KEY POINTS
Appendicitis is one of the most common surgical emergencies in contemporary medicine, with a yearly incidence rate of about 100 per 100,000 inhabitants. Lifetime risk for appendicitis is 8.6% for males and 6.7% for females, with the highest incidence in the second decade of life.
The natural history of appendicitis is unclear, but it appears that progression to perforation is not predictable and that spontaneous resolution is common, suggesting that nonperforated and perforated appendicitis may, in fact, be different diseases.
Right lower quadrant pain, gastrointestinal symptoms starting after the onset of pain, and a systemic inflammatory response with leukocytosis and neutrophilia, increased C-reactive protein concentration, and fever are considered diagnostic of appendicitis. The Appendicitis Inflammatory Response Score or Alvarado score can help improve diagnostic accuracy.
Computed tomography scan has improved diagnostic accuracy in individual studies. However, in population-wide studies, the rate of misdiagnosis of appendicitis remains constant. Rates of misdiagnosis are highest in female patients of child-bearing age and patients on the extremes of age (i.e., very young and very old).
The role of nonoperative treatment for uncomplicated appendicitis remains controversial. Currently, appendectomy remains the standard of care. Laparoscopic appendectomy has a slight benefit over open appendectomy.
Perforated or complicated appendicitis is more common in the very young (age <5 years) and very old (age >65 years).
Complicated appendicitis without signs of sepsis or generalized peritonitis may benefit from nonoperative management. The role of interval appendectomy in these cases remains controversial.
Single-incision appendectomy provides no obvious advantage over standard laparoscopic appendectomy. Natural orifice transluminal endoscopic surgery remains an investigational procedure.
The incidence of fetal loss following normal appendectomy in pregnant patients is 4%, and the risk of premature delivery is 10%. The greatest opportunity to improve fetal outcomes may be through improving diagnostic accuracy and reducing the rate of negative appendectomy.
Antibiotic prophylaxis is effective in the prevention of postoperative surgical site infection. Postoperative antibiotics are unnecessary following uncomplicated appendicitis. For complicated appendicitis, a treatment duration of 4 to 7 days is recommended.
The role of incidental appendectomy is limited to patients at high risk for misdiagnosis of appendicitis (malrotation, patients unable to respond or react normally), patients at high risk for complications with appendicitis (children ready to undergo chemotherapy), and patients with limited access to modern healthcare.
The prevalence of appendiceal malignancy remains at or below 1% of appendectomies. Carcinoid and mucinous adenocarcinoma remain the most frequent histologic diagnosis.
HISTORICAL BACKGROUND
Appendiceal disease is a frequent reason for emergency hospital admission, and appendectomy is one of the most common emergency procedures performed in contemporary medicine. Despite the prevalent role this organ plays in healthcare today, the human appendix was not noted until 1492. Leonardo da Vinci depicted the appendix in his anatomic drawings, but these were not published until the eighteenth century.1 In 1521, Berengario Da Capri and, in 1543, Andreas Vesalius published drawings recognizing the appendix.2
Credit is given to Jean Fernel for first describing appendiceal disease in a paper published in 1544. He reported on a 7-year-old girl whose diarrhea he treated with doses of quince, an apple-like fruit used in folk remedies. She developed abdominal pain and died. At autopsy, the quince was found to have obstructed the lumen of the appendix, causing necrosis and perforation.3 Lorenz Heister provided the first description of classic appendicitis in 1711.1
The first known appendectomy was performed in 1736 by Claudius Amyand in London. He operated on an 11-year-old boy with a scrotal hernia and a fecal fistula. Within the hernia sac, Amyand found a perforated appendix surrounded by omentum. The appendix and omentum were amputated. The patient was discharged a month later in good condition.4
It would be over a century later before appendicitis was widely recognized as a common cause of right lower quadrant pain and early appendectomy advocated as treatment. Throughout this period, there was extensive discussion of typhlitis and perityphlitis as the common etiologies of right lower quadrant pain. Only sporadic cases of right lower quadrant pain were treated with appendectomy. In 1886, Reginald H. Fitz presented his findings regarding appendicitis and recommended consideration for operative treatment. In 1889, Charles McBurney published his landmark paper in the New York State Medical Journal describing the indications for early laparotomy for the treatment of appendicitis.5 During the following decade, the role of surgical treatment was discussed intensely between proponents of early appendectomy and of a more expectant management. It was recognized that most instances of appendicitis could resolve without surgical treatment; but, the problem was how to identify early the patients who had the progressive, often lethal form of the disease.6 Eventually, early appendectomy became the accepted standard of care, with broad indications in order to prevent perforation. This change in practice resulted in an enormous increase in the number of appendectomies during the first decades of the twentieth century. However, this had almost no impact on the incidence of perforated appendicitis or on the mortality of appendicitis.7 In the 1970s, the negative effects of the large number of appendectomies of uninflamed appendices were noted, and the focus gradually shifted toward a more conservative approach to exploration.8
EMBRYOLOGY, ANATOMY, AND PHYSIOLOGY
In the sixth week of human embryonic development, the appendix and cecum appear as outpouchings from the caudal limb of the midgut. The appendiceal outpouching, initially noted in the eighth week, begins to elongate at about the fifth month to achieve a vermiform appearance.9,10 The appendix maintains its position at the tip of the cecum throughout development. The subsequent unequal growth of the lateral wall of the cecum causes the appendix to find its adult position on the posterior medial wall, just below the ileocecal valve. The base of the appendix can be located by following the longitudinally oriented taeniae coli to their confluence on the cecum. The tip of the appendix can be located anywhere in the right lower quadrant of the abdomen, pelvis, or retroperitoneum.
In patients with midgut malrotation and situs inversus, the cecum (and thus the appendix) will not reside in the usual right lower quadrant location. With midgut malrotation, the midgut (small bowel and proximal colon) incompletely rotates or fails to rotate around the axis of the superior mesenteric artery during fetal development. In this situation, the appendix will remain in the left upper quadrant of the abdomen. Situs inversus is a rare autosomal recessive congenital defect characterized by the transposition of abdominal and/or thoracic organs. In this situation, the appendix is found in the left lower quadrant of the abdomen.11
In the adult, the average length of the appendix is 6 to 9 cm; however, it can vary in length from <1 to >30 cm. The outer diameter varies between 3 and 8 mm, whereas the luminal diameter varies between 1 and 3 mm.9
The appendix receives its arterial supply from the appendicular branch of the ileocolic artery. This artery originates posterior to the terminal ileum, entering the mesoappendix close to the base of the appendix.12 The lymphatic drainage of the appendix flows into lymph nodes that lie along the ileocolic artery. Innervation of the appendix is derived from sympathetic elements contributed by the superior mesenteric plexus (T10-L1) and afferents from the parasympathetic elements via the vagus nerves.12
The histologic features of the appendix are contained within the three following layers: the outer serosa, which is an extension of the peritoneum; the muscularis layer, which is not well defined and may be absent in certain locations; and finally, the submucosa and mucosa. Lymphoid aggregates occur in the submucosal layer and may extend into the muscularis mucosa. Lymphatic channels are prominent in regions underlying these lymphoid aggregates. The mucosa is like that of the large intestine, except for the density of the lymphoid follicles. The crypts are irregularly sized and shaped, in contrast to the more uniform appearance of the crypts in the colon. Neuroendocrine complexes composed of ganglion cells, Schwann cells, neural fibers, and neurosecretory cells are positioned just below the crypts.13,14
For many years, the appendix was erroneously believed to be a vestigial organ with no known function. It is now well recognized that the appendix is an immunologic organ that actively participates in the secretion of immunoglobulins, particularly immunoglobulin A.
Although there is no clear role for the appendix in the development of human disease, an inverse association between appendectomy and the development of ulcerative colitis has been reported, suggesting a protecting effect of the appendectomy. However, this association is only seen in patients treated with appendectomy for appendicitis before age 20.15,16,17
The association between Crohn’s disease and appendectomy is less clear. Although earlier studies suggested that appendectomy increases the risk of developing Crohn’s disease, more recent studies that carefully assessed the timing of appendectomy in relationship to the onset of Crohn’s disease demonstrated no correlation.17 A recent meta-analysis demonstrated a significant risk of Crohn’s disease early following appendicitis.18 This risk diminishes later, which suggests that a diagnostic (misidentifying Crohn’s disease as appendicitis) rather than a physiologic relationship exists between appendectomy and Crohn’s disease.
The appendix may function as a reservoir to recolonize the colon with healthy bacteria. One retrospective study demonstrated that prior appendectomy may have an inverse relationship to recurrent Clostridium difficile infections.19 However, in another retrospective study, prior appendectomy did not affect the rate of C. difficile infections.20 The role of the appendix in recolonizing the colon remains to be elucidated.
ACUTE APPENDICITIS
The lifetime risk of developing appendicitis is 8.6% for males and 6.7% for females, with the highest incidence in the second and third decades.21 The rate of appendectomy for appendicitis has been decreasing since the 1950s in most countries. In the United States, it reached its lowest incidence rate of about 15 per 10,000 inhabitants in the 1990s.22 Since then, there has been an increase in the incidence rate of nonperforated appendicitis. The reason for this is not clear, but it has been proposed that the increased use of diagnostic imaging has led to a higher detection rate of mild appendicitis that would otherwise resolve undetected.
The etiology and pathogenesis of appendicitis are not completely understood. Obstruction of the lumen due to fecaliths or hypertrophy of lymphoid tissue is proposed as the main etiologic factor in acute appendicitis. The frequency of obstruction rises with the severity of the inflammatory process. Fecaliths and calculi are found in 40% of cases of simple acute appendicitis,23 in 65% of cases of gangrenous appendicitis without rupture, and in nearly 90% of cases of gangrenous appendicitis with rupture.24
Traditionally, the belief has been that there is a predictable sequence of events leading to eventual appendiceal rupture. The proximal obstruction of the appendiceal lumen produces a closed-loop obstruction, and continuing normal secretion by the appendiceal mucosa rapidly produces distension. Distension of the appendix stimulates the nerve endings of visceral afferent stretch fibers, producing vague, dull, diffuse pain in the mid-abdomen or lower epigastrium. Distension increases from continued mucosal secretion and from rapid multiplication of the resident bacteria of the appendix. This causes reflex nausea and vomiting, and the visceral pain increases. As pressure in the organ increases, venous pressure is exceeded. Capillaries and venules are occluded but arterial inflow continues, resulting in engorgement and vascular congestion. The inflammatory process soon involves the serosa of the appendix and in turn the parietal peritoneum. This produces the characteristic shift in pain to the right lower quadrant.
The mucosa of the appendix is susceptible to impairment of blood supply; thus, its integrity is compromised early in the process, which allows bacterial invasion. The area with the poorest blood supply suffers the most: ellipsoidal infarcts develop in the antimesenteric border. As distension, bacterial invasion, compromise of the vascular supply, and infarction progress, perforation occurs, usually on the antimesenteric border just beyond the point of obstruction. This sequence is not inevitable, however, and some episodes of acute appendicitis may resolve spontaneously.
Appendicitis may occur in clusters, suggesting an infectious genesis. However, an association with various contagious bacteria and viruses has only been found in a small proportion of appendicitis patients.25 The flora of the inflamed appendix differs from that of the normal appendix. About 60% of aspirates of inflamed appendices have anaerobes compared to 25% of aspirates from normal appendices.26 Tissue specimens from the inflamed appendix wall (not luminal aspirates) virtually all grow Escherichia coli and Bacteroides species on culture.27,28 Fusobacterium nucleatum/necrophorum, which is not present in the normal cecal flora, has been identified in 62% of inflamed appendices.29 In addition to the other usual species (Peptostreptococcus, Pseudomonas, Bacteroides splanchnicus, Bacteroides intermedius, Lactobacillus), previously unreported fastidious gram-negative anaerobic bacilli have been encountered. Patients with gangrene or perforated appendicitis appear to have more tissue invasion by Bacteroides.
Because of the current predilection for surgical treatment, the natural history of appendicitis has not been well described. An increasing amount of circumstantial evidence suggests that not all patients with appendicitis will progress to perforation and that resolution may be a common event.30 Among the strongest evidence are two randomized trials comparing early laparoscopy with conservative management of patients with acute abdominal pain. These studies found three to five times more patients with appendicitis in the group of patients who were randomized to laparoscopy.31,32 Based on epidemiologic differences, it has been proposed that nonperforated and perforated appendicitis may, in fact, be different diseases.22
The inflammatory process in the appendix presents as pain, which initially is of a diffuse visceral type and later becomes more localized as the peritoneal lining gets irritated (Table 30-1).33
| TRUE POSITIVE LIKELIHOOD RATIO | 95% CONFIDENCE INTERVAL | TRUE NEGATIVE LIKELIHOOD RATIO | 95% CONFIDENCE INTERVAL | |
|---|---|---|---|---|
Duration of symptoms (hours) >9 >12 >24 >48 | 1.01 0.96 0.65 0.49 | 0.97–1.05 0.90–1.04 0.47–0.90 0.36–0.67 | 0.94 1.19 1.47 1.20 | 0.62–1.42 0.87–1.63 1.14–1.90 1.08–1.34 |
Fever | 1.64 | 0.89–3.01 | 0.61 | 0.49–0.77 |
Gastrointestinal dysfunction Anorexia Nausea Vomiting | 1.27 1.15 1.63 | 1.14–1.41 1.04–1.36 1.45–1.84 | 0.59 0.72 0.75 | 0.45–0.77 0.57–0.91 0.69–0.80 |
Pain Pain migration Pain progression Direct tenderness Indirect tenderness Psoas sign Rebound Percussion tenderness Guarding Rigidity | 2.06 1.39 1.29 2.47 2.31 1.99 2.86 2.48 2.96 | 1.63–2.60 1.29–1.50 1.06–1.57 1.38–4.43 1.36–3.91 1.61–2.45 1.95–4.21 1.60–3.84 2.43–3.59 | 0.52 0.46 0.25 0.71 0.85 0.39 0.49 0.57 0.86 | 0.40–0.69 0.27–0.77 0.12–0.53 0.65–0.77 0.76–0.95 0.32–0.48 0.37–0.63 0.48–0.68 0.72–1.02 |
Temperature (degrees centigrade) >37.7 >38.5 | 1.57 1.87 | 0.90–2.76 0.66–5.32 | 0.65 0.89 | 0.31–1.36 0.71–1.12 |
White blood cells (109/L) ≥10 ≥15 | 4.20 7.20 | 2.11–8.35 4.31–12.00 | 0.20 0.66 | 0.10–0.41 0.56–0.78 |
C-reactive protein (mg/L) >10 >20 | 1.97 2.39 | 1.58–2.45 1.67–3.41 | 0.32 0.47 | 0.20–0.51 0.28–0.81 |
Appendicitis usually starts with periumbilical and diffuse pain that eventually localizes to the right lower quadrant (sensitivity, 81%; specificity, 53%).34 Although right lower quadrant pain is one of the most sensitive signs of appendicitis, pain in an atypical location or minimal pain will often be the initial presentation. Variations in the anatomic location of the appendix may account for the differing presentations of the somatic phase of pain.
Appendicitis is also associated with gastrointestinal symptoms like nausea (sensitivity, 58%; specificity, 36%), vomiting (sensitivity, 51%; specificity, 45%), and anorexia (sensitivity, 68%; specificity, 36%). Gastrointestinal symptoms that develop before the onset of pain suggest a different etiology such as gastroenteritis.34 Many patients complain of a sensation of obstipation prior to the onset of pain and feel that defecation will relieve their abdominal pain. Diarrhea may occur in association with perforation, especially in children.
Early in presentation, vital signs may be minimally altered. The body temperature and pulse rate may be normal or slightly elevated. Changes of greater magnitude may indicate that a complication has occurred or that another diagnosis should be considered.35
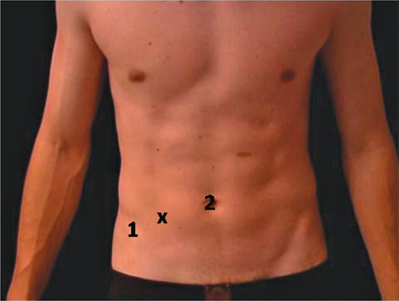
Physical findings are determined by the presence of peritoneal irritation and are influenced by whether the organ has already ruptured when the patient is first examined. Patients with appendicitis usually move slowly and prefer to lie supine due to the peritoneal irritation. On abdominal palpation, there is tenderness with a maximum at or near McBurney’s point (Fig. 30-1).5 On deep palpation, one can often feel a muscular resistance (guarding) in the right iliac fossa, which may be more evident when compared to the left side. When the pressure of the examining hand is quickly relieved, the patient feels a sudden pain, the so-called rebound tenderness. Indirect tenderness (Rovsing’s sign) and indirect rebound tenderness (i.e., pain in the right lower quadrant when the left lower quadrant is palpated) are strong indicators of peritoneal irritation. Rebound tenderness can be very sharp and uncomfortable for the patient. It is therefore recommended to start with testing for indirect rebound tenderness and direct percussion tenderness.
Anatomic variations in the position of the inflamed appendix lead to deviations in the usual physical findings. With a retrocecal appendix, the abdominal findings are less striking, and tenderness may be most marked in the flank. When the appendix hangs into the pelvis, abdominal findings may be entirely absent, and the diagnosis may be missed. Right-sided rectal tenderness is said to help in this situation, but the diagnostic value is low. Pain with extension of the right leg (psoas sign) indicates a focus of irritation in the proximity of the right psoas muscle. Similarly, stretching of the obturator internus through internal rotation of a flexed thigh (obturator sign) suggests inflammation near the muscle.
Appendicitis is associated with an inflammatory response that is strongly related to the severity of the disease. Laboratory examinations are therefore an important part of the diagnosis. Mild leukocytosis is often present in patients with acute, uncomplicated appendicitis and is usually accompanied by a polymorphonuclear prominence. It is unusual for the white blood cell count to be >18,000 cells/mm3 in uncomplicated appendicitis. Counts above this level raise the possibility of a perforated appendix with or without an abscess. An increased C-reactive protein (CRP) concentration is a strong indicator of appendicitis, especially for complicated appendicitis.36
White blood cell counts can be low due to lymphopenia or septic reaction, but in this situation, the proportion of neutrophils is usually very high. Therefore, all inflammatory variables should be viewed together. Appendicitis is very unlikely if the white blood cell count, proportion of neutrophils, and CRP are all normal. The inflammatory response in acute appendicitis is a dynamic process. Early in the process, the inflammatory response can be weak. CRP elevation, in particular, can have up to a 12-hour delay. A decreasing inflammatory response may indicate spontaneous resolution.
Urinalysis can be useful to rule out the urinary tract as the source of infection; however, several white or red blood cells can be present from irritation of the ureter or bladder. Bacteriuria is generally not seen.
The clinical diagnosis of appendicitis is a subjective estimate of the probability of appendicitis based on multiple variables that individually are weak discriminators; however, used in conjunction, they possess a high predictive value. This process can be made more objective by the use of clinical scoring systems, which are based on variables with proven discriminating power and assigned a proper weight. The Alvarado score is the most widespread scoring system. It is especially useful for ruling out appendicitis and selecting patients for further diagnostic workup.37 The Appendicitis Inflammatory Response Score resembles the Alvarado score but uses more graded variables and includes CRP (Table 30-2).38,39 Studies have shown it to perform better than the Alvarado score in accurately predicting appendicitis.38,39 However, clinical scoring systems have not gained widespread acceptance in making the diagnosis of appendicitis.
| ALVARADO SCORE37 | APPENDICITIS INFLAMMATORY RESPONSE SCORE38,39 | ||
|---|---|---|---|
Findings Migratory right iliac fossa pain Anorexia Nausea or vomiting Tenderness: right iliac fossa Rebound tenderness right iliac fossa Fever ≥36.3°C Leukocytosis ≥10 × 109 cells/L Shift to the left of neutrophils | Points 1 1 1 2 1 1 2 1 | Findings Vomiting Pain in the right inferior fossa Rebound tenderness or muscular defense Light Medium Strong Body temperature ≥38.5°C Polymorphonuclear leukocytes 70%–84% ≥85% White blood cell count 10.0–14.9 × 109 cells/L ≥15.0 × 109 cells/L C-reactive protein concentration 10–49 g/L ≥50 g/L | Points 1 1 1 2 3 1 1 2 1 2 |
Plain films of the abdomen can show the presence of a fecalith and fecal loading in the cecum associated with appendicitis but are rarely helpful in diagnosing acute appendicitis40; however, they may be of benefit in ruling out other pathology. A chest radiograph is helpful to rule out referred pain from a right lower lobe pneumonic process. If the appendix fills on barium enema, appendicitis is unlikely41; however, this test is not indicated in the acute setting. Technetium-99m–labeled leukocyte scan has been reported for use in diagnosing appendicitis with good results but has not gained widespread use due to its relative unavailability and impracticality in daily use.42
Ultrasonography and computed tomography (CT) scan are the most commonly used imaging tests in patients with abdominal pain, particularly in evaluation of possible appendicitis. Multiple meta-analyses have been performed comparing the two imaging modalities (Table 30-3).43,44,45,46,47 Overall, CT scan is more sensitive and specific than ultrasonography in diagnosing appendicitis.
| AUTHOR | SUMMARY | ||||||
|---|---|---|---|---|---|---|---|
| TERASAWA | WESTON | DORIA | AL-KHAYAL | VAN RANDEN | |||
| Year | 2004 | 2005 | 2006 | 2007 | 2008 | ||
| No. of studies | 22 | 21 | 57 | 25 | 6 | ||
| No. of patients | CT US Total | 1172 1516 2688 | NR NR 5039 | NR NR 13697 | NR NR 13046 | NR NR 671 | |
| Sensitivity | CT US | 94% (CI: 91%–95%) 86% (CI: 83%–88%) | 97% (CI: 95%–98%) 87% (CI: 85%–89%) | 94% (CI: 92%–97%) 88% (CI: 86%–90%) | 93% (CI: 92%–95%) 84% (CI: 82%–85%) | 91% (CI: 84%–95%) 78% (CI: 67%–86%) | CT more sensitive than US in five of five meta-analyses |
| Specificity | CT US | 95% (CI: 93%–96%) 81% (CI: 78%–84%) | 95% (CI: 93%–96%) 93% (CI: 92%–94%) | 94% (CI: 94%–96%) 93% (CI: 90%–96%) | 93 (CI: 92%–94%) 96 (CI: 95%–96%) | 90% (CI: 85%–94%) 83% (CI: 76%–88%) | CT more specific than US in four of five meta-analyses |
| Positive predictive value | CT US | NR NR | 94% (CI: 92%–95%) 89% (CI: 87%–90%) | NR NR | 90% (CI: 89%–92%) 90% (CI: 89%–91%) | NR NR | CT has superior positive predictive value in one of two meta-analyses |
| Negative predictive value | CT US | NR NR | 97% (CI: 96%–98%) 92% (CI:91%–93%) | NR NR | 96% (CI: 95%–97%) 93% (CI: 92%–94%) | NR NR | CT has superior negative predictive value in both meta-analyses |
| Accuracy | CT US | NR NR | NR NR | NR NR | 94% (CI: 93%–94%) 92% (CI: 92%–96%) | NR NR | CT is more accurate in the one study reporting results |
Graded compression ultrasonography is inexpensive, can be performed rapidly, does not require a contrast medium, and can be used in pregnant patients. Sonographically, the appendix is identified as a blind-ending, nonperistaltic bowel loop originating from the cecum. With maximal compression, the diameter of the appendix is measured in the anterior-posterior direction. Thickening of the appendiceal wall and the presence of periappendiceal fluid are highly suggestive of appendicitis. Demonstration of an easily compressible appendix measuring <5 mm in diameter excludes the diagnosis of appendicitis. The sonographic diagnosis of acute appendicitis has a reported sensitivity of 55% to 96% and a specificity of 85% to 98%. Ultrasonography is similarly effective in children and pregnant women, although its application is limited in late pregnancy. Ultrasonography has its limitations, particularly the operator-dependent nature of results. In the adult population, ultrasonography remains limited in its use.
With high-resolution helical CT, the inflamed appendix appears dilated (>5 mm), and the wall is thickened. There is often evidence of inflammation, which can include periappendiceal fat stranding, thickened mesoappendix, periappendiceal phlegmon, and free fluid. Fecaliths can be often visualized; however, their presence is not pathognomonic of appendicitis. CT scanning is also an excellent technique for identifying other inflammatory processes masquerading as appendicitis. Several CT techniques have been used, including focused and nonfocused CT scans and contrast and noncontrast scans. Surprisingly, all of these techniques have yielded essentially identical rates of diagnostic accuracy: 92% to 97% sensitivity, 85% to 94% specificity, 90% to 98% accuracy, 75% to 95% positive predictive value, and 95% to 99% negative predictive value. The additional use of rectal contrast does not improve the results of CT scanning.
A number of studies have documented improvement in diagnostic accuracy with the liberal use of CT scanning in the workup of suspected appendicitis. CT lowered the rate of negative appendectomies from 19% to 12% in one study48 and the incidence of negative appendectomies in women from 24% to 5% in another study.49 Use of CT altered the care of 24% of patients studied and provided an alternative diagnosis in half of the patients with normal appendices on CT scan.
Despite the potential usefulness of CT, there are significant disadvantages. CT scanning is expensive, exposes the patient to significant radiation, and has limited use during pregnancy. Allergy to iodine or contrast limits the administration of contrast agents in some patients, and others cannot tolerate the oral ingestion of luminal dye.
The role of CT scanning in patients who present with right lower quadrant pain is unclear. One rationale is universal CT scanning. There is, however, an argument that indiscriminate diagnostic imaging can increase the detection of clinically nonsignificant appendicitis that would resolve without treatment. Alternatively, selective CT scanning based on the likelihood of appendicitis takes advantage of the clinical skills of the surgeon and, when indicated, adds the expertise of the radiologist.
Despite the increased use of ultrasonography and CT, the rate of misdiagnosis of appendicitis has remained constant (15%). The percentage of misdiagnosed cases of appendicitis is significantly higher among women than men (22% vs. 9.3%).50,51 The negative appendectomy rate is highest in women of reproductive age.
The differential diagnosis of acute appendicitis is essentially the diagnosis of acute abdomen. An identical clinical picture can result from a wide variety of acute processes within the peritoneal cavity that produce the same physiologic alterations as acute appendicitis.
The accuracy of preoperative diagnosis should be higher than 85%. If it is consistently less, it is likely that unnecessary operations are being performed and a more rigorous preoperative differential diagnosis is needed.
The most common findings in the case of an erroneous preoperative diagnosis of appendicitis—together accounting for more than 75% of cases—are, in descending order of frequency, acute mesenteric adenitis, no organic pathologic condition, acute pelvic inflammatory disease, twisted ovarian cyst or ruptured graafian follicle, and acute gastroenteritis.
The differential diagnosis of acute appendicitis depends on four major factors: the anatomic location of the inflamed appendix; the stage of the process (uncomplicated or complicated); the patient’s age; and the patient’s gender.52,53,54,55,56
Acute mesenteric adenitis is the disease most often confused with acute appendicitis in children. Almost invariably, an upper respiratory tract infection is present or has recently subsided. The pain usually is diffuse, and tenderness is not as sharply localized as in appendicitis. Voluntary guarding is sometimes present, but true rigidity is rare. Generalized lymphadenopathy may be noted. Laboratory procedures are of little help in arriving at the correct diagnosis, although a relative lymphocytosis, when present, suggests mesenteric adenitis. Observation for several hours is appropriate if the diagnosis of mesenteric adenitis is suspected, as it is a self-limited disease.
Diverticulitis or perforating carcinoma of the cecum or of a portion of the sigmoid that overlies the right lower abdomen may be impossible to distinguish from appendicitis. These entities should be considered, particularly in older patients. CT scanning is often helpful in making a diagnosis in older patients with right lower quadrant pain and atypical clinical presentations. In patients successfully managed conservatively, interval surveillance of the colon (colonoscopy or barium enema) may be warranted.
Diseases of the female internal reproductive organs that may erroneously be diagnosed as appendicitis are, in approximate descending order of frequency, pelvic inflammatory disease, ruptured graafian follicle, twisted ovarian cyst or tumor, endometriosis, and ruptured ectopic pregnancy. As a result, the rate of misdiagnosis remains higher among female patients.
In pelvic inflammatory disease, the infection is usually bilateral but, if confined to the right tube, may mimic acute appendicitis. Nausea and vomiting are present in patients with appendicitis but in only approximately 50% of those with pelvic inflammatory disease. Pain and tenderness are usually lower, and motion of the cervix is exquisitely painful. Intracellular diplococci may be demonstrable on smear of the purulent vaginal discharge. The ratio of cases of appendicitis to cases of pelvic inflammatory disease is low in females in the early phase of the menstrual cycle and high during the luteal phase. The careful clinical use of these features has reduced the incidence of negative findings on laparoscopy in young women to 15%.
Ovulation commonly results in the spillage of sufficient amounts of blood and follicular fluid to produce brief, mild lower abdominal pain. If the amount of fluid is unusually copious and is from the right ovary, appendicitis may be simulated. Pain and tenderness may be rather diffuse, and leukocytosis and fever minimal or absent. Because this pain occurs at the midpoint of the menstrual cycle, it is often called mittelschmerz.
Serous cysts of the ovary are common and generally remain asymptomatic. When right-sided cysts rupture or undergo torsion, the manifestations are similar to those of appendicitis. Patients develop right lower quadrant pain, tenderness, rebound, fever, and leukocytosis. Both transvaginal ultrasonography and CT scanning can be diagnostic.
Torsion requires emergent operative treatment. If the torsion is complete or longstanding, the pedicle undergoes thrombosis, and the ovary and tube become gangrenous and require resection. However, simple detorsion, fenestration of the cyst, and fixation of the ovary as a primary intervention, followed by a laparoscopy a few days later, can be recommended because it is often difficult to preoperatively determine the viability of the ovary.
Blastocysts may implant in the fallopian tube (usually the ampullary portion) and in the ovary. Rupture of right tubal or ovarian pregnancies can mimic appendicitis. Patients may give a history of abnormal menses, either missing one or two periods or noting only slight vaginal bleeding. Unfortunately, patients do not always realize they are pregnant. The development of right lower quadrant or pelvic pain may be the first symptom. The diagnosis of ruptured ectopic pregnancy should be relatively easy. The presence of a pelvic mass and elevated levels of human chorionic gonadotropin are characteristic. Although the leukocyte count rises slightly, the hematocrit level falls as a consequence of the intra-abdominal hemorrhage. Vaginal examination reveals cervical motion and adnexal tenderness, and a more definitive diagnosis can be established by culdocentesis. The presence of blood and particularly decidual tissue is pathognomonic. The treatment of ruptured ectopic pregnancy is emergency surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree