Synovial Sarcoma
Key Facts
Clinical Issues
Predilection for young adults (median: 35 years)
Female predilection (2:1)
Aggressive behavior similar to soft tissue counterpart
Microscopic Pathology
Uniform and monotonous proliferation of atypical oval to spindle cells with minimal stroma
Glandular structures may be very focal or may predominate
Fascicular growth pattern with “herringbone” appearance is most common histologic pattern of growth
Many tumors show, at least focally, a prominent hemangiopericytomatous growth pattern
Other growth patterns include storiform, palisading, and sclerosing
Stromal changes may include fibrosis, calcifications, and myxoid changes
Ancillary Tests
Pattern of cytokeratin positivity in monophasic spindle cell tumors is usually weak and focal (patchy)
Spindle cells
Strongly and diffusely stain for Bcl-2
Usually stain for CD99
May be positive for S100 protein in 30% of cases
Are negative for actin, desmin, CD34, HMB-45, CEA, MOC-31, and p63
(X;18)(p11;q11) translocation is characteristically present in > 80% of cases
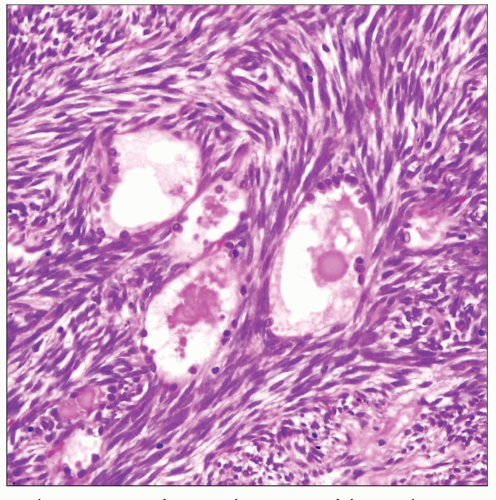
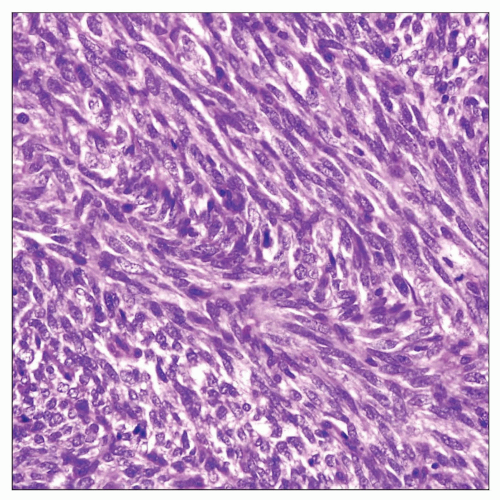 Monophasic spindle cell variant of synovial sarcoma of the mediastinum shows a monotonous population of atypical spindle cells with scant stroma. |
TERMINOLOGY
Abbreviations
Synovial sarcoma (SS)
Synonyms
Primary carcinoma of soft tissue
Definitions
Primary malignant epithelial neoplasm arising from soft tissues
ETIOLOGY/PATHOGENESIS
Pathogenesis
Unknown; unrelated to synovium or synovial cells
Pluripotential mesenchymal cells capable of aberrant epithelial differentiation
CLINICAL ISSUES
Epidemiology
Incidence
Rare tumor
Age
Broad age range: 3-83 years
Predilection for young adults (median: 35 years)
Gender
Female predilection (2:1)
Site
May involve all mediastinal compartments: Anterior, middle, and posterior
Presentation
Cough
Chest pain
Pleural effusion
Shortness of breath
Neck or back pain
Treatment
Surgical excision
Prognosis
Aggressive behavior similar to soft tissue counterpart
Local recurrences and distant metastases to lung, lymph nodes, liver, and epidural space
IMAGE FINDINGS
General Features
Tumors may present as well circumscribed or infiltrative masses with focal calcifications
CT Findings
Well-circumscribed mediastinal mass with low attenuation
Pleural effusion
MACROSCOPIC FEATURES
General Features
Usually well-circumscribed, fleshy tumors surrounded by thin, fibrous capsule
May be infiltrative and extend into surrounding structures, such as lung, pleura, pericardium, chest wall, and ribs
Cut section shows gray-white to tan, homogeneous soft tissue with gelatinous consistency
Some cases may undergo extensive cystic changes
May contain scattered calcifications
Can show focal hemorrhage and necrosis
Sections to Be Submitted
1 section per each centimeter of largest tumor diameter
Size
5-20 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Monophasic (spindle cell) synovial sarcoma
Uniform and monotonous proliferation of atypical oval to spindle cells with minimal stroma
Spindle cells show vesicular or hyperchromatic nuclei with coarse chromatin pattern and inconspicuous nucleoli
Mitotic activity may vary from low (1 mitosis per 10 HPF) to high (> 10 mitoses per 10 HPF)
Fascicular growth pattern with “herringbone” appearance is most common histologic pattern of growth
Many tumors show, at least focally, a prominent hemangiopericytomatous growth pattern
Other growth patterns include storiform, palisading, sclerosing, nesting, and rhabdoid
Stromal changes may include fibrosis, calcifications, and myxoid changes
“Poorly differentiated” variant characterized by round cell, epithelioid morphology rather than spindle cells
Some tumors can show prominent hemorrhage and necrosis
Secondary cystic changes are often seen in monophasic tumors
Biphasic synovial sarcoma
Shows admixture of well-formed glandular structures and spindle cells
Spindle cell component surrounding glands has identical features to those seen in monophasic variant
Glandular structures may be very focal or may predominate
Glandular structures are lined by large, round to polygonal or columnar epithelial cells
Glandular cells are round to oval nuclei with abundant eosinophilic cytoplasm
Glands may contain dense, homogeneous eosinophilic secretions in lumen
Glandular structures may adopt tubulo-papillary pattern with intraluminal papillary infoldings
Glandular structures can display prominent cytoplasmic clearing of tumor cells
ANCILLARY TESTS
Immunohistochemistry
All biphasic tumors show strong keratin positivity in the glandular component
Monophasic tumors are frequently, but not always, positive for cytokeratin stains
Pattern of cytokeratin positivity in monophasic spindle cell tumors is usually weak and focal (patchy)
Epithelial membrane antigen (EMA) shows similar pattern and distribution as cytokeratin
Low molecular weight cytokeratins are more sensitive than broad-spectrum cytokeratins for monophasic tumors
Spindle cells
Strongly express vimentin
Strongly and diffusely stain for Bcl-2
Usually stain for CD99
May be positive for calretinin and calponin
May be positive for S100 protein in 30% of cases
Negative for actin, desmin, CD34, HMB-45, CEA, MOC-31, and p63
Cytogenetics
(X;18)(p11;q11) translocation characteristically present in > 80% of cases
Other complex translocations may be found infrequently
FISH and Rt-PCR are useful for detecting translocations in paraffin-embedded tissues
2/3 contain an SYT/SSX1 fusion
1/3 contain an SYT/SSX2 fusion
Rare cases may show an SYT/SSX4 fusion
Cases with SYT/SSX2 fusion are associated with better prognosis
Electron Microscopy
Glandular epithelial component shows similar features to adenocarcinoma
Monophasic spindle cell component shows closely apposed cell membranes, frequent desmosomal junctions, and occasional surface microvilli
Monophasic spindle cell component does not contain abundant rough endoplasmic reticulum or other features of fibroblastic cells
DIFFERENTIAL DIAGNOSIS
Metastatic Adenocarcinoma
Clinical history is helpful for diagnosis
Metastatic adenocarcinoma will usually not contain stromal, atypical spindle cell component
Pulmonary Blastoma
Only rarely will secondarily involve mediastinum, but bulk of tumor will be centered in lung
Cells lining glands in pulmonary blastoma show subnuclear clearing simulating fetal lung
Most biphasic pulmonary blastomas are characterized by squamoid morules located at base of glands
Spindle cell component in pulmonary blastoma is negative for epithelial markers (keratin, EMA)
Thymic Carcinosarcoma
Spindle cell component in thymic carcinosarcoma is negative for epithelial markers (keratin, EMA)
Glandular component in thymic carcinosarcoma displays pronounced nuclear atypia
Negative for t(X;18) translocation
Biphasic Pleural Mesothelioma
Usually grows as diffuse, plaque-like process covering pleural surface, rather than discrete, well-circumscribed tumor mass
Spindle cell component in pleural mesothelioma shows marked cytologic atypia and nuclear pleomorphism
Spindle cells in pleural mesothelioma are negative for Bcl-2 and CD99
Spindle Cell Thymoma
Slow-growing tumor that is usually encapsulated and noninvasive
Absence of cytologic atypia or mitotic activity in spindle cells
Lobular architecture with fibrous bands separating lobules
Presence of immature T lymphocytes
Spindle cells are negative for vimentin, CD99, and Bcl-2
Spindle Cell Thymic Carcinoma
Marked cytologic atypia, nuclear pleomorphism, and mitotic activity
Spindle cells are negative for Bcl-2 and CD99
Absence of t(X;18) translocation
Malignant Peripheral Nerve Sheath Tumor
Commonly arises in background of neurofibromatosis
Grossly associated with nerve trunks
Spindle cells are negative for cytokeratins and CD99
Electron microscopy shows complex interdigitating cytoplasmic processes invested by basal lamina material
Absence of t(X;18) translocation
Solitary Fibrous Tumor
Usually shows variegation in growth patterns within same tumor and lack of uniformity of cell population
Commonly shows variable degrees of stromal fibrosis, including characteristic, rope-like deposition of keloidal collagen
Spindle cells are positive for CD34
Spindle cells are negative for cytokeratins and EMA
Absence of t(X;18) translocation
Metastasis of Synovial Sarcoma of Soft Tissue to Mediastinum
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree