Thyroglossal Duct Cyst
In this section, the anatomy of the upper midline of the neck is explored, and the embryology of the thyroid gland and associated anomalies is discussed through the operation of removal of thyroglossal duct cyst.
Thyroglossal duct cysts form along the path of descent of the thyroid gland. They present as upper midline neck masses. Often, these cysts become infected and present as abscesses. Incision and drainage or simple excision of the cyst results in a high recurrence rate. Complete removal of the cyst and its associated tract is necessary for cure.
SCORE™, the Surgical Council on Resident Education, has classified surgery for thyroglossal duct cyst as a “COMPLEX” Pediatric Surgical procedure.
STEPS IN PROCEDURE
Position patient: Neck hyperextended, lower face, and mouth draped into field
Transverse incision (include sinus tract if present)
Retract sternohyoid muscles and expose cysts
Dissect cyst free of surrounding tissues medially, laterally, cephalad, and caudad
Seek and dissect fibrous tract leading to hyoid bone
Trace to hyoid and resect midportion of hyoid bone in continuity with tract
Follow tract to base of tongue, using pressure on foramen cecum if necessary; ligate termination
HALLMARK ANATOMIC COMPLICATION
Recurrence resulting from inadequate dissection
LIST OF STRUCTURES
Embryologic Structures and Terms
Thyroid anlagen
Pharyngeal arches
Tuberculum impar (pharyngeal arch I)
Copula (pharyngeal arches II through IV)
Thyroglossal duct
Adult Structures
Tongue
Foramen cecum
Hyoid bone
Suprahyoid muscles
Mylohyoid muscle
Geniohyoid muscle
Sternohyoid muscle
Genioglossus muscle
Hypoglossal nerve (XII)
Mandibular division of trigeminal nerve (V)
Mylohyoid nerve
Lingual nerve
Thyroid gland
Pyramidal lobe
Thyroid cartilage
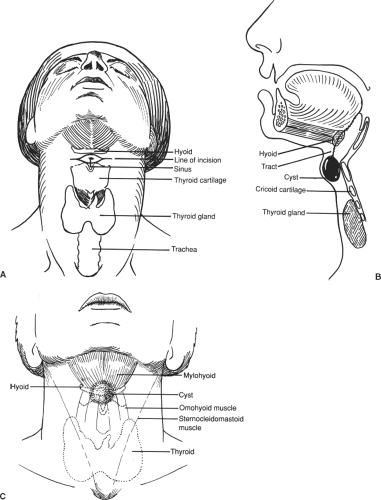
Positioning the Patient and Incising the Skin (Fig. 5.1)
Technical Points
Position the patient supine with the neck hyperextended and the chin directly anterior. Include the lower face and lips in the surgical field. (Access to the mouth may facilitate subsequent dissection.)
Make a transverse skin incision over the cyst (Fig. 5.1A). If previous drainage of the cyst resulted in an external sinus tract or scar, excise this in transverse elliptical fashion with the skin incision. Plan the incision to lie parallel to, or within, the natural skin lines. Elevate flaps in the plane deep to the platysma muscle to expose the deep cervical fascia and paired sternohyoid muscles overlying the cyst. Incise this fascia in the midline.
Anatomic Points
Thyroid anlagen begin as an epithelial thickening of endodermal origin during the fourth intrauterine week. This thickening
is located in the floor of pharyngeal arch II, between the tuberculum impar (pharyngeal arch I) and copula (arches II through IV) that participate in the formation of the tongue. The anlage rapidly evaginates, coming into contact with the aortic sac of the developing heart. Owing to differential growth, the thyroid migrates from its point of origin, marked by the foramen cecum of the mature tongue (at the junction of the anterior two-thirds and posterior one-third), to its definitive location. During this migration, the gland is connected to the tongue by the thyroglossal duct (Fig. 5.1B). The path of migration passes anterior to the developing hyoid bone, whose paired anlagen, from pharyngeal arch II, fuse in the ventral midline
and also undergo some rotation. Because of the relationship of the thyroglossal duct to the developing hyoid bone, the duct can be drawn posterocranially with respect to the hyoid, be enveloped in hyoid periosteum or hyoid bone proper, or pass posterior to the hyoid. Typically, the duct degenerates, leaving a short diverticulum at the foramen cecum proximally, a longer cord distally that develops into the pyramidal lobe of the thyroid gland (typically displaced slightly to the left of the median plane), and an intervening fibrous cord. If the discontinuous epithelial cells present in the fibrous remnant differentiate and subsequently assume a secretory function, a thyroglossal duct cyst results.
is located in the floor of pharyngeal arch II, between the tuberculum impar (pharyngeal arch I) and copula (arches II through IV) that participate in the formation of the tongue. The anlage rapidly evaginates, coming into contact with the aortic sac of the developing heart. Owing to differential growth, the thyroid migrates from its point of origin, marked by the foramen cecum of the mature tongue (at the junction of the anterior two-thirds and posterior one-third), to its definitive location. During this migration, the gland is connected to the tongue by the thyroglossal duct (Fig. 5.1B). The path of migration passes anterior to the developing hyoid bone, whose paired anlagen, from pharyngeal arch II, fuse in the ventral midline
and also undergo some rotation. Because of the relationship of the thyroglossal duct to the developing hyoid bone, the duct can be drawn posterocranially with respect to the hyoid, be enveloped in hyoid periosteum or hyoid bone proper, or pass posterior to the hyoid. Typically, the duct degenerates, leaving a short diverticulum at the foramen cecum proximally, a longer cord distally that develops into the pyramidal lobe of the thyroid gland (typically displaced slightly to the left of the median plane), and an intervening fibrous cord. If the discontinuous epithelial cells present in the fibrous remnant differentiate and subsequently assume a secretory function, a thyroglossal duct cyst results.
A thyroglossal duct cyst should be suspected in any person presenting with a median or paramedian lump in the neck, especially if the lump is superior to the level of the cricoid cartilage and if it moves with the excursion of the hyoid bone during swallowing or tongue protrusion (Fig. 5.1C). A lingual thyroid, usually the result of maldescent of the thyroid, has to be considered if the lump is located intralingually. In this case, preoperative evaluation with a radioisotope scan is essential because 65% to 75% of patients with this condition lack other thyroid tissues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree