Thoracic Outlet Decompression
M. Victoria Gerken
Phillip C. Camp Jr.
First rib resection for thoracic outlet decompression remains a controversial solution to a complex problem. The term thoracic outlet syndrome refers to a variety of symptoms usually neurologic but is on occasion vascular and that results from any of a number of anatomic situations. Most patients with thoracic outlet syndrome improve significantly with physical therapy and repetitive behavior avoidance. Only a small number of patients require surgical intervention. When such intervention is indicated, resection of the first rib is the most common approach, but is not the only possible procedure. Some authors recommend subperiosteal resection of the first rib in order to reduce the risk for injury to the neurovascular contents; however, leaving the periosteum intact can lead to reformation of a rudimentary rib, which can cause recurrence of the symptoms. In this chapter, complete resection of the first rib and its periosteum is described. For further discussion of the etiology and treatment of this complex condition, the reader is referred to the references. This uncommon procedure is included because it illustrates regional anatomy well.
SCORE™, the Surgical Council on Resident Education, classified thoracic outlet decompression as a “COMPLEX” procedure.
STEPS IN PROCEDURE
Lateral decubitus position, arm supported at 90-degree angle from torso
Skin incision just inferior to axillary hairline from pectoralis major to latissimus dorsi muscles
Dissect down to chest wall, identifying and protecting intercostobrachial nerves
Gently displace axillary contents from thoracic outlet
Identify anterior scalene muscle (between axillary vein and artery) and divide it
Identify subclavius tendon anterior to axillary vein and divide it
Identify first rib and divide intercostal muscle from it
Resect first rib anteriorly at costal cartilage and posteriorly close to transverse process
Smooth edges of resected rib
Divide any residual connection between anterior scalene muscle and middle scalene muscle
Check hemostasis, check for pleural entry
Close incision in layers without drains
HALLMARK ANATOMIC COMPLICATIONS
Injury to axillary vein
Injury to long thoracic nerve
Injury to phrenic nerve
Injury to intercostobrachial nerve
LIST OF STRUCTURES
Anterior axillary fold
Posterior axillary fold
Pectoralis major muscle
Latissimus dorsi muscle
Serratus anterior muscle
Anterior scalene muscle
Middle scalene muscle
Posterior scalene muscle
Smallest scalene muscle
Subclavius muscle
Intercostal muscles
Intercostobrachial nerve
Medial brachial cutaneous nerve
Long thoracic nerve
Phrenic nerve
Brachial plexus
Axillary vein
Subclavian vein
Internal jugular vein
Cervical fascia
Sibson’s fascia
Carotid sheath
Sympathetic trunk
Axillary artery
Thyrocervical Trunk
Suprascapular artery
Transverse cervical artery
Thoracic duct
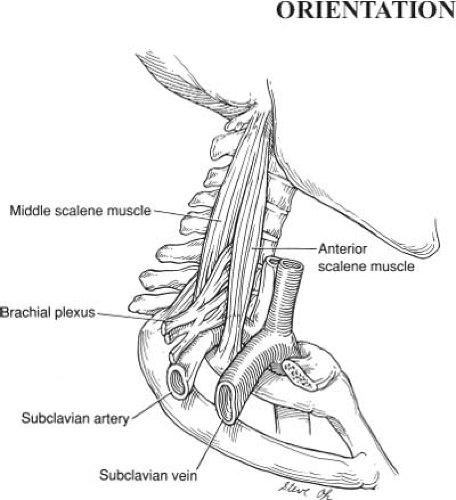
The brachial plexus and subclavian artery pass between the anterior and middle scalene muscles, the subclavian vein passes between the anterior scalene muscle and the first rib (Fig. 31.1). Any of these three crucial structures are vulnerable to compression. Unfortunately, simple excision of the anterior scalene muscle generally fails to solve the problem and the wider decompression afforded by first rib resection is generally required.
Position of the Patient and Skin Incision (Fig. 31.2)
Technical Points
Place the patient in the lateral decubitus position, as for standard thoracotomy. Your assistant should support the superior arm at a 90-degree angle from the torso. Flex the patient’s arm at the elbow to make it easier for the assistant to support it comfortably. Allow the assistant to relax the position of the arm periodically during the case to prevent undue stress to its neurovascular supply (and to the assistant).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree