Superficial Myxoid Lesions
INTRODUCTION
As a general rule, superficial myxoid lesions are benign and deep ones are often malignant, with the important exceptions that intramuscular myxoma is deep and myxofibrosarcoma (also called myxoid malignant fibrous histiocytoma) is classically superficial. These latter two lesions are covered in Chapter 21 and are likely to be sampled on needle biopsies, whereas superficial lesions are typically managed by excisional biopsy. The classic myxoid lesions of the genital region (aggressive angiomyxoma and angiomyofibroblastoma) are considered in Chapter 8.
CUTANEOUS MYXOMA AND SUPERFICIAL ANGIOMYXOMA (CUTANEOUS ANGIOMYXOMA)
Myxomas of the dermis and subcutaneous tissue are less well-characterized than the more frequently encountered deep intramuscular myxomas and those arising in the jaw bones and heart. In 1985, Carney et al.1 described a complex of myxomas, including cutaneous myxomas, spotty pigmentation, and endocrine overactivity—such patients have been subsequently shown to have various mutations in the PRKAR1A gene.2,3,4,5,6,7 In 1988, Allen et al.8 delineated the clinicopathologic features of histologically similar appearing myxoid lesions of the dermis and subcutaneous tissue which lacked an association with Carney complex. After a critical review of the literature, Allen et al.8 concluded that the lesions he described, many previously reported and variously named myxoid lesions of the dermis and subcutis, as well as the “cutaneous myxomas” of Carney complex, were all closely related. The term “superficial angiomyxoma” was proposed to encompass both syndromic and sporadic superficial myxomas. Superficial angiomyxomas were unassociated with Carney complex in a subsequent series,9 so the syndromic ones are presumably rare.
Clinical Features
Allen et al.8 described three clinical presentations of superficial myxomas. The most common presentation is that of a solitary lesion unassociated with Carney complex, followed by multiple lesions unassociated with
Carney complex, and lastly, lesions associated with the fully expressed Carney complex.
Carney complex, and lastly, lesions associated with the fully expressed Carney complex.
Superficial angiomyxoma/cutaneous myxoma unassociated with Carney complex presents as a painless, slow-growing, solitary skin nodule with a slight male predominance. Lesions arise primarily on the trunk and lower extremity, followed by the head and neck region and arm. They have also been reported in the female and male genital regions.10
Carney complex1 includes pigmented skin lesions (lentigines and giant cell blue nevi), endocrine disorders (primary pigmented nodular adrenocortical disease, a variety of stromal tumors of the testis, and growth hormone-producing pituitary adenoma), psammomatous melanocytic schwannoma, and myxomatous tumors (cardiac myxoma, myxoid fibroadenoma of the breast, myxoma of the external ear canal11 and cutaneous myxoma). The disorder is familial and transmitted as an autosomal dominant trait. Females are affected slightly more often than males, and the initial lesions manifest at an early age (mean 18 years). Most patients do not have all of the lesions. However, as the cardiac myxoma and the psammomatous melanocytic schwannoma are the main causes of morbidity and mortality in this disorder,1,12 it is important to identify patients at risk so that proper evaluation for these potentially lethal tumors can be performed.
Superficial myxomas associated with Carney complex are usually multiple and vary from small sessile papules to large pedunculated lesions. They most commonly occur on the eyelid.1
Cutaneous myxomas are benign but local recurrence is common, especially with superficial angiomyxomas containing epithelial components.8
Pathologic Features
On gross examination, the tumor consists of soft, lobulated nodules, which may appear as polypoid or pedunculated skin lesions. The majority of lesions range between 1 and 5 cm. The cut surface is glistening, mucoid or gelatinous, and gray to white. Incomplete collagenous bands traverse the cut surface, resulting in a nodular configuration.
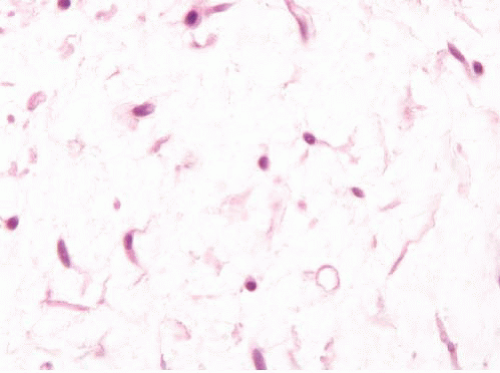
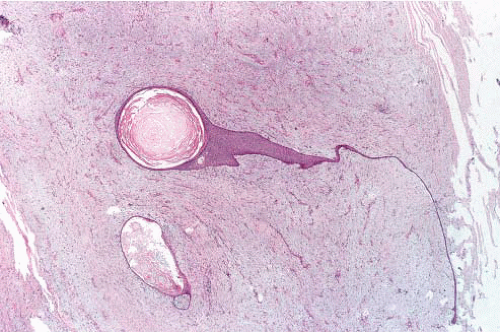
Microscopically, the process typically involves both the dermis and subcutaneous fat, but, occasionally, only one location is affected (Fig. 20.1). The tumor consists of multiple, variably demarcated angiomyxoid nodules (Fig. 20.2, e-Fig. 20.1). The nodules are composed of a hypo- to moderately cellular population of bland-appearing, short spindled, stellateshaped (Fig. 20.3, e-Fig. 20.2), and, occasionally, multinucleated cells scattered haphazardly throughout a highly myxoid stroma. Mitotic activity is negligible.
The stroma contains abundant hyaluronic acid-rich matrix that forms microcysts within the nodules and cleft-like spaces at the interface of the nodule with the surrounding tissue. Thin, wavy collagen fibers
course through the stroma. The vascular element consists of small- to medium-sized, thin-walled, nonarborizing vessels. The vascular density of the nodules varies. Other features observed in superficial angiomyxoma include some perivascular hyalinization, a mixed inflammatory infiltrate (including neutrophils [Fig. 20.4, e-Fig. 20.3] and mast cells), fibrin and hemosiderin deposition, and interstitial hemorrhage.
course through the stroma. The vascular element consists of small- to medium-sized, thin-walled, nonarborizing vessels. The vascular density of the nodules varies. Other features observed in superficial angiomyxoma include some perivascular hyalinization, a mixed inflammatory infiltrate (including neutrophils [Fig. 20.4, e-Fig. 20.3] and mast cells), fibrin and hemosiderin deposition, and interstitial hemorrhage.
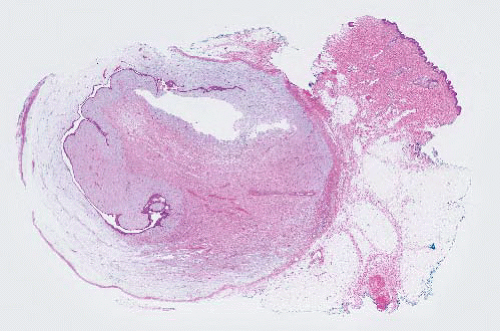 FIGURE 20.1 Cutaneous myxoma/superficial angiomyxoma. This lesion is multilobulated and superficial. On the left part of the field, the tumor has entrapped skin adnexal structures. |
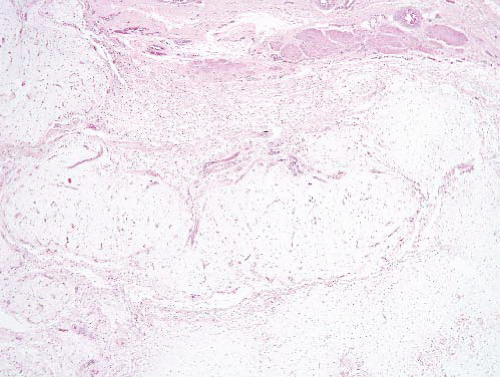 FIGURE 20.2 Cutaneous myxoma/superficial angiomyxoma. The tumor lobules have numerous small delicate capillaries. |
Epithelial structures within the tumor nodules (Fig. 20.5), including epidermal cysts with keratinous debris and linear strands of squamous cells emanating from the epidermal surface or from a cyst wall, have been identified in about a third of cases and have contributed to the plethora of names given to superficial angiomyxoma in the past.
The differential diagnosis is summarized in Table 20.1.
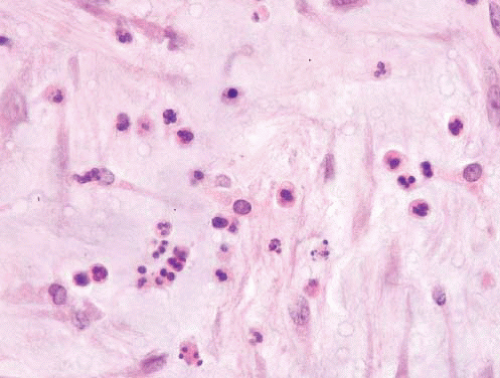 FIGURE 20.4 Cutaneous myxomas/superficial angiomyxomas often have abundant intralesional neutrophils. |
TABLE 20.1 Differential Diagnosis of Cutaneous Myxoma/Angiomyxoma | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|