Thoracoscopic Lobectomy or Segmentectomy
Kemp H. Kernstine Sr.
Thoracoscopic lobectomy or other anatomic thoracoscopic lung resections are performed as described for the other thoracoscopic procedures (see Chapter 27). Where we once allowed an extra 30 to 60 minutes for a thoracoscopic approach, it now routinely requires less than 2 to 3 hours for a thoracoscopic lobectomy. The learning curve is significant and these procedures should only be attempted by an experienced thoracoscopic surgeon. Ideal minimally invasive lobectomy patients are those with tumor diameters less than 3 cm, tumors that do not involve the hilar vessels or mainstem bronchi on computed tomography, and minimal hilar scarring and nodal disease. In patients with significant adhesions, poor visibility, and chest wall or hilar-invading tumors, the open thoracotomy technique should be used for resection. For patients with hilar lesions who potentially might require a pneumonectomy, we prefer to perform an open thoracotomy to determine the need for a pneumonectomy or sleeve lobectomy.
SCORE™, the Surgical Council on Resident Education, classified partial pulmonary resection, open or thoracoscopic, as a “COMPLEX” procedure.
STEPS IN PROCEDURE
Three to five thoracoports may be required
Identify venous drainage first
Ascertain that venous drainage to the rest of the lung is normal
Dissect vein free, close to pericardium
Pass a silk tie around the vein for retraction and then divide the vein with an endoscopic linear stapler
The order in which the major structures are taken varies according to lobe:
Right upper lobe:
Take the vein
Then take the arterial branches and the bronchus
Right middle and lower lobe:
Take the vein
Then the bronchus and pulmonary artery branches
Left upper lobe:
Take the vein
Then the upper pulmonary artery branches
Take the bronchus directly adjacent to the lower lobe pulmonary artery
Avoid taking the left mainstem bronchus deeper in the hilum/mediastinum Then take remaining pulmonary artery branches
Left lower lobe:
Take the vein
Then take the superior segment pulmonary artery branch, the bronchus, and then the basilar segment artery branches.
Perform associated lymphadenectomy at this point
Identify the bronchus to the segment of lung to be resected
Visualize the bronchus through the endotracheal tube
Note transillumination of segment that is being resected
Close but do not fire the stapler
Have the anesthesiologist inflate the lung, confirming that the segment to be resected does not inflate and deflate, but the rest of the lung does
Resect with adjacent nodal tissue
For lobectomy or segmentectomy, place a flexible drain or 28- to 32-French chest tube to the apex
HALLMARK ANATOMIC COMPLICATIONS
Injury to pulmonary artery
Injury to pulmonary vein
Division of wrong bronchus
Air leak
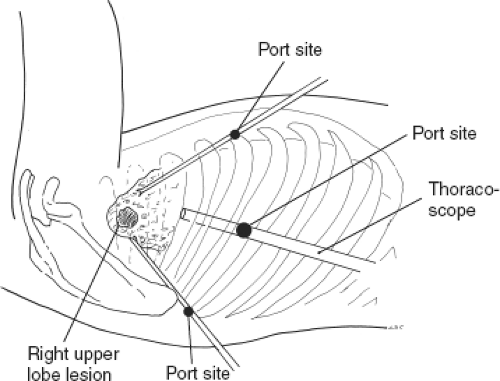
Port Placement (Fig. 30.1)
Technical and Anatomic Points
For the complete thoracoscopic approach, typically, five ports are required. Alternatively, the axillary port (which can be extended to 4 to 5 cm for the “access” incision) and one to three additional thoracoport incisions may be used. However, in spite of the complete thoracoscopic approach, the axillary insicion will likely still need to be extended to allow for the removal of the specimen.
We prefer to perform the completely thoracoscopic approach and place two posterior ports that are used for retraction and three anterior ports for dissection and visualization, although any of the ports can be used for dissection, retraction, or visualization. The three anterior ports are placed along the anterior axillary line; the first is a video port placed at the sixth to seventh intercostal space and the second in the midchest level. The third and most superior port is placed at the axillary hairline, typically at the second to third intercostal space. It is through this port that the specimen will be delivered, as stated, the port site that may need to be enlarged. The two posterior ports are placed 10 to 15 cm apart and are in the line of the middle distance between the posterior portion of the scapula and the posterior spinous processes. For upper lobes, these posterior ports are somewhat higher than for inferior lobes. After the ports are placed, any of them can be used for video examination or dissection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree