Thyroidectomy for Substernal Goiters
Andrew G. Shuman
Ashok R. Shaha
DEFINITION
A goiter refers to any abnormal thyroid enlargement secondary to nutritional deficiency, endocrine disease, or neoplasm. In general terms, substernal goiter applies to conditions in which the majority of the thyroid volume lies below the thoracic inlet.
PATIENT HISTORY AND PHYSICAL FINDINGS
A comprehensive medical history is obligatory, including assessment of the indications for surgery, consideration of medical comorbidities, and ensuring that patients are medically optimized and risk-stratified for surgery. Any prior operative records and pathology reports should be reviewed in advance.
A detailed physical examination is mandatory, including consideration of upper airway patency and visualization of the larynx to assess vocal fold mobility.
Flexible fiberoptic laryngoscopy is helpful in evaluating glottic function and assessing the airway.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Cross-sectional imaging (usually computerized tomography) is invaluable in defining the intrathoracic anatomic extent of the mass and its relationship to critical cervical and intrathoracic structures.1
Intravenous contrast may delay the ability to use radioactive iodine but should be used whenever anatomic considerations may affect the surgical planning or technique.
Ultrasound may also be employed but is of limited use in assessing the intrathoracic extent of disease.
A thoughtful approach to the airway is necessary. In addition to history, physical examination, and imaging studies, exclusion of cardiopulmonary factors affecting respiration is important.
Spirometry and flow-volume loops are useful adjuncts in order to understand the underlying respiratory physiology. However, surgical decisions are made based on functional and anatomic considerations rather than strictly physiologic tests.
Preoperative laboratory studies should include thyroid function testing and thyroglobulin.
In the case of a thyroid mass or nodule, fine needle aspiration (preferably image-guided) with cytologic evaluation should be attempted prior to surgery.
SURGICAL MANAGEMENT
Consideration for removal of substernal goiters is multifactorial.2
Indications for an operation may relate to the need to make a diagnosis, extirpate malignancy, ameliorate compression of the upper aerodigestive tract, or relieve venous outflow obstruction (superior vena cava syndrome).
In most patients meeting criteria for surgery, medical options other than watchful waiting are limited.
Given that most goiter operations are elective, prudent and deliberate preoperative planning and counseling are essential. The indications, risks, benefits, and alternatives of surgery versus expectant management should be discussed.
Preoperative Planning
Preoperative communication with anesthesia is critical. Although most patients can be readily intubated, airway compression or deviation must be considered. Atraumatic intubation is necessary.3
The endotracheal tube cuff should be well below the vocal folds to avoid both glottic trauma and inadvertent extubation, as the endotracheal tube has a tendency to be displaced with movement during surgery.
Thoracic surgeons should provide preoperative input and be available to assist in cases in which their presence may be needed.
Options such as small endotracheal tubes, endotracheal tubes facilitating nerve monitoring, and/or fiberoptic bronchoscopy/intubation should be discussed prior to induction with anesthesia.
Fiberoptic intubation is rarely necessary, although adjunctive technologies, such as the GlideScope®, may be useful.
Positioning
The patient is positioned supine with gentle neck extension. Effort should be made to prepare and drape in a manner that facilitates some movement of the head and neck while preserving the sterile field.
Overextension of the neck may put the recurrent laryngeal nerves (RLNs) under tension and make them more difficult to identify.
Even if sternotomy is not planned, the chest should be prepped for access in case of either an emergency or the inability to free the gland transcervically.
Anatomy
The tuberculum of Zuckerkandl is a posterolateral prominence of thyroid tissue that frequently approximates the location of the RLN.4
Berry’s ligament is a condensation of the pretracheal fascia that attaches the thyroid to the airway. Small vessels run along the ligament, and it may be in close proximity to the RLN, requiring careful attention in order to ensure preservation of the nerve when the thyroid is being mobilized.
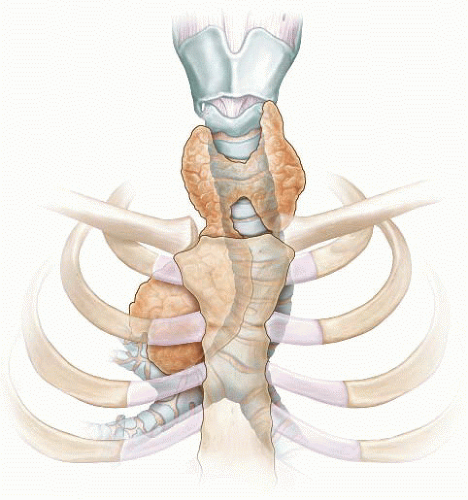
In general, the substernal component of the thyroid gland originates from one lobe. Left substernal goiters are anteriorly displaced by the aortic arch. Right substernal goiters are frequently nestled between the superior vena cava and the prevertebral muscles (FIG 1).
Posterior mediastinal goiters are rare, but when present, the RLN may be anteriorly displaced.
In rare cases, substernal goiters may not be contiguous with the cervical thyroid gland.
Approach
The cervical vascular supply, anterior position, and rarity of bilateral intrathoracic extension typically facilitate complete removal of substernal goiters transcervically.5
Less than 10% of substernal goiters require sternotomy or thoracotomy.
Relative indications for sternotomy include the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree