Learning Objectives
Learn the role of blood gases in the evaluation of the patient with pulmonary disease.
Understand how pleural fluid analysis is used in the diagnosis of pulmonary disorders.
Understand how bronchoalveolar lavage can aid in the diagnosis of respiratory disease.
Recognize the different laboratory tests used for assessing fetal lung maturity.
Approach to the Patient With Pulmonary Disease
Impaired exchange of gases is the unifying theme of respiratory disorders (Figure 14–1). Although they do not play a significant role in the diagnosis of specific pulmonary diseases, blood gas and electrolyte measurements (see Chapter 2 for blood gas determinations) are commonly used to assess the severity of different pulmonary abnormalities. The analysis of fluid located in the pleural space, which collects with certain abnormalities, constitutes another battery of tests often useful in the evaluation of pulmonary diseases. Careful analysis of respiratory secretions along with accompanying white blood cells, immune mediators, and foreign pathogens through bronchoalveolar lavage (BAL) aids in the diagnosis and management of lung disease. Infections in the respiratory tract are a major cause of pulmonary disorders. These are nearly always diagnosed using clinical laboratory tests (respiratory infections are discussed in Chapter 5). This chapter begins with a discussion of laboratory tests utilized in the diagnosis and monitoring of respiratory diseases and is followed by a section describing the most common lung diseases—asthma, respiratory distress syndrome (RDS) in adults and neonates, chronic obstructive pulmonary disease (COPD), and lung cancer.
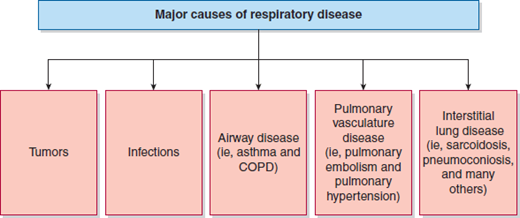
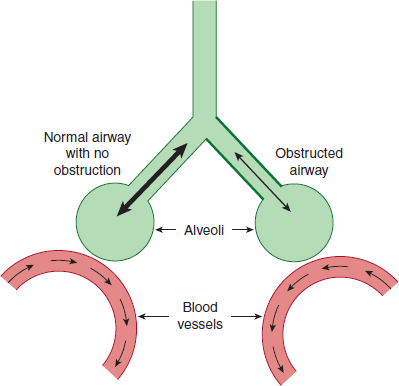
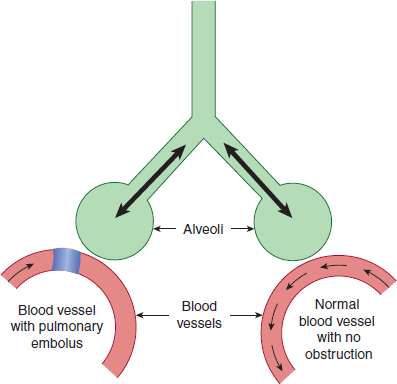
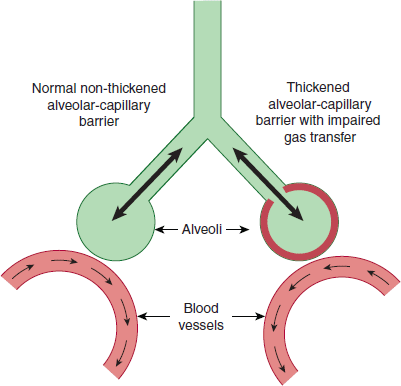
Pulmonary disorders other than infections and tumors can be classified into 3 major groups. One group of disorders includes emphysema, bronchitis, asthma, and RDS. These are airway-based (bronchial) diseases. Inflammation or damage to the bronchi results in impaired ventilation of alveoli (Figure 14–2). Another group of disorders affects the blood vessels, and, thereby, blood flow in the lung. Pulmonary vascular diseases are associated with reduced blood flow, resulting in nonuniform perfusion of the lungs (Figure 14–3). The third major group of pulmonary diseases is the interstitial lung disorders, which affect the tissue and space around the alveoli. These are a heterogeneous group of disorders associated with lung tissue damage due to scarring or inflammation. Damaged lung tissue is unable to fully expand, leading to thickening of the interface between alveoli and adjacent capillaries resulting in impaired diffusion of gases (Figure 14–4).
Clinical progression of pulmonary disease can lead to life-threatening respiratory failure. Acute RDS is a rapid-onset disease associated with severe breathing problems resulting from multiple insults to the lung (see more information below). It is distinct from “end-stage lung,” which is the result of a chronic pulmonary disorder.
Blood Gases and Blood pH
Many disorders are associated with abnormalities in arterial blood pO2, pCO2, and pH. While these tests are not themselves diagnostic, they are valuable in assessment of the severity of respiratory diseases. The blood gas test panel includes:
pO2 or partial pressure of oxygen
pCO2 or partial pressure of carbon dioxide
pH
The functional abnormalities most commonly detected with this battery of tests are:
Low pO2 (hypoxemia or low O2 in blood, as opposed to hypoxia, which is reduced O2 in tissues)
High pCO2 (hypercapnia)
Low arterial blood pH with a primary respiratory cause (respiratory acidosis from an increased arterial pCO2)
Low arterial blood pH with a primary metabolic cause (metabolic acidosis, usually from increased acid production and/or impaired renal H+ elimination, resulting in a decreased arterial HCO3−)
High arterial blood pH with a primary respiratory cause (respiratory alkalosis from a decreased arterial pCO2)
High arterial blood pH with a primary metabolic cause (metabolic alkalosis from an increased arterial HCO3−)
The lungs respond within minutes to acid–base disturbances by 1) eliminating CO2 (hyperventilation) to increase blood pH or 2) retaining CO2 (hypoventilation) to decrease the pH.
The lungs respond within minutes to acid–base disturbances by 1) eliminating CO2 (hyperventilation) to increase blood pH or 2) retaining CO2 (hypoventilation) to decrease the pH. The kidney has the ability to 1) excrete H+ and retain HCO3− to increase pH or 2) retain H+ and excrete HCO3− to lower blood pH. However, renal compensation is slow and occurs over hours to days. Table 14–1 lists selected respiratory and nonrespiratory disorders associated with hypoxemia, and Table 14–2 presents selected respiratory and nonrespiratory disorders that can result in acid–base abnormalities.
| Disorder | Basis of Abnormality |
|---|---|
| Chronic bronchitis | Impaired ventilation of lung |
| Emphysema | Impaired ventilation of lung |
| Asthma | Impaired ventilation of lung |
| Pneumoconioses | Impaired ventilation of lung |
| Central or peripheral neuromuscular disorders | Impaired ventilation of lung |
| Right-to-left shunts of great vessels | Impaired perfusion of blood into lungs |
| Pulmonary embolism and pulmonary infarction | Impaired perfusion of blood into lungs |
| Sarcoidosis | Impaired diffusion of gases into blood |
| Selected lung cancers | Impaired diffusion of gases into blood |
| Disorder | Metabolic Alterations |
|---|---|
| |
|
|
| |
|
|
| |
|
|
| |
|
|