Thymic Carcinoma
Key Facts
Clinical Issues
Generally poor prognosis
High-grade tumors have median survival of 18 months
Usual sites of metastases include lymph nodes, bone, lung, pleura, liver, and brain
Macroscopic Features
Commonly contain areas of hemorrhage and necrosis
Usually invasive, unencapsulated, and poorly circumscribed
Cystic degeneration can be seen in some subtypes (basaloid, mucoepidermoid)
Microscopic Pathology
Closely resembles other types of carcinoma
Well-differentiated squamous cell carcinoma of thymus
Basaloid carcinoma
Mucoepidermoid carcinoma
Poorly differentiated, nonkeratinizing (lymphoepithelioma-like) carcinoma
Adenocarcinoma of thymus
Papillary carcinoma
Clear cell carcinoma
Spindle cell (sarcomatoid) carcinoma
Carcinosarcoma
Anaplastic carcinoma
Top Differential Diagnoses
Atypical thymoma (WHO type B3)
Metastatic carcinoma of lung
Metastatic carcinoma from other organs
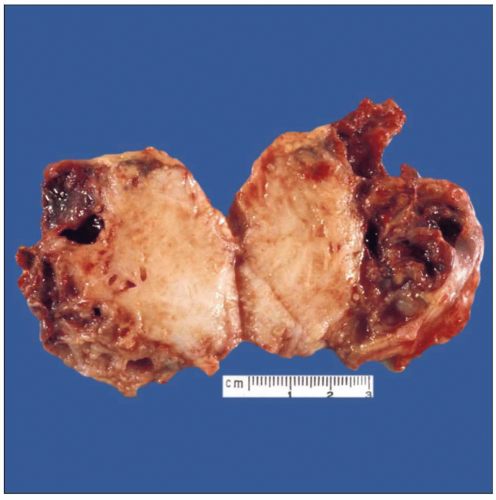 Gross appearance of squamous cell carcinoma of the thymus shows solid tumor surrounded by areas of hemorrhage, necrosis, and cystic degeneration. |
TERMINOLOGY
Abbreviations
Thymic carcinoma (TC)
Synonyms
Malignant thymoma type II
WHO type C thymoma
Poorly differentiated (high-grade) thymic epithelial neoplasm
Definitions
Primary thymic epithelial neoplasm showing overt cytologic features of malignancy with loss of organotypical features of thymic differentiation
ETIOLOGY/PATHOGENESIS
Pathogenesis
Unknown
Some cases may arise from malignant degeneration of preexisting thymoma
CLINICAL ISSUES
Epidemiology
Incidence
Extremely rare neoplasm; accounts for less than 1% of thymic tumors
Age
Affects all age groups but is most frequent between 30-60 years of age
Gender
Slight male predilection (M:F = 1.5:1)
Presentation
Incidental finding in small subset of cases
Anorexia
Weight loss
Chest pain
Shortness of breath
Paraneoplastic syndromes are not seen
Natural History
Highly aggressive neoplasm; generally refractory to treatment
Treatment
Options, risks, complications
Treatment related to grade and stage
Surgical approaches
Surgical resection may be curative for low-grade, encapsulated lesions
Surgical excision may be indicated in larger tumors for debulking or palliation of symptoms
Adjuvant therapy
Radiation and chemotherapy are used in high-grade or high-stage tumors
Prognosis
Generally poor prognosis.
High-grade tumors have median survival of 18 months
Usual sites of metastases include lymph nodes, bone, lung, pleura, liver, and brain
IMAGE FINDINGS
General Features
Lobulated, marginated, anterior mediastinal mass
Radiographic Findings
Calcification in 10-40% of cases
Obscuring of mediastinal fat plane
Extension to pericardium and pleura
Extrathymic metastases often present
Invasion into great vessels and mediastinal structures seen in about 40% of cases
MACROSCOPIC FEATURES
General Features
Commonly contain areas of hemorrhage and necrosis
Usually invasive, unencapsulated, and poorly circumscribed
Cystic degeneration can be seen in some subtypes (basaloid, mucoepidermoid)
Sections to Be Submitted
Sections should include tumor with capsule (1 per cm of greatest diameter) as well as infiltrating margins and any included lymph nodes or surrounding structures
MICROSCOPIC PATHOLOGY
Histologic Features
Well-differentiated squamous cell carcinoma of thymus
Identical histologic features to squamous cell carcinoma arising at other locations
Must 1st rule out metastasis from other organ or occult primary site
Stage-by-stage has better prognosis than squamous cell carcinoma of lung with massive mediastinal compromise
Basaloid carcinoma
Small hyperchromatic round to oval tumor cells with prominent peripheral palisading of nuclei
Often associated with cystic changes; tumor cells can be tracked to lining of cysts
Usually associated with low-grade behavior but can also metastasize distantly
Mucoepidermoid carcinoma
Admixture of squamous, intermediate, and mucinous cells with cribriform cystic spaces filled with mucin
Mucinous cysts and individual mucocytes are highlighted by mucicarmine stains
Frequently associated with cystic changes of thymus
Most cases are well differentiated; however, moderate and poorly differentiated variants also exist and are associated with more aggressive behavior
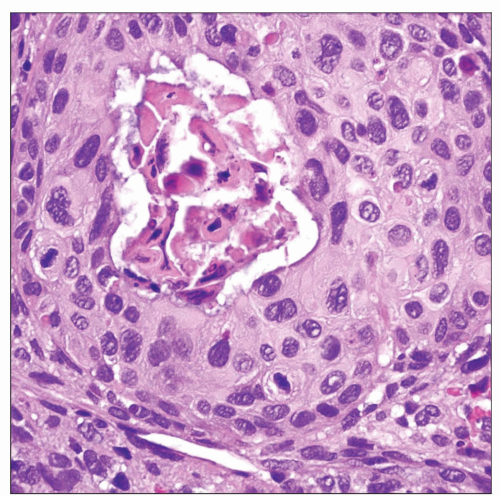
Poorly differentiated, nonkeratinizing (lymphoepithelioma-like) carcinoma
Most frequent type of thymic carcinoma in Western patients
Poorly differentiated tumor cells with large hyperchromatic nuclei with prominent eosinophilic nucleoli and frequent mitotic figures; resembles poorly differentiated carcinoma (lymphoepithelioma) of nasopharynx
Large tumor cell islands characterized by central comedo-like areas of necrosis
Some cases are characterized by dense lymphoplasmacellular stromal infiltrates; others are devoid of lymphoid stroma
Can often show admixtures with areas of spindle cell thymoma (WHO type A)
Some cases in children and adolescents may be associated with Epstein-Barr virus
Adenosquamous carcinoma
Biphasic glandular and squamous components
High-grade tumor usually associated with poor prognosis
May harbor “myoid” cell component (“rhabdomyomatous carcinoma of thymus”)
Adenocarcinoma of thymus
Very rare variant (few cases reported)
May be of mucinous and nonmucinous type; mucinous variant resembles “colloid carcinoma” in other organs
Metastasis from distant or occult primary must be stringently ruled out before making this diagnosis
Papillary carcinoma
Very rare type; very few cases reported in literature
Often associated with areas of spindle cell thymoma (WHO type A)
Papillary areas may display very low-grade cytologic features
Clear cell carcinoma
Characterized by large cells with abundant clear cytoplasm
Can display very aggressive behavior
Most cases represent secondary clear cell changes in squamous cell carcinoma
Care must be taken to exclude metastasis from clear cell carcinoma of lung, kidney, adrenal, or other organs
Spindle cell (sarcomatoid) carcinoma
Composed of highly atypical spindle epithelial cells with high nuclear grade and brisk mitotic activity
Majority are seen in association with preexisting areas of spindle cell thymoma (WHO type A)
Aggressive behavior with frequent distant metastases
Carcinosarcoma
True mixed tumor with both malignant epithelial (carcinomatous) component and malignant sarcomatous component
Most frequent sarcomatous component is rhabdomyosarcoma; most frequent carcinomatous component is poorly differentiated adenocarcinoma
Highly aggressive tumor with high mortality
Anaplastic carcinoma
Bizarre tumor cells with marked nuclear atypia and abnormal mitotic figures
Diagnosis of exclusion: Needs demonstration of epithelial lineage of tumor cells by either immunohistochemistry or electron microscopy
Rare foci of differentiated squamous carcinoma or adenocarcinoma can be occasionally identified
Highly aggressive behavior
Neuroendocrine carcinoma
Well, moderately, or poorly differentiated types
Other rare types of thymic carcinoma
Rhabdoid carcinoma of thymus: Characterized by eccentric globular eosinophilic cytoplasmic inclusions
Hepatoid carcinoma of thymus: Tumor cells resemble hepatocytes
Desmoplastic carcinoma of thymus: Characterized by prominent desmoplastic stroma entrapping squamoid elements
Predominant Cell/Compartment Type
Epithelial
Grade
Low-grade and high-grade types, depending on degree of cytologic atypia, mitotic activity, and amount of necrosis
ANCILLARY TESTS
Cytology
As screening tool to confirm presence of malignant cells
Frozen Sections
To confirm presence of cytologic atypia, mitotic activity, and necrosis; not for definitive diagnosis
Cytogenetics
Several nonrecurrent chromosomal losses and gains have been reported but are not useful for diagnosis or prognosis
DIFFERENTIAL DIAGNOSIS
Atypical Thymoma (WHO Type B3)
May be difficult to distinguish from low-grade, well-differentiated squamous cell carcinoma of thymus
Should not show marked cytologic atypia or overt features of malignancy
Contains perivascular spaces and immature T lymphocytes
Usually lacks vascular invasion and necrosis
Metastatic Carcinoma of Lung
Well-differentiated squamous cell carcinoma of lung can metastasize massively to mediastinal lymph nodes
Bronchoscopy with bilateral bronchial brushings and washings are necessary to rule out primary bronchial squamous cell carcinoma
Immunohistochemical stains for TTF-1 may be helpful for identifying pulmonary metastases of adenocarcinoma
Metastatic Carcinoma from Other Organs
Carcinomas in mediastinum are statistically more likely to represent metastases from other organs rather than primary tumors of thymus
Thorough clinical and radiographic examination is required to rule out possibility of occult or late metastasis from distant primary before rendering diagnosis of thymic carcinoma
DIAGNOSTIC CHECKLIST
Clinically Relevant Pathologic Features
Thymic carcinoma is diagnosis of exclusion
There are no pathognomonic features that can permit a pathologist to make this diagnosis based on histology because tumors resemble carcinomas from other organs
Demonstration of absence of tumor elsewhere is required for definitive diagnosis
Pathologic Interpretation Pearls
Islands of poorly differentiated cells with central comedo-like areas of necrosis characterize poorly differentiated nonkeratinizing (lymphoepithelioma-like) squamous cell carcinoma
Cases showing areas of transition with well-differentiated or atypical thymoma can be seen in a significant number of cases
SELECTED REFERENCES
1. Marchevsky AM et al: Thymic epithelial neoplasms: a review of current concepts using an evidence-based pathology approach. Hematol Oncol Clin North Am. 22(3):543-62, 2008
2. Moran CA et al: Thymic carcinoma: current concepts and histologic features. Hematol Oncol Clin North Am. 22(3):393-407, 2008
3. Rajan A et al: Treatment of advanced thymoma and thymic carcinoma. Curr Treat Options Oncol. 9(4-6):277-87, 2008
4. Rieker RJ et al: An institutional study on thymomas and thymic carcinomas: experience in 77 patients. Thorac Cardiovasc Surg. 56(3):143-7, 2008
5. Suster S et al: Histologic classification of thymoma: the World Health Organization and beyond. Hematol Oncol Clin North Am. 22(3):381-92, 2008
6. Ra SH et al: Mucinous adenocarcinomas of the thymus: report of 2 cases and review of the literature. Am J Surg Pathol. 31(9):1330-6, 2007
7. Nakagawa K et al: Immunohistochemical KIT (CD117) expression in thymic epithelial tumors. Chest. 128(1):140-4, 2005
8. Suster S: Thymic carcinoma: update of current diagnostic criteria and histologic types. Semin Diagn Pathol. 22(3):198-212, 2005
9. Chalabreysse L et al: Thymic carcinoma: a clinicopathological and immunohistological study of 19 cases. Histopathology. 44(4):367-74, 2004
10. Pan CC et al: KIT (CD117) is frequently overexpressed in thymic carcinomas but is absent in thymomas. J Pathol. 202(3):375-81, 2004
11. Choi WW et al: Adenocarcinoma of the thymus: report of two cases, including a previously undescribed mucinous subtype. Am J Surg Pathol. 27(1):124-30, 2003
12. Pan CC et al: Expression of calretinin and other mesothelioma-related markers in thymic carcinoma and thymoma. Hum Pathol. 34(11):1155-62, 2003
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree