Surgical Management of Anal Fissures
Daniel Albo
DEFINITION
An anal fissure is an acute longitudinal tear or a chronic ovoid ulcer in the squamous epithelium of the anal canal.
They are also often referred to as fissure in ano.
The exact etiology of anal fissures is debated. Risk factors that increase the likelihood of developing an anal fissure include the following:
Increased sphincter tone
Chronic constipation
Straining to have a bowel movement, especially if the stool is large, hard, and/or dry
Sedentary lifestyle
Sexual practices: anal intercourse, insertion of anal/rectal foreign bodies
Overly tight or spastic anal sphincter muscles: failure of relaxation of the anal sphincter during bowel movements
Decreased blood flow to the perianal skin
Scarring in the anorectal area
Inflammatory bowel disease, such as Crohn’s disease and ulcerative colitis
Anal cancer, especially after radiation therapy
Tuberculosis
Sexually transmitted diseases (such as syphilis, gonorrhea, chlamydia, chancroid, HIV)
Leukemic infiltrates
Decreased blood flow to the anorectal area
Anal fissures are also common in women after childbirth and in young infants.
Women are more commonly affected than men (58% vs. 42%).
DIFFERENTIAL DIAGNOSIS
Hemorrhoids (specially thrombosed hemorrhoids)
Anal canal cancer
Anal trauma
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients typically present with intense anal pain during and especially after defecation. The pain can last for several minutes to a few hours after having a bowel movement.
Although patients are often asymptomatic between bowel movements, they often develop a “fear of defecation” and may try to avoid defecation secondary to the pain.
Chronic constipation is common.
Some bright red anal bleeding, especially on the toilet paper, is common.
On physical exam, the anus appears tight and spastic. The pain is usually severe enough that the patient will not tolerate a digital rectal exam in the office.
On anoscopy, which oftentimes is done under conscious sedation due to severe anal pain, the fissure is usually linear, although ovoid-shaped fissures are oftentimes seen as well.
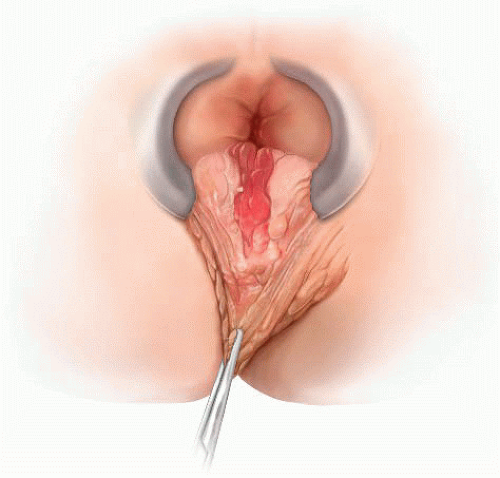
Anal fissures are almost universally present along the posterior midline in men and they are often associated with a sentinel skin tag at the squamous-columnar epithelial junction (anal verge). In women, they can also be seen on an anterior location (FIG 1).
Anal fissures seen in Crohn’s disease and tuberculosis are frequently painless.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Diagnosis is made by visual inspection. Unless findings suggest a specific cause or the appearance and/or location is unusual, further studies are not required.
In selected cases, flexible sigmoidoscopy or colonoscopy may be indicated.
SURGICAL MANAGEMENT
The majority of anal fissures will resolve with medical management and will not require surgery.
Medical management includes the following:
Aggressive prevention of constipation
Increase fiber and decrease fat in the diet
Fiber supplementation
Increase water intake
Use of moist pads (flushable baby wipes) for wiping and anal hygiene
Avoiding straining or prolonged sitting on the toilet
Soaking in a warm bath (also called a sitz bath), 10 to 20 minutes several times a day, to promote the relaxation of the anal muscles
These conservative measures lead to healing of the anal fissure in a few weeks to a few months in 80% to 90% of patients. However, when these conservative measures alone are not successful, pharmacologic intervention can also be instituted. This includes the following:
Topical nitrates ointment: Examples include nitroglycerin ointment 0.4% (Rectiv) and glyceryl trinitrate ointment (Rectogesic). Although effective, they are dose dependent. Disabling headaches are common at higher doses, making patient compliance with the treatment unreliable.
Topical calcium channel blockers, including nifedipine or diltiazem ointment, are as effective as nitrate ointments but with significantly less side effects. Examples include topical nifedipine 0.3% with lidocaine 1.5% ointment and diltiazem 2% ointment.
Combination of medical therapies may offer up to 98% cure rates.
A combined surgical and pharmacologic treatment, administered by colorectal surgeons, is periodic direct injection of botulinum toxin (Botox) into the anal sphincter to relax it. Oftentimes, these injections prove less and less potent with each application. With patients spending thousands of dollars and not achieving a permanent cure, they oftentimes elect to have surgery.
When conservative medical therapy fails, surgery is considered.
Preoperative Planning
Mechanical bowel preparation is not necessary.
Fleet enemas are prescribed for the night before and the morning of surgery to clear the rectal vault.
Intravenous cefoxitin is administered within 1 hour of skin incision.
A preoperative time-out and briefing is conducted with the entire surgical team in attendance.
An anal block with bupivacaine extended-release liposome injection is associated with both pain relief for 72 hours and a 45% reduction in total opioid consumption at 72 hours.
Positioning
The patient is placed supine on a modified lithotomy position with the legs on padded stirrups to prevent neurovascular injuries to the calves (FIG 2).
Alternatively, the patient can be placed in a prone jackknife position on a split-leg table, with the surgeon positioned between the legs (FIG 3). The buttocks are spread apart with tape.
The author prefers to perform these procedures under general anesthesia.
Using headlights is critical for good visualization.
 FIG 2 • Modified lithotomy position. The legs are placed on stirrups with padding to help prevent neurovascular injuries. |
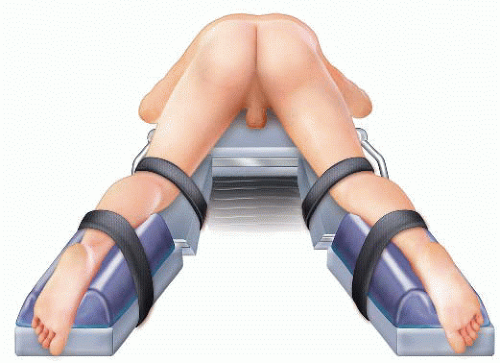 FIG 3 • Prone jackknife position. The lower extremities are placed on a split-leg table position to allow the surgeon to operate from in between the patient’s legs. |
TECHNIQUES
CLOSED LATERAL INTERNAL SPHINCTEROTOMY (TRANSCUTANEOUS)
Using lubrication, perform a gentle anal dilation with two fingers.
An anoscope is used to confirm the presence of the anal fissure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree