Surgery for Subareolar Abscess; Duct Excision
James P. De Andrade
Jesse L. Dirksen
An acute subareolar abscess can initially be treated with antibiotics and needle aspiration or incision and drainage as appropriate. However, these abscesses generally are associated with underlying duct pathology that predisposes to recurrence of abscess or formation of a mammary duct fistula. Thus, it is often necessary to excise the diseased subareolar ducts to prevent recurrence. Duct excision is also used to diagnose and treat nipple discharge. This chapter describes the management of subareolar abscesses as well as definitive surgical ductal excision for nipple discharge or chronic subareolar abscess.
SCORE™, the Surgical Council on Resident Education, classified incision, drainage, debridement for soft tissue infections, and duct excision as “ESSENTIAL COMMON” procedures.
STEPS IN PROCEDURE
Surgery for Subareolar Abscess
Inspect, palpate, and perform ultrasound imaging (if needed) of the abscess and overlying skin
Aspirate if small and liquid
Incise if complex
Small, radially oriented incision at areolar border
Send fluid for culture
Duct Excision (Microdochectomy and Central Duct Excision)
Place lacrimal duct in offending duct
Incision
Circumareolar for nipple discharge
Radial ellipse for chronic subareolar abscess/mammary fistula
Elevate flaps
Ligate duct(s) at undersurface of the nipple and do a wedge resection proximally
Orient the specimen
Obtain hemostasis
Close incision in two layers
HALLMARK ANATOMIC COMPLICATIONS
Subareolar Abscess
Recurrence or fistula formation
Incomplete evacuation of necrotic or purulent material
Undiagnosed inflammatory breast carcinoma
Duct Excision (Microdochectomy and Central Duct Excision)
Inverted nipple
Insensate nipple
Nipple necrosis
LIST OF STRUCTURES
Nipple
Areola
Subareolar ducts
Intercostal nerves 4 to 6
Lateral cutaneous branch
Anterior cutaneous branch
Subareolar Abscess
Technical and Anatomic Points
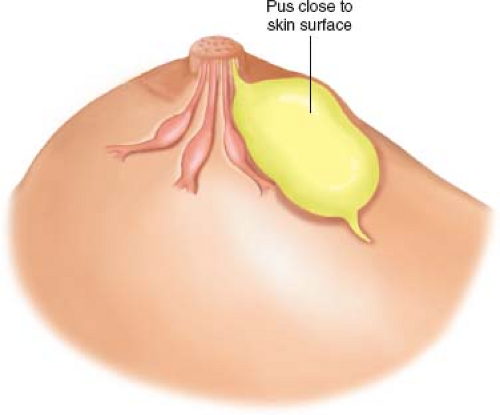
Examine the patient in the supine position with the ipsilateral arm extended above the patient’s head. Suspect a subareolar abscess by location and setting (generally seen in nonlactating women). First, visually inspect the breast for the degree of erythema and the integrity of the skin overlying the abscess (Fig. 17.1). Second, palpate the area to determine the amount of induration and fluctuance. Finally, use an ultrasound machine to visualize if an abscess cavity is present and to determine if other adjacent loculated collections exist (please refer to breast ultrasound techniques described in Chapter 15). If the skin is not overly thinned or necrotic and an abscess cavity containing liquid contents and without loculations is visualized with ultrasound, the subareolar abscess is amenable to needle aspiration, either under direct palpation or with ultrasound guidance.
Aspiration is performed in a manner similar to cyst aspiration (see Chapter 15). Prep and drape the area in a sterile fashion. Most often, aspiration can be performed under palpation. If ultrasound is needed, drape the ultrasound transducer with a sterile cover. Anesthetize the area with local anesthetic using a 22- or 25-gauge needle. Using an 18-gauge needle, aspirate the abscess cavity under ultrasound guidance and then culture the fluid to tailor antibiotic therapy. The abscess cavity will collapse on ultrasound imaging if an adequate aspiration has been achieved. Ultrasound-guided aspiration may need to be repeated every 2 to 3 days as the abscess cavity slowly collapses and heals in conjunction with antibiotics.
If the skin is significantly thinned or necrotic, the abscess should be managed with incision and drainage. Prep and drape the area and anesthetize with local anesthetic. A number 15 blade is used to make a stab incision into the abscess cavity and the purulent fluid is evacuated and cultured (Fig. 17.2A). The incision should be made along the areolar border, if possible, as this lends to a better cosmetic result. A small radially oriented incision facilitates subsequent ductal excision should this be required. Avoid using a long circumareolar incision as this may complicate subsequent excision. Use local anesthetic or sterile saline to irrigate the abscess cavity. Debride grossly nonviable tissue and send cultures. A small drain may be placed. Packing is not routinely utilized in the management of a subareolar abscess.
These abscesses are generally caused by ductal ectasia or other problem in the distal ducts such as stricture from nipple piercing (Fig. 17.2B). This underlying problem is not cured by aspiration or incision and drainage. Always warn the patient that recurrence is common. Recurrence may take the form of another abscess, or a chronic draining fistula at the areolar margin. This chronic draining fistula is termed a mammary duct fistula or mammary fistula. Definitive management requires duct excision.
Duct Excision (Microdochectomy and Central Duct Excision) for Nipple Discharge
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree