Techniques for Correcting Lumpectomy Defects
Julie E. Park
Jonathan Bank
David H. Song
DEFINITION
Breast conservation therapy (BCT), the combination of lumpectomy and breast radiation, allows women with breast cancer to avoid mastectomy without compromising outcome. Although the majority of women will have an excellent cosmetic outcome, some women will develop asymmetry from volume loss and postradiation contour deformity and nipple-areolar complex (NAC) deviation. Several techniques exist for correcting lumpectomy defects to allow for oncologically sound and aesthetically acceptable BCT.
PATIENT HISTORY AND PHYSICAL FINDINGS
In some situations, the plastic surgeon is asked to evaluate the patient prior to lumpectomy in order to plan for an immediate correction. In other situations, the patient is referred to plastic surgery after radiation therapy for correction of postradiation contour deformity and NAC deviation.
It is important to discuss with the patient her expectations; specifically, whether she would accept a smaller breast.
Does the patient have symptomatic macromastia and would she benefit from, or be interested in, breast reduction?
Does the patient smoke? This might impact nipple perfusion.
A thorough breast examination should take note of the breast size and any preexisting asymmetry. Any previous scars or contour deformities should be noted, especially in women who have already completed BCT.
It is also important to document the position of the nipple, including any ptosis, and the distance from the sternal notch.
For patients anticipated to have a significant deformity from BCT, a multidisciplinary approach is critical to achieving the optimal cosmetic outcome. Communication with the surgical oncologist is critical to both identifying appropriate patients, planning the site and expected volume of resection, and coordinating schedules. It is important to identify with the radiation oncologist if the patient will require a “boost,” as this will limit how much tissue can be rearranged. In cases of wire-localized lumpectomy, marks should be placed prior to wire placement and this should be coordinated with the breast radiologist.
IMAGING AND OTHER DIAGNOSTIC STUDIES
SURGICAL MANAGEMENT
Preoperative Planning
The goals of correcting lumpectomy defects include obliterating any dead space, supporting the NAC and maintaining adequate perfusion, and resecting any excess skin.
There are two main options for reconstructing a lumpectomy defect. Volume displacement techniques use parenchymal remodeling (volume shrinkage). Volume replacement techniques use both local and distant tissue to preserve volume.
After reviewing the preoperative imaging and discussing with the surgical oncologist, the next question is whether given the size and location of the tumor, will there be sufficient tissue in the breast to rearrange and obliterate dead space without losing too much volume?
Yes—volume displacement: reduction, mastopexy, or intrinsic breast flaps
No—volume replacement: local rotational flaps
Thoracodorsal artery perforator (TAP) or muscle-sparing latissimus dorsi (MSLD) flap
Lateral intercostal artery perforator (LICAP) flap
Positioning
The patient is positioned supine with the arms secured to the arm boards at the side to allow for sitting the patient up during the surgery (FIG 2). The arms should be place on padded arm boards and positioned in a way that pressure points are alleviated.
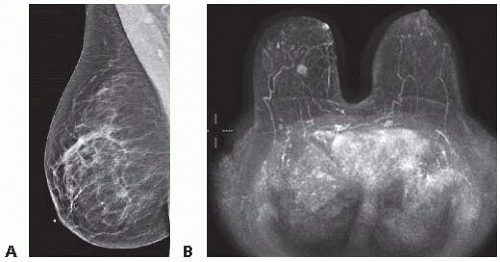 FIG 1 • Mammogram (A) and MRI (B) of patient with 1.1 × 1.0 × 0.8 cm right-sided breast cancer at 5 o’clock position. |
 FIG 2 • Positioning of a patient with both arms abducted, padded, and secured, enabling seating the patient during surgery to assess for symmetry of reconstruction. |
TECHNIQUES
FREESTYLE INTRINSIC BREAST FLAPS
For some defects, dermatoglandular flaps can be created to fill small defects. Depending on the location, even small defects can lead to unfavorable cosmetic results, particularly a significant concavity at the site of the lumpectomy after radiation. This can occur when there is minimal tissue between the skin and underlying muscle.
The principle of intrinsic breast flaps is to focus on perfusion and support to the NAC and to obliterate the dead space.
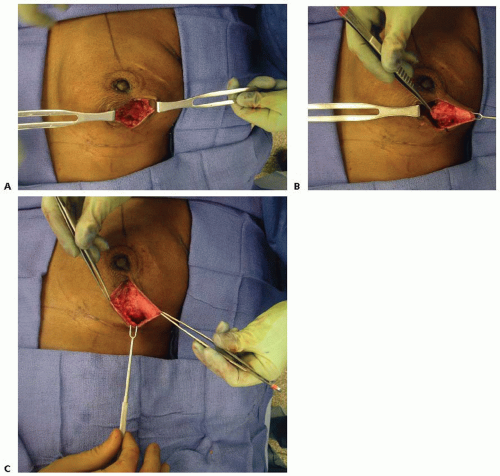
The lumpectomy cavity is examined to evaluate how much dead space there is and the remainder of the breast is assessed for where there is extra tissue (FIG 4A). An intrinsic breast flap is created by dissecting between the skin and breast parenchyma and between the breast parenchyma and pectoralis (FIG 4B). The flaps are based either on axial blood supply from perforators originating from the internal mammary artery or from the intercostal vessels. As these vessels are not typically identified in the dissection, the flaps should be created as random pattern flaps, adhering to the principles of creating broad-based flaps that are not too lengthy as to put the distal tip of the flap at risk of ischemia. The flap is then advanced and secured to fill the lumpectomy cavity and to maintain support to NAC (FIG 4C).
Any excess skin is resected and the wound is closed.
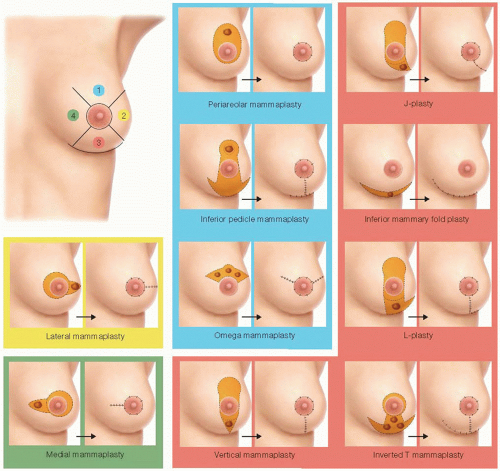 FIG 3 • There are multiple options for skin incisions for resections depending on the location of the defect, size of the defect, and size of the breast. |
INFERIOR POLE LUMPECTOMY DEFECTS— THE VERTICAL MAMMAPLASTY TECHNIQUE
Preoperative Marking
This approach is an option for patients with lumpectomy defects from approximately 4 o’clock to 8 o’clock positions.
For patients with appropriately sized breasts, a vertical reduction pattern is marked out on the breast (FIG 5). Alternatively, an inverted T pattern can be used.
With the patient in the upright position, landmarks are drawn—sternal notch, midline, and breast meridians. The new position of NAC is marked out, along with any excess skin as follows: the breast mobilized laterally, vertical line drawn medially, then the breast mobilized medially, vertical line drawn laterally. The vertical components connected with curved line 2 to 4 cm above
the inframammary fold (IMF). A mosque-shaped marking is drawn for inset of NAC.
Assess Lumpectomy Defect and Nipple-Areolar Complex
In the operating room, the prior lumpectomy cavity is opened and the seroma evacuated. As there will no longer be a seroma to guide radiation, it is a good idea to place several small clips at the boundaries of the lumpectomy defect.
Confirm perfusion and support to NAC and make sure that the lumpectomy cavity is not undermining the NAC. If it is, you need to plan on supporting it with intrinsic breast tissue. If this is not possible, a free nipple graft (FNG) will be needed: The NAC is excised as a full-thickness skin graft, defatted, replaced on a well-vascularized bed in the appropriate position on the breast mound, and secured in place with a bolster dressing.
Convert to Vertical Reduction
Additional (i.e., more than the lumpectomy) breast tissue is resected as needed to allow for an acceptable final shape. Undermining of the breast off of the pectoralis is usually confined to inferior breast. Tissue is resected medial and lateral to vertical incision to allow “rounding off” of the breast. The parenchyma is approximated centrally (approximating the medial and lateral remaining portions of the breast—the medial and lateral “pillars”).
Skin closure—excessed gathered in subcuticular closure. A small horizontal excision is made along the IMF if needed to further reduce the skin.
This approach will result in volume loss, so a contralateral reduction will be needed in the future, approximately 3 to 6 months after radiation therapy has been completed.
VOLUME REPLACEMENT PEDICLED FLAPS
For patients with larger defects for which displacement techniques would not work, replacement techniques may be necessary. Pedicled flaps are recommended. Free tissue transfer is not initially recommended in this situation, as it eliminates the use of a flap in the future should the patient have a local recurrence or new tumor and require a mastectomy. Free flaps should only be considered if pedicled flaps are not feasible or fail.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree