KEY POINTS
Surgery of the hand is a regional specialty, integrating components of neurologic, orthopedic, plastic, and vascular surgery.
Understanding hand anatomy is the key to proper diagnosis of injury, infection, and degenerative disease of the hand.
After evaluation and/or treatment, patients should be splinted to protect the injured digits and keep the collateral ligaments of the injured joints on tension (metacarpophalangeal joints flexed, interphalangeal joints extended).
Healing of an injured or diseased structure in the hand is not the endpoint of treatment; the goal of any intervention must be to obtain structure healing, relief of pain, and maximization of function.
If a patient managed conservatively for cellulitis does not improve within 24 to 48 hours of appropriate intravenous antibiotics, abscess must be suspected.
Clinical examination, particularly noting the area of greatest tenderness and/or inflammation, is the most useful diagnostic tool for hand infections.
INTRODUCTION
The highly mobile, functional, and strong hand is a major distinguishing point between humans and the nonhuman primates. The hand is an essential participant for activities of daily living, vocation, and recreational activities. The hand is even adaptable enough to read for the blind and speak for the mute. The underlying goal of all aspects of hand surgery is to maximize mobility, sensibility, stability, and strength while minimizing pain. These goals are then maximized to the extent possible given the patient’s particular pathology. Hand surgery is a regional specialty. Hand surgeons integrate components of neurologic, orthopedic, plastic, and vascular surgery in the care of patients with disorders of the upper extremities.
ANATOMY OF THE HAND AND WRIST
In order to understand any disorder of the hand, one must understand the anatomy of the underlying structures. Examination of the hand is based on demonstrating the function or lack thereof of each of these structures.
The hand is highly mobile in space to allow maximum flexibility in function. As such, a number of directions particular to the hand are necessary in order to properly describe position, motion, and so on.1 Palmar (or volar) refers to the anterior surface of the hand in the anatomic position; dorsal refers to the posterior surface in the anatomic position. The hand can rotate at the wrist level; rotation to bring the palm down is called pronation, rotation to bring the palm up is called supination. Because the hand can rotate in space, the terms medial and lateral are avoided. Radial and ulnar are used instead as these terms do not vary with respect to the rotational position of the hand. Abduction and adduction, when used on the hand, refer to movement of the digits away from and toward the middle finger, respectively (Fig. 44-1).
The hand is comprised of 19 bones arranged in five rays.2 A ray is defined as a digit (finger or thumb) from the metacarpal base to the tip of the digit (Fig. 44-2A). The rays are numbered 1 to 5, beginning with the thumb. By convention, however, they are referred to by name: thumb, index, middle, ring, and small. There are five metacarpals, comprising the visible palm of the hand. Each digit has a proximal and a distal phalanx, but only the fingers have a middle phalanx as well. The metacarpophalangeal (MP) joint typically allows 90° of flexion with a small amount of hyperextension. In addition, the fingers can actively abduct (move away from the middle finger) and adduct (move toward the middle finger). The thumb, in contrast, moves principally in the flexion-extension arc at the MP joint. Although there can be laxity in the radial and ulnar direction, the thumb cannot actively move in these directions at the MP level. The proximal interphalangeal joint (PIP) is the critical joint for finger mobility. Normal motion is 0 to 95° (full extension to flexion). The distal interphalangeal joint (DIP) also moves only in a flexion-extension plane from 0 to 90° on average. The thumb interphalangeal joint (IP) also moves only in a flexion-extension plane. Its normal motion is highly variable between individuals, but averages 0 to 80°.
Figure 44-2.
Bony architecture of the hand and wrist. A. Bones of the hand and digits. All rays have metacarpophalangeal (MP) joints. The fingers have proximal and distal interphalangeal joints (PIP and DIP), but the thumb has a single interphalangeal (IP) joint. B. Bones of the wrist. The proximal row consists of the scaphoid, lunate, and capitate. The distal row bones articulate with the metacarpals: the trapezium with the thumb, the trapezoid with the index, the capitate with the middle, and the hamate with the ring and small. The pisiform bone is a sesamoid within the flexor carpi ulnaris tendon. It overlaps the triquetrum and hamate but does not contribute to a carpal row. CMC = carpometacarpal; TFCC = triangular fibrocartilage complex.
Each of the MP and IP joints has a radial and ulnar collateral ligament to support it. The IP joint collateral ligaments are on tension with the joint fully extended. For the fingers, the MP joint collateral ligaments are on tension with the joint bent 90°. Collateral ligaments have a tendency to contract when not placed on tension; this becomes relevant when splinting the hand (see later Trauma section on splinting).
The wrist consists of eight carpal bones divided into two rows (Fig. 44-2B).2 The proximal row consists of the scaphoid, lunate, and triquetrum. The lunate is the principle axis of motion of the hand onto the forearm. It bears approximately 35% of the load of the wrist onto the forearm. The scaphoid is shaped like the keel of a boat and bears 55% of the load of the hand onto the forearm, but also serves as the principle link between the proximal and distal rows, allowing for motion while maintaining stability. Both the scaphoid and the lunate articulate with the radius. The triquetrum resides ulnar to the lunate. It does not interact with the ulna proximally; rather, it interacts with a cartilage suspended between the ulnar styloid and the distal radius called with triangular fibrocartilage complex (TFCC) (Fig. 44-2B). The remaining 10% of load of the hand onto the forearm is transmitted through the TFCC.3
The distal row consists of four bones. The trapezium resides between the scaphoid and the thumb metacarpal. Distally, it has a saddle-shaped surface, which interacts with a reciprocally saddle-shaped base of the thumb metacarpal to allow for high mobility of the thumb carpometacarpal (CMC) joint in radial-ulnar and palmar-dorsal directions and opposition (Fig. 44-1B). The trapezoid rests between the scaphoid and the index finger metacarpal. The capitate, the largest carpal bone and first to ossify in a child, lies between the lunate and the middle finger metacarpal, but also interacts with the scaphoid on its proximal radial surface. The index and middle finger CMC joints are highly stable and have minimal mobility. The hamate is the ulnar-most bone in the distal row, sitting between the triquetrum proximally and the ring and small finger metacarpals distally. The ring and small finger CMC joints are mobile, principally in the flexion-extension direction.
The pisiform is a carpal bone only by geography. It is a sesamoid bone within the FCU tendon (see below). It does not bear load and can be excised, when necessary, without consequence.
The wrist is moved by multiple tendons that originate from the forearm and elbow. The digits of the hand are moved by both intrinsic (originating within the hand) and extrinsic (originating in the forearm) muscles. All of these muscles are innervated by the median, radial, or ulnar nerves (or their branches) (Fig. 44-3).
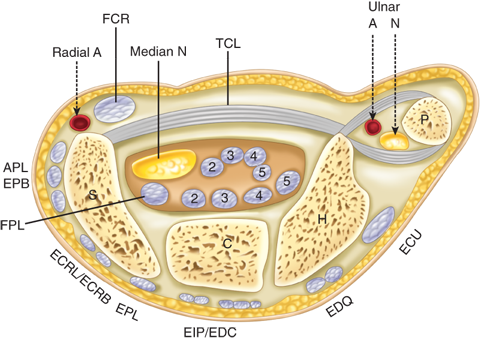
Figure 44-3.
Cross-section of the wrist at the midcarpal level. The relative geography of the neurologic and tendinous structures can be seen. The transverse carpal ligament (TCL) is the roof of the carpal tunnel, passing volar to the median nerve and long flexor tendons. The TCL is also the floor of the ulnar tunnel, or Guyon’s canal, passing dorsal to the ulnar artery and nerve. The wrist and digital extensor tendons are also seen, distal to their compartments on the distal radius and ulna. Bones: C = capitate; H = hamate; P = pisiform; S = scaphoid. Tendons (flexor digitorum superficialis is volar to flexor digitorum profundus within the carpal tunnel): 2 = index finger; 3 = middle finger; 4 = ring finger; 5 = small finger. A = artery; APL = abductor pollicis longus; ECRB = extensor carpi radialis brevis; ECRL = extensor carpi radialis longus; ECU = extensor carpi ulnaris; EDC = extensor digitorum communis; EDQ = extensor digiti quinti; EIP = extensor indices proprius; EPB = extensor pollicis brevis; EPL = extensor pollicis longus; FCR = flexor carpi radialis; FPL = flexor pollicis longus; N = nerve.
Three muscles flex the wrist, all of which originate from the medial epicondyle of the humerus. The flexor carpi radialis (FCR, median nerve) inserts on the volar base of the index finger metacarpal. The flexor carpi ulnaris (FCU, ulnar nerve) also originates from the proximal ulna and inserts on the volar base of the small finger metacarpal. The palmaris longus (PL) tendon does not insert on a bone; it inserts on the palmar fascia, located deep to the skin in the central proximal palm, and is absent in up to 15% of patients. The FCR also deviates the wrist radially, whereas the FCU deviates the wrist ulnarly.
All three wrist extensors are innervated by the radial nerve or its branches. The extensor carpi radialis longus (ECRL) originates from the distal shaft of the humerus and inserts on the dorsal base of the index finger metacarpal. The extensor carpi radialis brevis (ECRB) originates from the lateral epicondyle of the humerus and inserts on the dorsal base of the middle finger metacarpal. The extensor carpi ulnaris (ECU) also originates from the lateral epicondyle of the humerus and inserts on the dorsal base of the small finger metacarpal. The ECRL deviates the wrist radially, whereas the ECU deviates the wrist ulnarly.
The long flexors of the fingers all originate from the medial epicondyle of the humerus. The flexor digitorum superficialis (FDS) inserts on the base of the middle phalanx of each finger and primarily flexes the PIP joint. The flexor digitorum profundus (FDP) inserts on the base of the distal phalanx and primarily flexes the DIP joint. The flexor pollicis longus (FPL) originates more distally, from the ulna, radius, and interosseous membrane between them in the forearm. It inserts on the base of the distal phalanx of the thumb and primarily flexes the IP joint. All of these tendons can also flex the more proximal joint(s) in their respective rays. All of these muscles are innervated by the median nerve (or its branches) except the FDP to the ring and small fingers, which are innervated by the ulnar nerve.
The extrinsic extensors of the fingers and thumb are all innervated by the posterior interosseous nerve (PIN, branch of the radial nerve). The extensor digitorum communis (EDC) originates from the lateral epicondyle of the humerus and extends the MP joints of the fingers. Unlike most tendons that attach directly into a bone, the EDC tendons do not insert on the dorsal base of the proximal phalanx, but rather into a soft tissue sling called the sagittal hood, which surrounds the proximal phalanx base and pulls up on the volar surface in a hammock-like manner. More distally in the dorsal forearm, the extensor indices proprius (EIP) and extensor digiti quinti (EDQ) originate from the ulna, radius, and posterior interosseous membrane and insert on the sagittal hood of the index and small fingers, respectively.
The thumb has three separate extrinsic extensors. All of these originate from the dorsal ulna in the mid-forearm and are innervated by the PIN. The abductor pollicis longus (APL) inserts on the radial base of the thumb metacarpal to produce some extension, but mostly abduction. The extensor pollicis brevis (EPB) inserts on the base of the thumb proximal phalanx. The extensor pollicis longus (EPL) inserts on the base of the thumb distal phalanx.
The intrinsic muscles of the hand are what allow humans fine, subtle movements of the hand. Microsurgery, typing, and even video gaming would be difficult, if not impossible, without them.
The thenar muscles originate from the volar radial surface of the scaphoid and trapezium and the flexor retinaculum. The abductor pollicis brevis (APB) inserts on the radial base of the thumb proximal phalanx and abducts the thumb in a radial and volar direction. The opponens pollicis (OP) inserts on the radial distal aspect of the thumb metacarpal and draws the thumb across the palm toward the small finger. The flexor pollicis brevis (FPB) inserts on the base of the thumb proximal phalanx and flexes the thumb MP joint. The APB, OP, and superficial head of the FPB are all innervated by the thenar motor branch of the median nerve.
The lumbrical muscles are unique in the body in that they originate from a tendon. Each finger’s lumbrical originates from the FDP tendon in the palm. The lumbrical tendon passes along the radial aspect of the digit to flex the MP and extend the IP joints. The index and middle lumbricals are median nerve innervated, and the ring and small finger lumbricals are ulnar nerve innervated.
The hypothenar muscles originate from the pisiform, hamate, and flexor retinaculum and insert on the ulnar base of the small finger proximal phalanx. The abductor digiti quinti (ADQ) abducts the small finger. The opponens digiti quinti (ODQ) brings the small finger across the palm in reciprocal motion to the OP. The flexor digiti quinti (FDQ) flexes the small finger metacarpal. All of these muscles are innervated by the ulnar nerve.
The interosseous muscles occupy the space between the metacarpal bones. Their tendons insert on the bases of the proximal phalanges. All act to flex the MP joints and extend the IP joints. The three palmar interosseous muscles adduct the fingers. The four dorsal interosseous muscles abduct the fingers. The adductor pollicis originates from the middle finger metacarpal and inserts on the ulnar base of the thumb proximal phalanx. It acts to adduct the thumb. All of these muscles, as well as the deep head of the FPB, are innervated by the ulnar nerve.
Multiple pulleys pass over or surround the extrinsic tendons en route to or within the hand. There purpose is to maintain tendon position near the bone, allowing maximal translation of tendon excursion into joint motion.
The most well known of the wrist-level pulleys is the flexor retinaculum, also known as the transverse carpal ligament. It attaches to the scaphoid tubercle and trapezium radially and the hook of the hamate bone and pisiform ulnarly. Deep to this ligament, between the scaphoid (radially) and the hamate (ulnarly), pass the FDS, FDP, and FPL tendons as well as the median nerve. This area is also known as the carpal tunnel (see Fig. 44-3).
On the dorsum of the wrist, the extensor retinaculum is divided into six compartments. Beginning on the radial aspect of the radius, the first compartment contains the APL and EPB tendons. The second holds the ECRL and ECRB tendons. The EPL passes through the third compartment. The fourth compartment contains the EIP and EDC tendons, the fifth the EDQ, and the sixth the ECU. The sixth compartment is located on the ulnar aspect of the distal ulna. Although the compartments end at the radiocarpal/ulnocarpal joints, the relative geography of the tendons is preserved over the carpal bones (see Fig. 44-3).
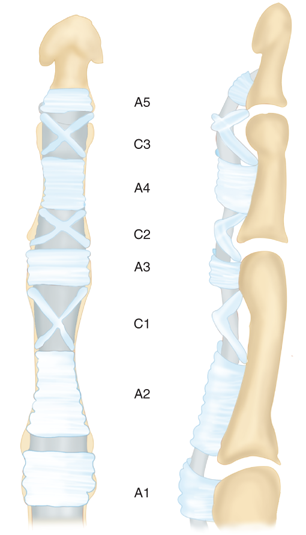
In the hand, the pulleys maintain the long flexor tendons in close apposition to the fingers and thumb. There are no extensor pulleys within the hand. Each finger has five annular and three cruciate pulleys (Fig. 44-4). The second and fourth (A2 and A4) pulleys are the critical structures to prevent bowstringing of the finger.4 The remaining pulleys can be divided as needed for surgical exposure or to relieve a stricture area.
Two major arteries serve the hand. The radial artery travels under the brachioradialis muscle in the forearm. At the junction of the middle and distal thirds of the forearm, the artery becomes superficial and palpable, passing just radial to the FCR tendon. At the wrist level, the artery splits into two branches. The smaller, superficial branch passes volarly into the palm to contribute to the superficial palmar arch. The larger branch passes dorsally over the scaphoid bone, under the EPL and EPB tendons (known as the anatomic snuffbox) and back volarly between the proximal thumb and index finger metacarpals to form the superficial palmar arch.
The ulnar artery travels deep to the FCU muscle in the forearm. When the FCU becomes tendinous, the ulnar artery resides deep and slightly radial to it. At the wrist, the artery travels between the hamate and pisiform bones superficial to the transverse carpal ligament (known as Guyon’s canal) into the palm. The larger, superficial branch forms the superficial palmar arch. The deeper branch contributes to the deep palmar arch (Fig. 44-5A). In 97% of patients, at least one of the deep or superficial palmar arches is intact, allowing for the entire hand to survive on the radial or ulnar artery.5
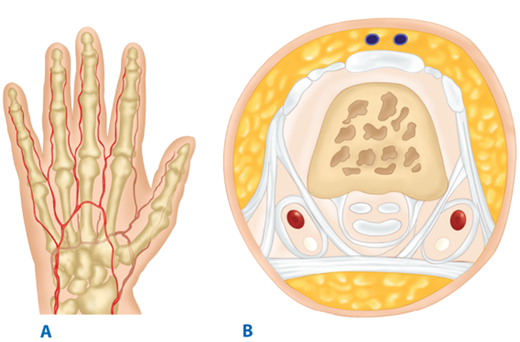
Figure 44-5.
Arteries of the hand and finger. A. Relative position of the superficial and deep palmar arches to the bony structures and each other; note the radial artery passes dorsal to the thumb metacarpal base, through the first web space, and anterior to the index metacarpal base as it forms the deep arch. B. The neurovascular bundles lay volar to the midaxis of the digit with the artery dorsal to the nerve; Grayson’s ligament (volar) and Cleland’s ligament (dorsal) connect the bone to the skin surrounding the bundle.
Each digit receives a radial and ulnar digital artery. For the thumb, the radial digital artery may come from the deep palmar arch or the main body of the radial artery. The larger ulnar digital artery comes off the deep arch as either a discrete unit, the princeps pollicis artery, or less frequently as the first common digital artery, which then splits into the radial digital artery to the index finger and the ulnar digital artery to the thumb. The second, third, and fourth digital arteries typically branch off the superficial palmar arch and pass over the similarly named interosseous spaces respectively, ultimately dividing into two proper digital arteries each. The ulnar digital artery of the small finger comes off as a separate branch from the superficial arch. Within the finger, the proper digital arteries travel lateral to the bones and tendons, just palmar to the midaxis of the digit, but dorsal to the proper digital nerves (Fig. 44-5B).
Three principal nerves serve the forearm, wrist, and hand: the median, radial, and ulnar nerves. The most critical of these from a sensory standpoint is the median nerve. The median nerve begins as a terminal branch of the medial and lateral cords of the brachial plexus. It receives fibers from C5–T1. The palmar cutaneous branch of the median nerve separates from the main body of the nerve 6 cm proximal to the volar wrist crease and serves the proximal, radial-sided palm. The main body of the median nerve splits into several branches after the carpal tunnel: a radial digital branch to the thumb, an ulnar digital nerve to the thumb, and a radial digital nerve to the index finger (sometimes beginning as a single first common digital nerve); the second common digital nerve that branches into the ulnar digital nerve to the index finger and the radial digital nerve to the middle finger; and a third common digital nerve that branches into the ulnar digital nerve to the middle finger and a radial digital nerve to the ring finger. The digital nerves provide volar-sided sensation from the metacarpal head level to the tip of the digit. They also, through their dorsal branches, provide dorsal-sided sensation to the digits from the midportion of the middle phalanx distally via dorsal branches. The thenar motor branch of the median nerve most commonly passes through the carpal tunnel and then travels in a recurrent fashion back to the thenar muscles. Less commonly, the nerve passes through or proximal to the transverse carpal ligament en route to its muscles.
In the forearm, the median nerve gives motor branches to all of the flexor muscles except the FCU, and the ring and small finger portions of the FDP. Distal median motor fibers (with the exception of those to the thenar muscles) are carried through a large branch called the anterior interosseous nerve.
The ulnar nerve is a terminal branch of the medial cord of the brachial plexus. It receives innervation from C8 and T1 roots. The FCU and FDP (ring/small) receive motor fibers from the ulnar nerve. In the distal forearm, 5 cm above the head of the ulna, the nerve gives off a dorsal sensory branch. Once in the hand, the nerve splits into the motor branch and sensory branches. The motor branch curves radially at the hook of the hamate bone to innervate the intrinsic muscles, as described earlier. The sensory branches become the ulnar digital nerve to the small finger and the fourth common digital nerve, which splits into the ulnar digital nerve to the ring finger and the radial digital nerve to the small finger. The sensory nerves provide distal dorsal sensation similar to the median nerve branches.
The radial nerve is the larger of two terminal branches of the posterior cord of the brachial plexus. It receives fibers from C5–T1 nerve roots. It innervates all of the extensor muscles of the forearm and wrist through the PIN branch except for the ECRL, which is innervated by the main body of the radial nerve in the distal upper arm. There is no ulnar nerve contribution to extension of the wrist, thumb, or finger MP joints. As noted earlier, the ulnar innervated intrinsic hand muscles are the principle extensors of the finger IP joints, although the long finger extensors (EDC, EIP, EDQ) make a secondary contribution to this function.
In the proximal dorsal forearm, the superficial radial nerve (SRN) is the other terminal branch of the radial nerve. It travels deep to the brachioradialis muscle until 6 cm proximal to the radial styloid, where it becomes superficial. The SRN provides sensation to the dorsal hand and the radial three and a half digits up to the level of the mid-middle phalanx (where the dorsal branches of the proper digital nerves take over, as described earlier). The dorsal branch of the ulnar nerve provides sensation to the ulnar one and a half digits and dorsal hand in complement to the SRN.
HAND EXAMINATION
A common scenario in which the hand surgeon will be introduced to the patient is in trauma or other acute situations. The patient is evaluated by inspection, palpation, and provocative testing.
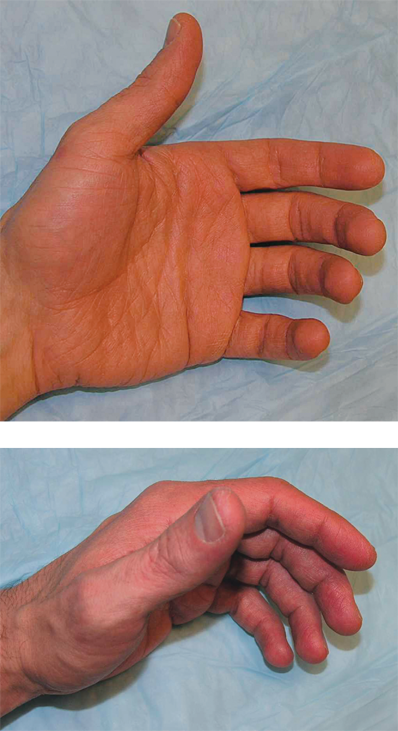
On inspection, one should first note the position of the hand. The resting hand has a normal cascade of the fingers, with the small finger flexed most and the index finger least (Fig. 44-6). Disturbance of this suggests a tendon or skeletal problem. Also note any gross deformities or wounds and what deeper structures, if any, are visible in such wounds. Observe for abnormal coloration of a portion or all of the hand (this can be confounded by ambient temperature or other injuries), edema, and/or clubbing of the fingertips.
Palpation typically begins with the radial and ulnar artery pulses at the wrist level. Pencil Doppler examination can supplement this and evaluate distal vessels. A pulsatile signal is normally detectable by pencil Doppler in the pad of the finger at the center of the whorl of creases. Discrepancies between digits should be noted. If all other tests are inconclusive, pricking the involved digit with a 25-gauge needle should produce bright red capillary bleeding. If an attached digit demonstrates inadequate or absent blood flow (warm ischemia), the urgency of completing the evaluation and initiating treatment markedly increases.
Sensation must be evaluated prior to any administration of local anesthetic. At a minimum, light and sharp touch sensation should be documented for the radial and ulnar aspects of the tip of each digit. Beware of writing “sensation intact” at the conclusion of this evaluation. Rather, one should document what was tested (e.g., “light and sharp touch sensation present and symmetric to the tips of all digits of the injured hand”). In the setting of a sharp injury, sensory deficit implies a lacerated structure until proven otherwise. Once sensation has been evaluated and documented, the injured hand can be anesthetized for patient comfort during the remainder of the examination (see below).
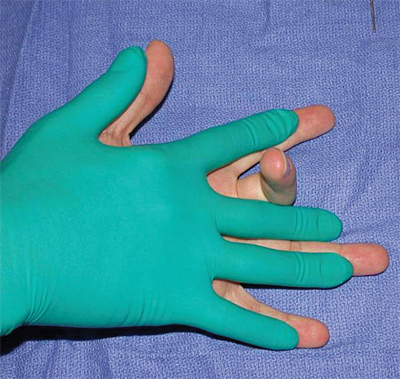
Ability to flex and extend the wrist and digital joints is typically examined next. At the wrist level, the FCR and FCU tendons should be palpable during flexion. The wrist extensors are not as readily palpated due to the extensor retinaculum. Ability to flex the DIP joint (FDP) is tested by blocking the finger at the middle phalanx level. To test the FDS to each finger, hold the remaining three fingers in slight hyperextension and ask the patient to flex the involved digit (Fig. 44-7). This maneuver makes use of the fact that the FDP tendons share a common muscle belly. Placing the remaining fingers in extension prevents the FDP from firing, and allows the FDS, which has a separate muscle belly for each tendon, to fire. Strength in grip, finger abduction, and thumb opposition is tested and compared to the uninjured side. Range of motion for the wrist, MP, and IP joints should be noted and compared to the opposite side.
If there is suspicion for closed space infection, the hand should be evaluated for erythema, swelling, fluctuance, and localized tenderness. The dorsum of the hand does not have fascial septae; thus dorsal infections can spread more widely than palmar ones. The epitrochlear and axillary nodes should be palpated for enlargement and tenderness. Findings for specific infectious processes will be discussed in the Infections section.
Additional exam maneuvers and findings, such as those for office consultations, will be discussed with each disease process covered later in this chapter.
HAND IMAGING
Almost every hand evaluation should include plain X-rays of the injured or affected part. A standard, anteroposterior, lateral, and oblique view of the hand or wrist (as appropriate) is rapid, inexpensive, and usually provides sufficient information about the bony structures to achieve a diagnosis in conjunction with the symptoms and findings.6
Lucencies within the bone should be noted. Most commonly, these represent fractures, but they can on occasion represent neoplastic or degenerative processes. Great care should be taken to evaluate the entire X-ray, typically beginning away from the area of the patient’s complaint. Additional injuries can be missed, which might affect the treatment plan selected and eventual outcome.
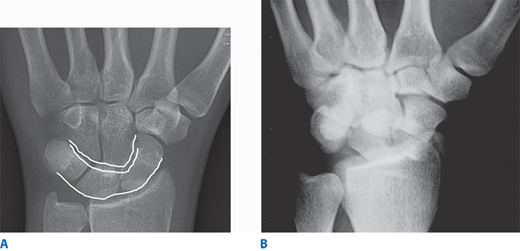
Congruency of adjacent joints should also be noted. The MP and IP joints of the fingers should all be in the same plain on any given view. Incongruency of the joint(s) of one finger implies fracture with rotation. At the wrist level, the proximal and distal edge of the proximal row and proximal edge of the distal row should be smooth arcs,7 known as Gilula’s arcs (Fig. 44-8A). Disruption of these implies ligamentous injury or possibly dislocation (Fig. 44-8B).
Computed tomography (CT) scanning of the hand and wrist can provide additional bony information when plain X-rays are insufficient. Comminuted fractures of the distal radius can be better visualized for number and orientation of fragments. Scaphoid fractures can be evaluated for displacement and comminution preoperatively as well as for the presence of bony bridging postoperatively (Fig. 44-9). CT scans are also useful for CMC fractures of the hand where overlap on a plain X-ray lateral view may make diagnosis difficult.
Figure 44-9.
A. Preoperative images demonstrate a nonunion of a scaphoid fracture sustained 4 years earlier. Postoperatively, cross-sectional imaging with a computed tomography scan in the coronal plan demonstrates bone crossing the previous fracture line. This can be difficult to discern on plain X-rays due to overlap of bone fragments.
Unlike the trunk and more proximal extremities, CT scans with contrast are less useful to demonstrate abscess cavities due to the small area of these spaces.
Ultrasonography has the advantages of being able to demonstrate soft tissue structures and being available on nights and weekends. Unfortunately, it is also highly operator dependent. In the middle of the night when magnetic resonance imaging (MRI) is not available, ultrasound may be able to demonstrate a large deep infection in the hand but is rarely more useful than a thorough clinical examination.
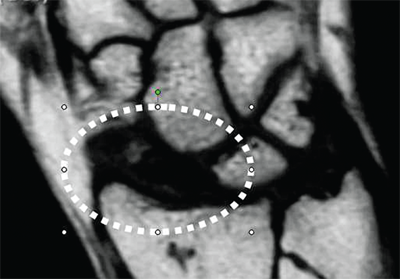
MRI provides the best noninvasive visualization of the soft tissue structures. With contrast, MRI can demonstrate an occult abscess. Unfortunately, it is often not available on an urgent basis for hand issues when this information is often needed. MRI can also demonstrate soft tissue injuries such as cartilage or ligament tears or tendonitis (usually by demonstrating edema in the area in question). It can demonstrate occult fractures that are not sufficiently displaced to be seen on X-ray or CT (again, by demonstrating edema). MRI can also demonstrate vascular disturbance of a bone, as in a patient with avascular necrosis of the scaphoid (Fig. 44-10).
Angiography of the upper extremity is rarely used. In many centers, MRI and CT angiography provide sufficient resolution of the vascular structures to make traditional angiography unnecessary. Also, primary vascular disease of the upper extremity is relatively uncommon. In the trauma setting, vascular disturbance usually mandates exploration and direct visualization of the structures in question, and angiography is thus obviated.
For a patient with vascular disease of the upper extremity, angiography of the upper extremity is usually performed through a femoral access much like with the leg. An arterial catheter can be used to deliver thrombolytic drugs to treat a thrombotic process.
TRAUMA
The upper extremity–injured patient may have additional injuries to other parts of the body. All injured patients should receive an appropriate trauma survey to look for additional injuries.
The patient with upper extremity trauma is evaluated as described in the Hand Examination section. Sensory examination should be performed early. Once sensory status has been documented, administration of local anesthesia can provide comfort to the patient during the remainder of the evaluation and subsequent treatment. Patients should receive tetanus toxoid for penetrating injuries if more than 5 years have passed since the last vaccination.
Anesthetic blockade can be administered at the wrist level, digital level, or with local infiltration as needed. Keep in mind that all local anesthetics are less effective in areas of inflammation.
The agents most commonly used are lidocaine and bupivacaine. Lidocaine has the advantage of rapid onset, whereas bupivacaine has the advantage of long duration (average 6– 8 hours).8 Although bupivacaine can produce irreversible heart block in high doses, this is rarely an issue with the amounts typically used in the hand. For pediatric patients, the tolerated dose is 2.5 mg/kg. This can be easily remembered by noting that when using 0.25% bupivacaine, 1 mL/kg is acceptable dosing.
A commonly held axiom is that epinephrine is unacceptable to be used in the hand. Several recent large series have dispelled this myth.9 Epinephrine should not be used in the fingertip and not in concentrations higher than 1:100,000 (i.e., what is present in commercially available local anesthetic with epinephrine). Beyond that, its use is acceptable and may be useful in an emergency room (ER) where tourniquet control may not be available. Also, because most ER procedures are done under pure local anesthesia, many patients will not tolerate the discomfort of the tourniquet beyond 30 minutes.10 Epinephrine will provide hemostasis and also prolong the effect of the local anesthetic.
Simple lacerations, particularly on the dorsum of the hand, can be anesthetized with local infiltration. This is performed in the standard fashion.
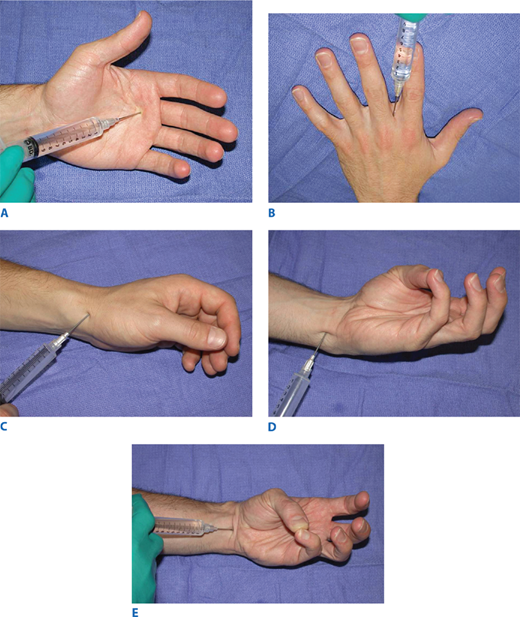
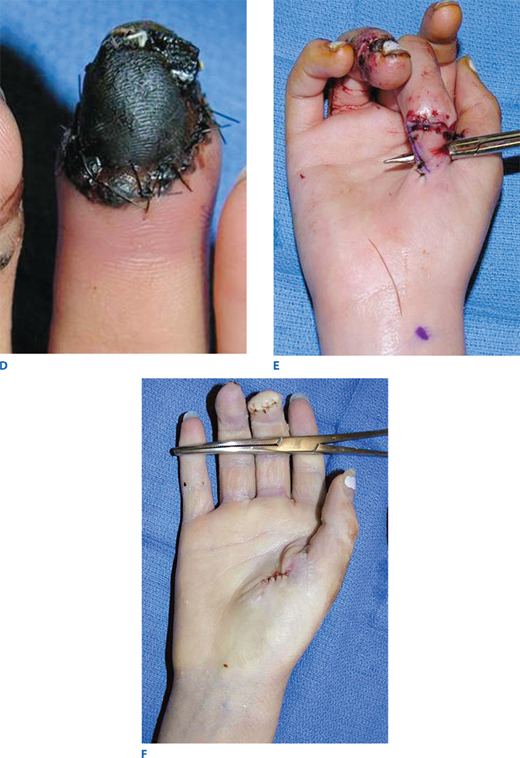
Blocking of the digital nerves at the metacarpal head level is useful for volar injuries distal to this point and for dorsal injuries beyond the midpoint of the middle phalanx (via dorsal branches of the proper digital nerves). Fingertip injuries are particularly well anesthetized by this technique. A digit can be anesthetized via a flexor sheath approach or via the dorsal web space (Fig. 44-11A,B).
Figure 44-11.
Local anesthesia can be administered at the digital or the wrist level. A. A single injection into the flexor tendon sheath at the metacarpal head level provides complete anesthesia for the digit. B. Alternatively, one can inject from a dorsal approach into the web space on either side. C. The superficial radial nerve is blocked by infiltrating subcutaneously over the distal radius from the radial artery pulse to the distal radioulnar joint. The dorsal sensory branch of the ulnar nerve is blocked in similar fashion over the distal ulna. D. To block the ulnar nerve, insert the needle parallel to the plane of the palm and deep to the flexor carpi ulnaris tendon; aspirate to confirm the needle is not in the adjacent ulnar artery. E. To block the median nerve, insert the needle just ulnar to the palmaris longus tendon into the carpal tunnel. One should feel two points of resistance: one when piercing the skin, the second when piercing the antebrachial fascia.
Blocking one or more nerves as they cross the wrist can provide several advantages: anesthesia for multiple injured digits, avoiding areas of inflammation where the local anesthetic agent may be less effective, and avoiding injection where the volume of fluid injected may make treatment harder (such as fracture reduction). Four major nerves cross the wrist: the median nerve, SRN, ulnar nerve, and dorsal sensory branch of the ulnar nerve (Fig. 44-11C–E). When blocking the median and ulnar nerves, beware of intraneural injection, which can cause irreversible neural scarring. If the patient complains of severe paresthesias with injection or high resistance is encountered, the needle should be repositioned.
For dislocations and displaced fractures, a visible deformity is often present. Nondisplaced fractures may not show a gross deformity but will have edema and tenderness to palpation at the fracture site. A fracture is described by its displacement, rotation, and angulation. A fracture is also described in terms of comminution and the number and complexity of fracture fragments. Displacement is described as a percentage of the diameter of the bone; rotation is described in degrees of supination or pronation with respect to the rest of the hand; angulation is described in degrees. To avoid confusion, it is useful to describe which direction the angle of the fracture points. All injuries should be evaluated for nearby wounds (open) that may introduce bacteria into the fracture site or joint space.
Once the initial force on the fracture ceases, the tendons passing beyond the fracture site provide the principal deforming force. Their force is directed proximally and, to a lesser extent, volarly. Based on this, the stability of a fracture can be determined by the orientation of the fracture with respect to the shaft of the bone. Transverse fractures are typically stable. Oblique fractures typically shorten. Spiral fractures typically rotate as they shorten and thus require surgical treatment.
Fractures of the tuft of the distal phalanx are common. Catching of a finger in a closing door is a common causative mechanism. These fractures are often nondisplaced and do not require treatment beyond protection of the distal phalanx from additional trauma while the fracture heals.
Displaced transverse fractures of the phalanges can usually be reduced with distraction. The distal part is pulled away from the main body of the hand and then pushed in the direction of the proximal shaft of the finger, and then distraction is released. Postreduction X-rays should routinely be performed to document satisfactory reduction. Oblique and spiral fractures usually are unstable after reduction. The involved digit(s) should be splinted until appropriate surgical intervention can be performed.
Articular fractures of the IP and MP joints are worrisome because they may compromise motion. Chip fractures must be evaluated for instability of the collateral ligaments. If the joint is stable, the patient should initially be splinted for comfort. Motion therapy should be instituted early (ideally within the first week) to prevent stiffness. For larger fractures, the patient should be splinted until surgical treatment can be performed. In surgery, the fracture is typically internally fixated to allow for early motion, again with the goal of preventing stiffness.11
Dislocations of the PIP joints produce traction on the neurovascular structures but usually do not lacerate them. In general, the patient should not be sent home with a joint that remains dislocated. Most commonly, the distal part is dorsal to the proximal shaft and sits in a hyperextended position. For this patient, the examiner gently applies pressure to the base of the distal part until it passes beyond the head of the proximal phalanx. Once there, the relocated PIP joint is gently flexed, confirming the joint is in fact reduced. The joint is splinted in slight flexion to prevent redislocation. On occasion, the head of the proximal phalanx may pass between the two slips of the FDS tendon. For these patients, the joint may not be reducible in a closed fashion.
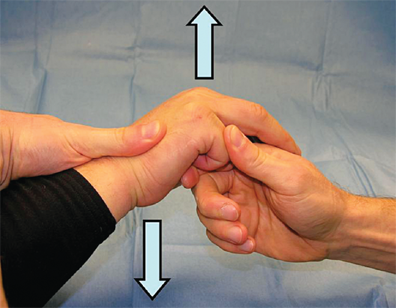
Angulated fractures of the small finger metacarpal neck (“boxer’s fracture”) are another common injury seen in the ER. Typical history is that the patient struck another individual or rigid object with a hook punch. These are often stable after reduction using the Jahss maneuver (Fig. 44-12).
Figure 44-12.
The Jahss maneuver. The surgeon fully flexes the patient’s small finger into the palm and secures it in his distal hand. The proximal hand controls the wrist and places the thumb on the patient’s fracture apex (the most prominent dorsal point). The examiner distracts the fracture, pushes dorsally with the distal hand (up arrow), and resists dorsal motion with the proximal hand (down arrow).
Fractures of the thumb metacarpal base are often unstable. The Bennett fracture displaces the volar-ulnar base of the bone. The remainder of the articular surface and the shaft typically dislocate dorsoradially and shorten. The thumb often appears grossly shortened, and the proximal shaft of the metacarpal may reside at the level of the trapezium or even the scaphoid on X-ray. In a Rolando fracture, a second fracture line occurs between the remaining articular surface and the shaft. These fractures nearly always require open reduction and internal fixation.
Most nondisplaced fractures do not require surgical treatment. The scaphoid bone of the wrist is a notable exception to this rule. Due to peculiarities in its vascular supply, particularly vulnerable at its proximal end, nondisplaced scaphoid fractures can fail to unite in up to 20% of patients even with appropriate immobilization. Recent developments in hardware and surgical technique have allowed stabilization of the fracture with minimal surgical exposure. One prospective randomized series of scaphoid wrist fractures demonstrated shortening of time to union by up to 6 weeks in the surgically treated group, but no difference in rate of union.12 Surgery may be useful in the younger, more active patient who would benefit from an earlier return to full activity.
Ligament injuries of the wrist can be difficult to recognize. Patients often present late and may not be able to localize their pain. In severe cases, the ligaments of the wrist can rupture to the point of dislocation of the capitate off the lunate or even the lunate off the radius. Mayfield and colleagues classified the progression of this injury into four groups.13 In the most severe group, the lunate dislocates off the radius into the carpal tunnel. In some circumstances, the scaphoid bone may break rather than the scapholunate ligament rupturing. Attention to the congruency or disruption of Gilula’s arcs will help the examiner to recognize this injury. For patients with type 4 (most severe) and some with type 3 injury, the examiner should also evaluate for sensory disturbance in the median nerve distribution because this may indicate acute carpal tunnel syndrome and necessitate more urgent intervention. Although the Mayfield pattern of injury is most common, force can also transmit along alternate paths through the carpus.14
After reduction of fractures and dislocations (as well as after surgical repair of these and many other injuries), the hand must be splinted in a protected position. For the fingers, MP joints should be splinted 90°, and the IP joints at 0° (called the intrinsic plus position). The wrist is generally splinted at 20° extension because this puts the hand in a more functional position. This keeps the collateral ligaments on tension and helps prevent secondary contracture. In general, one of three splints should be used for the ER patient (Fig. 44-13). The ulnar gutter splint uses places plaster around the ulnar border of the hand. It is generally appropriate for small finger injuries only. Dorsal plaster splints can be used for injuries of any of the fingers. Plaster is more readily contoured to the dorsal surface of the hand than the volar surface, particularly in the setting of trauma-associated edema. For thumb injuries, the thumb spica splint is used to keep the thumb radially and palmarly abducted from the hand.
Figure 44-13.
Commons splints used for hand injuries/surgeries. A. Ulnar gutter splint. The ring and small fingers are included. The surgeon pushes on the dorsum of the fingers with the distal hand to produce interphalangeal (IP) joint extension and metacarpophalangeal (MP) joint flexion to 90°, while the proximal hand controls wrist position. B. Dorsal four-finger splint. As with the ulnar gutter splint, finger MP joints are flexed to 90° with IP joints kept fully extended. C. Thumb spica splint. One easy method to fabricate is to place one slab of plaster radially over the wrist and thumb with a second square of plaster over the thenar eminence, which joins the first. In this patient, the IP joint was not included. For injuries at, or distal to, the MP joint, the IP should be included in the splint.
Injuries to the flexor and extensor tendons compromise the mobility and strength of the digits. On inspection, injury is normally suspected by loss of the normal cascade of the fingers. The patient should be examined as described earlier to evaluate for which tendon motion is deficient. If the patient is unable to cooperate, extension of the wrist will produce passive flexion of the fingers and also demonstrate a deficit. This is referred to at the tenodesis maneuver.
Flexor tendon injuries are described based on zones (Fig. 44-14). Up until 40 years ago, zone 2 injuries were always reconstructed and never repaired primarily due to concern that the bulk of repair within the flexor sheath would prevent tendon glide. The work of Dr. Kleinert and colleagues at the University of Louisville changed this “axiom” and established the principle of primary repair and early controlled mobilization postoperatively.15 Flexor tendon injuries should always be repaired in the operating room. Although they do not need to be repaired on the day of injury, the closer to the day of injury they are repaired, the easier it will be to retrieve the retracted proximal end in surgery. The laceration should be washed out and closed at the skin level only using permanent sutures. The hand should be splinted as described earlier; one notable difference is that the wrist should be splinted at slight flexion (about 20°) to help decrease the retracting force on the proximal cut tendon end.
Figure 44-14.
The zones of flexor tendon injury. I. Flexor digitorum superficialis insertion to the flexor digitorum profundus insertion. II. Start of the A1 pulley to the flexor digitorum superficialis insertion. III. End of the carpal tunnel to the start of the A1 pulley. IV. Within the carpal tunnel. V. Proximal to the carpal tunnel.
Extensor tendons do not pass through a sheath in the fingers. As such, bulkiness of repair is less of a concern. With proper supervision/experience and equipment, primary extensor tendon repair can be performed in the ER.
Very distal extensor injuries near the insertion on the dorsal base of the distal phalanx may not have sufficient distal tendon to hold a suture. Closed injuries, called mallet fingers, can be treated with extension splinting of the DIP joint for 6 continuous weeks. For patients with open injuries, a dermatotenodesis suture is performed. A 2-0 or 3-0 suture is passed through the distal skin, tendon remnant, and proximal tendon as a mattress suture. Using a suture of a different color than the skin closing sutures will help prevent removing the dermatotenodesis suture(s) too soon. The DIP joint is splinted in extension.
More proximal injuries are typically repaired with a 3-0 braided permanent suture. Horizontal mattress or figure-of-eight sutures should be used, two per tendon if possible. Great care should be used to ensure matching the appropriate proximal and distal tendon ends. The patient is splinted with IP joints in extension and the wrist in extension per usual. MP joints should be splinted in 45° flexion, sometimes less. Although this position is not ideal for MP collateral ligaments, it is important for taking tension off of the tendon repairs.
In the setting of a sharp injury, a sensory deficit implies a nerve laceration until proven otherwise. For blunt injuries, even displaced fractures and dislocations, nerves are often contused but not lacerated and are managed expectantly. Nerve repairs require appropriate microsurgical equipment and suture; they should not be performed in the ER. As with tendons, nerve injuries do not require immediate exploration. However, earlier exploration will allow for easier identification of structures and less scar tissue to be present. The nerve must be resected back to healthy nerve fascicle prior to repair. Delay between injury and repair can thus make a difference between the ability to repair a nerve primarily or the need to use a graft. The injured hand should be splinted with MPs at 90° and IPs at 0°, as described earlier.
Vascular injuries have the potential to be limb or digit threatening. A partial laceration of an artery at the wrist level can potentially cause exsanguinating hemorrhage. Consultations for these injuries must be evaluated urgently.
Initial treatment for an actively bleeding wound should be direct local pressure for no less than 10 continuous minutes. If this is unsuccessful, an upper extremity tourniquet inflated to 100 mmHg above the systolic pressure should be used. One should keep this tourniquet time to less than 2 hours to avoid tissue necrosis. Once bleeding is controlled well enough to evaluate the wound, it may be cautiously explored to evaluate for bleeding points. One must be very cautious if attempting to ligate these to ensure that adjacent structures such as nerves are not included in the ligature.
The hand must be evaluated for adequacy of perfusion to the hand as a whole as well as the individual digits. Capillary refill, turgor, Doppler signal, and bleeding to pinprick all provide useful information regarding vascular status. The finger or hand with vascular compromise requires urgent operative exploration. Unlike the complete amputation, in which the amputated part can be cold preserved (see below), devascularization without amputation produces warm ischemia, which is tolerated only for a matter of hours.
For the noncritical vascular injury, two treatment options exist. Simple ligation will control hemorrhage. At least one of the palmar arterial arches is intact in 97% of patients,5 so this will usually not compromise hand perfusion. Each digit also has two arterial inflows and can survive on one (see Amputations and Replantation section below). In the academic hospital setting, however, consideration should be given to repairing all vascular injuries. Instructing a resident in vascular repair in the noncritical setting will produce a more skilled and prepared resident for when a critical vascular injury does arise.
SPECIAL CONSIDERATIONS
After replantation was first reported,16 replantation was attempted for nearly all amputations. Over the ensuing decades, more stringent guidelines have been established regarding what should be replanted. Indications for replantation include amputations of the thumb, multiple digit amputations, and amputations in children. Relative contraindications to replantation include crush injuries, injuries to a single digit distal to the PIP joint, and patients who are unable to tolerate a long surgical procedure. As with all guidelines, one should evaluate the particular needs of the injured patient.
In preparation for replantation, the amputated part and proximal stump should be appropriately treated. The amputated part should be wrapped in moistened gauze and placed in a sealed plastic bag. This bag should then be placed in an ice water bath. Do not use dry ice, and do not allow the part to contact ice directly; frostbite can occur in the amputated part, which will decrease its chance of survival after replantation. Bleeding should be controlled in the proximal stump by as minimal a means necessary, and the stump should be dressed with a nonadherent gauze and bulky dressing.
For digital amputations deemed unsalvageable, revision amputation can be performed in the ER if appropriate equipment is available. Bony prominences should be smoothed off with a rongeur and/or rasp. Great care must be taken to identify the digital nerves and resect them back as far proximally in the wound as possible; this helps decrease the chance of painful neuroma in the skin closure. Skin may be closed with permanent or absorbable sutures; absorbable sutures will spare the patient the discomfort of suture removal several weeks later. For more proximal unsalvageable amputations, revision should be performed in the operating room to maximize vascular and neural control.
Prostheses can be made for amputated parts. The more proximal the amputation, the more important to function the prosthesis is likely to be. Although finger-level prostheses are generally considered cosmetic, patients with multiple finger amputations proximal to the DIP have demonstrable functional benefit from their prosthesis as well.17
Fingertip injuries are among the most common pathologies seen in an ER. The usual history is that a door closed on the finger (commonly the middle, due to its increased length) or something heavy fell on the finger.
Initial evaluation should include: wound(s) including the nail bed, perfusion, sensation, and presence and severity of fractures. For the common scenario, complex lacerations with minimally displaced fracture(s) and no loss of perfusion, the wound is cleansed, sutured, and splinted in the ER. To properly assess the nail bed, the nail plate (hard part of the nail) should be removed. A Freer periosteal elevator is well suited for this purpose. Lacerations are repaired with 6-0 fast gut suture. Great care must be taken when suturing because excessive traction with the needle can further lacerate the tissue. After repair, the nail folds are splinted with the patient’s own nail plate (if available) or with aluminum foil from the suture pack. This is done to prevent scarring from the nail folds down to the nail bed that would further compromise healing of the nail.
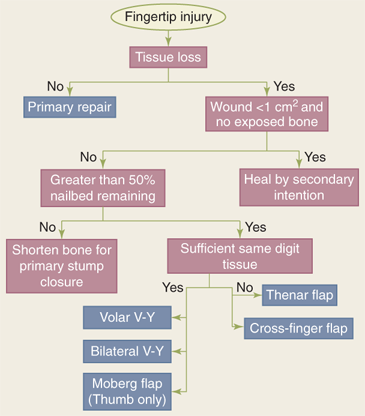
In some situations, tissue may have been avulsed in the injury and be unavailable for repair. Choice of treatment options depends on the amount and location of tissue loss (Fig. 44-15). For wounds less than 1 cm2 with no exposed bone, secondary intention will produce excellent functional and aesthetic results. For larger wounds or wounds or with bone exposed, one must decide if the finger is worth preserving at the current length or if shortening to allow for primary closure is a better solution. A useful guideline is the amount of fingernail still present; if greater than 50% is present, local or regional flap coverage may be a good solution.
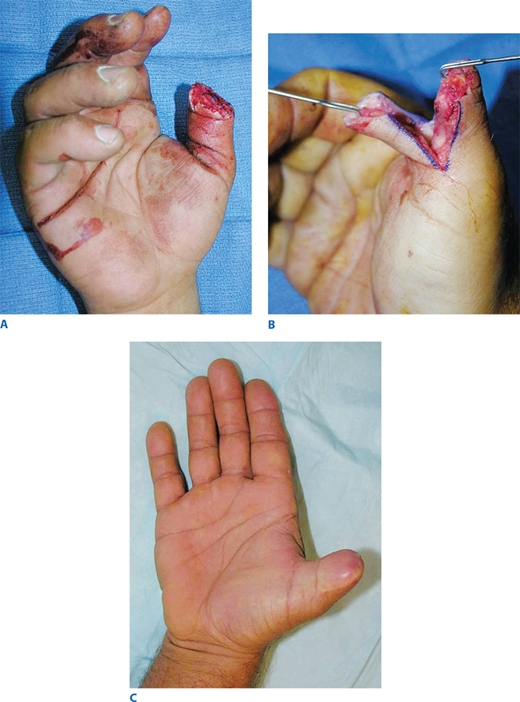
If sufficient local tissue is present, homodigital flaps can be considered. A wide range of antegrade and retrograde homodigital flaps can be mobilized to cover the defect. Some carry sensation or can receive nerve coaptation to recover sensation over time.18 For the thumb only, the entire volar skin including both neurovascular bundles can be raised and advanced distally up to 1.5 cm.19 The thumb receives separate vascularity to its dorsal skin from the radial artery. This flap is not appropriate for the fingers. Patients retain full sensibility in the advanced skin and can be mobilized within days of surgery (Fig. 44-16A–C).
Figure 44-16.
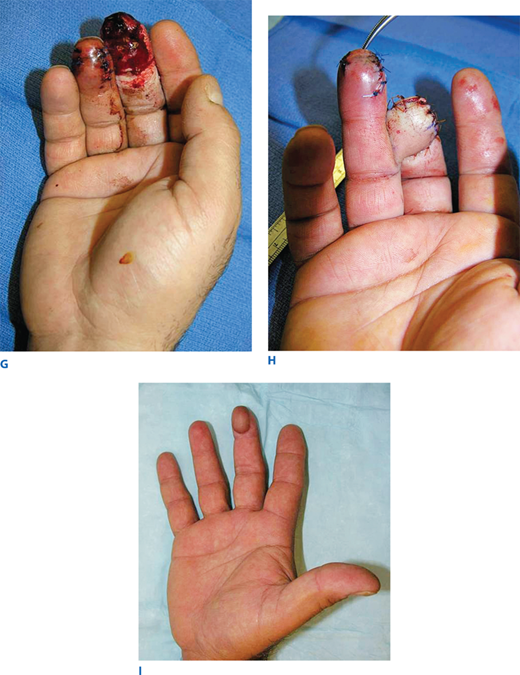
Local flaps for digital tip coverage. A–C. For thumb injuries, Moberg described elevation of the entire volar skin with both neurovascular bundles for distal advancement. Sensation to the advanced skin is maintained. D–F. An 8-year-old girl underwent fingertip replantation that did not survive. A thenar flap was transferred to cover the defect. Some authors advise against its use in patients over 30 years old. G–I. In this 45-year-old man, the entire skin of P3 of the long finger was avulsed and unrecoverable. A cross-finger flap was transferred and provides excellent, durable coverage. The border of the flap and surrounding skin is still apparent 4.5 months after surgery.
For wounds too large to cover with homodigital tissue, regional flaps can be considered. The skin from the distal radial thenar eminence can be raised as a random pattern flap (Fig. 44-16D–F). The finger is maintained in flexion for 14 to 21 days until division of the flap pedicle and inset of the flap. Some authors have reported prolonged stiffness in patients over 30 years old, but careful flap design helps minimize this complication.20 Alternatively, the skin from the dorsum of the middle phalanx of an adjacent digit can be raised as a flap to cover the volar P3 (Fig. 44-16G–I). The flap is inset at 14 to 21 days. Long-term studies have shown this flap develops sensation over time.21
Patients with fingertip injures must be assessed for the possibility of salvage of the injured digit(s) taken within the context of the patient’s recovery needs and goals. The surgeon then matches the available options to the particular patient needs.
High-pressure devices are commonly used for cleaning and applications of liquids such as lubricants and paint. Most commonly, the inexperienced worker accidentally discharges the device into his nondominant hand at the base of the digit. Severity of injury depends on the amount and type of liquid injected; hydrophobic compounds cause greater damage.
These injuries are typically quite innocuous to inspection. They are, however, digit-threatening emergencies. The patient should be informed of the severity of the injury, and exploration is ideally performed within 6 hours of injury. Up to 50% of such injuries result in loss of the digit, but early recognition and treatment are associated with increased chance of digit survival.22 Early frank discussion with the patient and initiation of appropriate treatment produce the best results and medicolegal protection.
Compartment syndromes can occur in the forearm and/or the hand. As in other locations, these are potentially limb-threatening issues. Principle symptoms are pain in the affected compartments, tense swelling, tenderness to palpation over the compartment, and pain with passive stretch of the muscles of the compartment.23 Pulse changes are a late finding; normal pulses do not rule out compartment syndrome.
There are three compartments in the forearm and four groups of compartments in the hand. The volar forearm is one compartment. On the dorsum of the forearm, there is the dorsal compartment as well as the mobile wad compartment, beginning proximally over the lateral epicondyle. In the hand, the thenar and hypothenar eminences each represent a compartment. The seven interosseous muscles each behave as a separate compartment.
Compartment syndrome can be caused by intrinsic and extrinsic causes. Intrinsic causes include edema and hematoma due to fracture. Extrinsic causes include splints and dressings that are circumferentially too tight and intravenous infiltrations. Infiltrations with hyperosmolar fluids such as x-ray contrast are particularly dangerous, because additional water will be drawn in to neutralize the hyperosmolarity.
Measurement of compartment pressures can be a useful adjunct to assessment of the patient. The Stryker pressure measurement device or similar device is kept in many operating rooms for this purpose. The needle is inserted into the compartment in question, a gentle flush with 0.1 to 0.2 cc of saline clears the measurement chamber, and a reading is obtained. Studies have disagreed about whether the criterion is a measured pressure (30–45 mmHg, depending on the series) or within a certain amount of the diastolic blood pressure.24
Compartment releases are performed in the operating room under tourniquet control. Release of the volar forearm compartment includes release of the carpal tunnel. As the incision travels distally, it should pass ulnar and then curve back radially just before the carpal tunnel. This avoids a linear incision across a flexion crease and also decreases the chance of injury to the palmar cutaneous branch of the median nerve. One dorsal forearm incision can release the dorsal compartment and the mobile wad. In the hand, the thenar and hypothenar compartments are released each with a single incision. The interosseous compartments are released with incisions over the index and ring metacarpal shafts. Dissection then continues radial and ulnar to each of these bones and provides release of all the muscle compartments. Any dead muscle is débrided. Incisions are left open and covered with a nonadherent dressing. The wounds are reexplored in 2 to 3 days to assess for muscle viability. Often the incisions can be closed primarily, but a skin graft may be needed for the forearm.
If the examiner feels the patient does not have a compartment syndrome, elevation and serial examination are mandatory. When in doubt, it is safer to release an early compartment syndrome than wait to release and risk muscle necrosis. Progression of compartment syndrome can lead to Volkmann’s ischemic contracture with muscle loss and scarring that may compress nerves and other critical structures. Medicolegally, it is far easier to defend releasing an early compartment syndrome than delaying treatment until the process has progressed to necrosis and/or deeper scarring.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree