive to laxatives and their symptoms become intolerable, surgery management should be considered.
A total colon exam is necessary to rule out a mechanical cause of the patient’s constipation.
A colonic transit study is necessary to confirm the diagnosis of colonic inertia. The patient ingests a capsule with 25 radiopaque markers and the patient is not allowed to use laxatives during examination period. Plain abdominal x-rays are obtained 3 and 5 days after ingestion. An abnormal exam is when five or more markers are retained in the colon after 5 days. The distribution of the markers is the diagnostic key: Markers scattered throughout the colon are consistent with colonic inertia, whereas accumulation of the markers in the rectum or distal sigmoid colon are suggestive of obstructed defecation.
Patients should also be evaluated with either a video defecography or dynamic magnetic resonance imaging (MRI) to evaluate for obstructive defecation. If a patient demonstrates evidence of obstructive defecation, they should undergo biofeedback prior to discussing surgery as a definitive treatment option.
SURGICAL MANAGEMENT
Preoperative Planning
Depending on the operative plan, patients should be marked for a diverting or end ileostomy. The patient needs to be assessed in the supine, sitting, and standing positions. The stoma should rest on the apex of skin fold and be of adequate distance from bony prominences, skin creases, and the waistline of their pants. The stoma should be brought through the rectus muscle to minimize the risk of developing a parastomal hernia.
The use of ureteral stents is left to the discretion of the surgeon.
Positioning
A mechanical bed that is able to place the patient in the extremes of position is necessary.
The patient is secured to the bed with either a beanbag, a nonslip pad, shoulder braces, or foam pads.
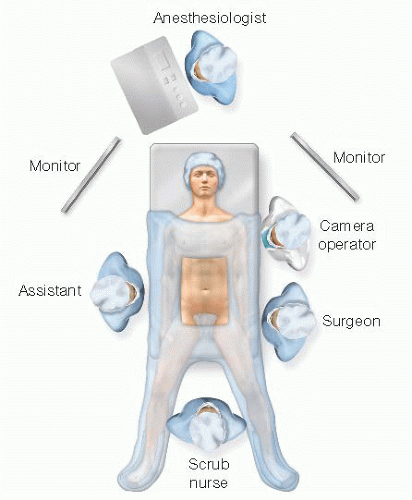
The patient should be placed in the modified lithotomy position with Allen or Yellofin stirrups (FIG 1). This allows access between the legs to assist with mobilization of the left colon and to the perineum for the anastomosis.
Both arms are tucked to the patient’s side with the thumbs facing up. This allows the surgeon, assistant, and camera driver plenty of room to maneuver during the case.
A monitor should be placed off the patient’s right shoulder during the mobilization of the right and transverse colon.
A monitor should be placed off the patients left shoulder for the mobilization of the left colon and splenic flexure.
TECHNIQUES
PORT PLACEMENT AND TEAM SETUP
There are several options for port placement and they depend on whether a total laparoscopic surgery or handassisted laparoscopic surgery (HALS) is going to be used.
Straight laparoscopic approach
Camera port—The port is placed in the periumbilical area in equal distance between the xiphoid process and the pubic symphysis (FIG 2A). The camera should be placed at the apex of the pneumoperitoneum so the widest field of view can be obtained.

FIG 2 • Port placement. A. Port placement for a conventional laparoscopic total colectomy. B. Port placement for a hand-assisted laparoscopic total colectomy.
HALS approach
Hand port—The hand port is placed in the suprapubic position via either a midline or Pfannenstiel incision (FIG 2B).
Camera port—The camera is placed in the supraumbilical position so that the port does not interfere with skirt of the hand port.
Working ports—There is one working port placed on the right and left sides. They are placed in equal distance between the hand port and the camera and lateral to the rectum muscle.
Team setup
For the HALS approach to the right and transverse colon, the surgeon stands on the patient’s left side with his or her left hand placed in the hand port and with his or her right hand on the energy source.
During the mobilization of the left colon, the surgeon stands on the patient’s right side, right hand in the abdomen and left hand on the energy source (FIG 3). The camera operator stands to the head side of the surgeon.
The operative steps described in the chapter are the same whether the procedure is being performed straight laparoscopically or as HALS. For the purpose of this chapter, the HALS approach to the total colectomy operation will be described.
MOBILIZATION OF THE RIGHT COLON
Once the abdomen has been accessed and inspected, the patient is placed in steep Trendelenburg position to pack the small bowel in the right upper quadrant (RUQ). The posterior approach will be described for the mobilization of the right colon. The specific steps of operation are the same for medial to lateral, lateral to medial, and superior to inferior, but the order of the steps is different depending on the approach.
The goals of the operation are to access the retroperitoneal plane, identify and sweep the duodenum out of the way, mobilize the right colon mesentery, divide the lateral attachments and omentum, and ligate the vasculature.
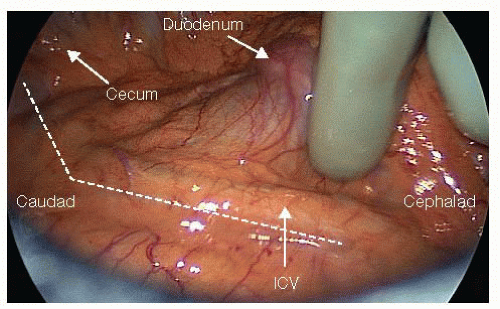
For the posterior approach, the small bowel is placed in the RUQ and the base of the ascending colon mesentery is exposed from the third portion of the duodenum to the cecum (FIG 4). The ileocolic vessels (ICV) are seen as they cross over the third portion of the duodenum. The patient is not tilted so that the small bowel will stay in the RUQ.
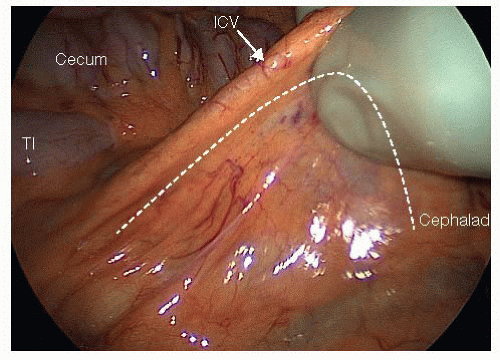
The middle finger and thumb grasp the ICV off the retroperitoneum. The index finger then sweeps under the mesentery to expose the third portion of the duodenum (FIG 5). The peritoneum is then scored dorsal to the ICV from the duodenum all the way down to the cecum.
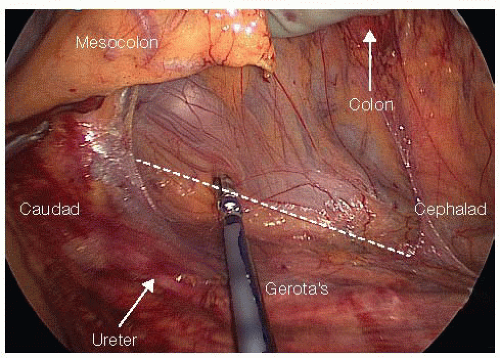
Once the retroperitoneum is accessed, the duodenum is identified and swept posteriorly. After the retroperitoneum has been accessed, the hand is placed under
the mesentery, palm down, and the ascending colon mesentery is elevated off the retroperitoneum (FIG 6) through a medial to lateral dissection approach. The retroperitoneum is bluntly swept down with an energy device.
This medial to lateral dissection is carried out beyond the colon from the midtransverse colon, out to the hepatic flexure, and down the ascending colon to the cecum. The more extensively the dissection can be carried laterally, the easier the lateral dissection will be.
Tension is the key to facilitating an easy dissection as this is an avascular plane than can be effortlessly dissected with adequate tension. The motion should almost be a swimming-type motion in which tension is created, the tissue is swept down, tension is recreated, and the tissue is swept down, over and over.
Now all that remains is the lateral attachments, which are transected with an energy device up along the right gutter (FIG 7). At this point, the patient is in airplane position with the right side up so the small bowel will fall to the left upper quadrant (LUQ). This exposes the lateral attachments of the right colon and the hepatic flexure.
At this point, the hand may get in the way so it can be removed and instruments can be passed through the hand port. With a grasper in the right hand, the cecum is grasped and retracted medially, and the energy source in the left hand is passed through the hand port.
Once the cecum is adequately mobilized, the hand is placed back into the abdomen. The left hand is placed under the right colon mesentery and lateral to the colon to expose the lateral attachments, which are divided under tension by the first assistant.
The right colon and its mesentery are elevated to expose the retroperitoneum and dissect any remaining retroperitoneal attachments. This dissection is carried all the way up to the hepatic flexure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree