Thyroid Lobectomy
Samuel M. Maurice
Geeta Lal
The thyroid gland is composed of two lobes (right and left) connected by a midline isthmus and a variable pyramidal lobe. It is purple-pink in color, and the normal gland weighs approximately 20 g. The isthmus lies inferior to the cricoid cartilage, whereas the lobes extend superiorly over the lateral aspects of the thyroid cartilage. The gland extends from approximately C5 to T1. The thyroid gland is closely associated with the external branch of the superior laryngeal nerve, the recurrent laryngeal nerve, and the parathyroid glands. Success in thyroid surgery requires careful and meticulous dissection and hemostasis, which aids in the identification and preservation of these vital structures.
Steps in Procedure
Beach chair position, with neck extended and roll between scapulae
Incision 1 cm caudal to cricoid cartilage
Raise flaps in subplatysmal plane
Incise midline and mobilize strap muscles
Mobilize thyroid gland medially and divide middle thyroid vein
Mobilize superior pole and divide vessels on thyroid
Ligate inferior pole structures, working from medial to lateral
Identify recurrent laryngeal nerve
Identify and mobilize parathyroid glands
Skeletonize and divide branches of inferior thyroid artery directly on thyroid
Divide ligament of Berry
Mobilize pyramidal lobe, if present
For lobectomy, clamp and ligate isthmus on contralateral side
For total thyroidectomy, mobilize contralateral lobe as previously described
For subtotal lobectomy, leave approximately 4 g remnant posteriorly
Reapproximate strap muscles and platysma
Close incision without drainage
Hallmark Anatomic Complications
Injury to recurrent laryngeal nerve
Injury to superior laryngeal nerve
Hypoparathyroidism
Bleeding
List of Structures
Thyroid Gland and Associated Structures
Thyroid gland
Left and right lobes
Isthmus
Pyramidal lobe
Parathyroid glands
Superior parathyroid glands
Inferior parathyroid glands
Nerves
Vagus nerve (CN X)
Facial nerve (CN VII)
Spinal accessory nerve (CN XI)
Recurrent laryngeal nerve
Superior laryngeal nerve
External branch
Internal branch
Ansa cervicalis
Muscles
Platysma
Strap muscles
Sternohyoid muscle
Sternothyroid muscle
Thyrohyoid muscle
Omohyoid muscle
Sternocleidomastoid muscle
Vessels
External jugular vein
Anterior jugular vein
Jugular venous arch
Internal jugular vein
Common carotid artery
External carotid artery
Internal carotid artery
Superior thyroid vein
Middle thyroid vein
Inferior thyroid vein
Thyrocervical trunk
Superior thyroid artery
Inferior thyroid artery
Thyroid ima artery
Landmarks
Trachea
Thyroid cartilage
Cricoid cartilage
Sternal notch
Esophagus
Pretracheal fascia
Ligament of Berry
Hyoid bone
Tubercle of Zuckerkandl
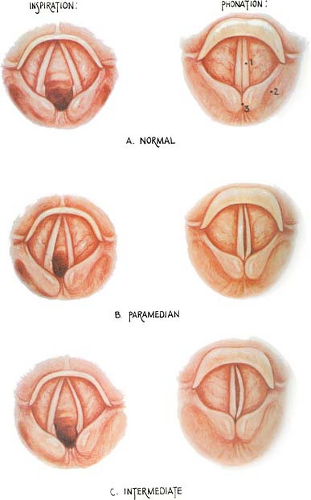
Preoperative Preparation (Fig. 6.1)
Technical Points
Patients should be suitable candidates for general anesthesia. Prepare hyperthyroid patients with antithyroid medications, beta-blockers, and Lugol’s iodine or supersaturated potassium iodide solution (sometimes steroids are also added) to avoid thyroid storm. Patients with medullary thyroid cancer or concerning symptoms should be screened for pheochromocytoma. Documentation of vocal cord function by direct or indirect laryngoscopy is paramount in those already suspected of having vocal cord dysfunction (i.e., those with prior neck surgery or altered phonation), because bilateral injury may lead to airway obstruction.
Anatomic Points
Recurrent laryngeal nerve injury generally results in the ipsilateral vocal cord lying in a paramedian position. Injury to both the external branch of the superior laryngeal nerve and the recurrent laryngeal nerve causes the vocal cord to lie in an intermediate position, as shown in Fig. 6.1.
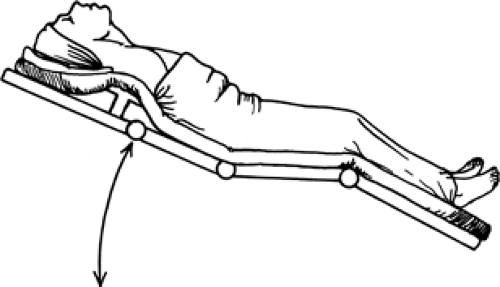
Patient Positioning (Fig. 6.2)
Technical Points
Position the patient supine. Keeping the patient in a “beach-chair” position, with a moderate reverse Trendelenburg and with the knees flexed, will help reduce venous pressure. Place a sandbag or roll between the scapulae allowing the shoulders to fall backward. Extend the neck and place the head on a donut cushion. The use of silk suture to secure the drapes helps in maintaining a sterile field, but is not absolutely necessary.
Anatomic Points
Proper positioning displaces the thyroid anteriorly and superiorly, allowing for an easier dissection. Suboptimal positioning translates into inadequate exposure and may result in a larger incision.
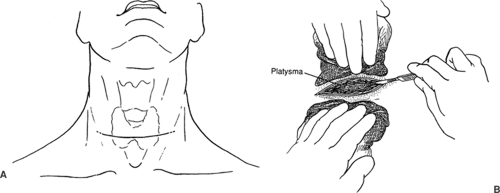
Choice of Skin Incision (Fig. 6.3)
Technical Points
Make a Kocher transverse collar incision in a natural skin crease approximately 1 cm below the cricoid cartilage. A 2-0 silk suture may be pressed against the skin to mark out the planned course of the incision. Take care to measure the distance on each side of the midline to ensure symmetry. A 4- to 5-cm incision is generally adequate; however, patients with a short neck, large thyroid gland, or limited neck extension may require a longer incision. Carry this incision through the skin, subcutaneous tissues, and the platysma. It is generally easier to identify the fibers of the platysma along the lateral aspect of the incision.
Anatomic Points
An incision 1 cm caudal to the cricoid cartilage generally places the incision over the thyroid isthmus. The platysma arises in the superficial fascia of the neck and is continuous with the fascia that covers the pectoralis major and deltoid muscles. It is a sheetlike muscle that extends from the mandible or subcutaneous tissues of the face to the clavicles. Its fibers decussate over the chin and become continuous with the facial musculature. As a muscle of facial expression, it is innervated by the seventh cranial nerve.
Raising Skin Flaps (Fig. 6.4)
Technical Points
Raise flaps in the subplatysmal plane. Place straight Kelly clamps, skin hooks, or rake retractors on the dermis to elevate the flaps anteriorly. Provide countertraction with a finger or gauze as the flaps are elevated both sharply with electrocautery or a scalpel and bluntly with a finger or Kitner. Extend this elevation superiorly to the level of the thyroid cartilage and inferiorly to the level of the suprasternal notch. Take care not to injure the superficial network of veins that lie beneath the platysma. This often extensive collection of veins, including the paired anterior jugular veins, external jugular veins, and communicating veins, lies beneath the platysma muscle overlying the sternocleidomastoid and midline strap muscles. Place towels along the skin edges to protect them, and a use a self-retaining retractor to aid in exposure.
Anatomic Points
Elevating subplatysmal flaps takes advantage of an avascular plane that lies between the platysma and underlying superficial
veins and strap muscles. The muscles encountered during thyroid surgery become apparent after mobilization of the subplatysmal flaps. These include the two sternocleidomastoid muscles and the paired strap muscles (sternohyoid, sternothyroid, thyrohyoid, and omohyoid muscles). The sternocleidomastoid muscles mark the lateral boundaries of the dissection. The sternocleidomastoid muscle has two muscle bellies, both inserting onto the mastoid process with dual origins, on the sternum and proximal clavicle. The sternocleidomastoid muscle is innervated by the spinal accessory nerve (CN XI). The omohyoid muscle inserts on the hyoid bone and originates from the scapula. Only the superior belly is generally encountered. The sternohyoid muscles lie in the midline overlying the sternothyroid and thyrohyoid muscles. The sternohyoid originates from the sternum and inserts on the hyoid bone. The sternothyroid extends from the sternum to the thyroid cartilage, and the thyrohyoid muscle extends from the thyroid cartilage to the hyoid bone.
veins and strap muscles. The muscles encountered during thyroid surgery become apparent after mobilization of the subplatysmal flaps. These include the two sternocleidomastoid muscles and the paired strap muscles (sternohyoid, sternothyroid, thyrohyoid, and omohyoid muscles). The sternocleidomastoid muscles mark the lateral boundaries of the dissection. The sternocleidomastoid muscle has two muscle bellies, both inserting onto the mastoid process with dual origins, on the sternum and proximal clavicle. The sternocleidomastoid muscle is innervated by the spinal accessory nerve (CN XI). The omohyoid muscle inserts on the hyoid bone and originates from the scapula. Only the superior belly is generally encountered. The sternohyoid muscles lie in the midline overlying the sternothyroid and thyrohyoid muscles. The sternohyoid originates from the sternum and inserts on the hyoid bone. The sternothyroid extends from the sternum to the thyroid cartilage, and the thyrohyoid muscle extends from the thyroid cartilage to the hyoid bone.
The superficial jugular veins lie just beneath the platysma. The paired external jugular veins are lateral and overlie the sternocleidomastoid muscles. The paired anterior jugular veins directly overlie the sternohyoid muscles. There is often an extensive network of communicating veins connecting the anterior jugular veins and external jugular veins. The jugular venous arch, a communication between the right and left anterior jugular veins, is often seen in the lower part of the neck and may have to be ligated and divided to provide optimal exposure and separation of the strap muscles. Although ligation of these veins is of little clinical consequence, identification and avoidance of these vessels is often possible.
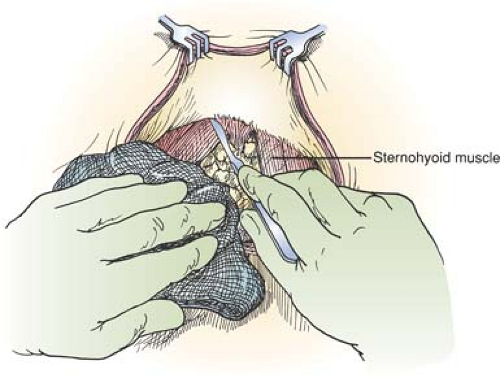
Division/Mobilization of Strap Muscles (Fig. 6.5)
Technical Points
Identify the whitish-colored midline raphe between the paired strap muscles. Separate the paired sternohyoid and sternothyroid muscles in the midline from the sternal notch to the thyroid cartilage to expose the underlying thyroid gland. On the side to be approached first, bluntly dissect the sternohyoid muscle from the deeper sternothyroid muscle lying just beneath it. This step often assists with exposure, particularly when working via smaller incisions. Identify and preserve the ansa cervicalis as it courses over the lateral aspect of the sternothyroid if possible. The strap muscles rarely require division to gain exposure to the thyroid gland, particularly in large goiters. In the rare occasion that division is necessary, divide the muscles as high as possible to preserve the strap muscles’ innervation by the ansa cervicalis. These muscles can then be sutured together at the end of the operation. If tumor directly invades into the strap muscles, resect the strap muscle en bloc with the underlying thyroid tissue. Then dissect the sternothyroid muscle off the thyroid bluntly. Identify the internal jugular vein by gently retracting laterally on the sternocleidomastoid muscle.