Superficial Groin Dissection
Laura A. Adam
Neal W. Wilkinson
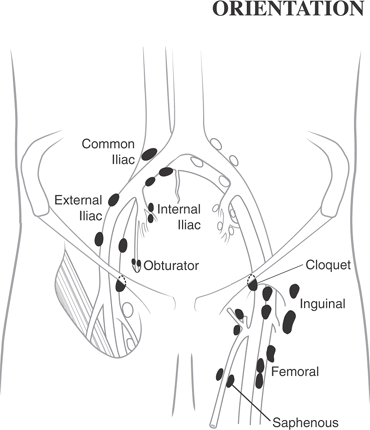
A variety of terms are used to describe lymphadenectomy of the inguinal and ilio-inguinal region. In this chapter, we will use the terms superficial and deep (orientation figure). A superficial dissection includes the lymph node basins of the inguinal ligament, saphenous vein, and femoral vessels. Cloquet’s node is typically removed during a superficial dissection. A deep dissection includes the lymph node basins extending along the course of external, internal, and common iliac vessels (orientation figure). In addition, deep dissection may include lymph nodes within the obturator canal.
Superficial Region
Inguinal
Saphenous
Femoral
Cloquet’s node
Deep Region
External iliac
Internal iliac
Common iliac
Obturator
When both the superficial and deep regions are removed, we will refer to a superficial and deep dissection, realizing that the term radical is occasionally used in this setting. The proximal extent or pelvic component of the dissection may vary depending on the pathology being treated and must be clearly stated in the operative note instead of using vague terms such as deep or radical.
Steps in Procedure
Superficial Inguinal Dissection
Supine position with leg externally rotated and knee slightly flexed
Lazy S–shaped incision from anterosuperior iliac spine to medial thigh
Proximal extent used primarily for deep dissection or in obese patients
Develop flaps medially and laterally just above superficial fascia; to lateral border of sartorius muscle and medial border of gracilis muscle
Avoid lateral femoral cutaneous nerve
Ligate tributaries of saphenous vein entering field and saphenous vein itself entering inferior aspect of field
Sweep fatty node-bearing tissue cephalad to saphenofemoral junction and ligate and divide saphenous vein (oversew femoral end)
Divide or retract inguinal ligament to expose femoral canal
Remove nodal tissue; label the highest node as Cloquet’s node and submit separately
Deep Inguinal Ligament
Place deep self-retaining retractors and divide external oblique aponeurosis
Divide inguinal ligament
Displace spermatic cord (in males) medially and divide the inferior epigastric vessels
Gently displace peritoneum medially to expose retroperitoneal structures
Begin laterally on the pelvic sidewall and sweep nodes and associated tissues medial
Mobilize rectum and bladder medially and retract these behind moist packs
Obturator node dissection can be performed by following the obturator nerve and artery
Obtain hemostasis and reapproximate the inguinal ligament and abdominal wall structures
Detach sartorius high on the anterior superior iliac spine
Mobilize it, rotating it to fit into the space over the femoral vessels
Suture the sartorius muscle to the inguinal ligament
Place closed suction drains and close, resecting several millimeters from skin edges
Close incision in layers
Hallmark Anatomic Complications
Injury to lateral femoral cutaneous nerve
Injury to femoral vein or femoral nerve
Injury to obturator nerve
Injury to pelvic nerve plexus
Lymphocele or lymphedema
Skin necrosis
List of Structures
Inguinal Lymph Nodes
Superficial inguinal lymph nodes
Deep inguinal lymph nodes
Node of Cloquet
Iliac lymph nodes
Obturator Lymph Nodes
Obturator foramen
Obturator canal
Anterosuperior iliac spine
Lateral femoral cutaneous nerve
Inguinal ligament
Pubic tubercle
External oblique aponeurosis
Fascia lata
Femoral Triangle
Femoral nerve
Femoral artery
Femoral vein
Saphenous Vein
Saphenofemoral junction
Adductor longus muscle
Sartorius muscle
The superficial and deep inguinal lymph node dissection is most commonly performed for cutaneous malignancies of the lower extremity, lower abdomen, and flank. Melanoma remains the most common indication and the majority will have been localized to the region by sentinel node mapping techniques. Additional indications include penile, distal urethral, scrotal, vulvar, anal, and anal canal cancers. The pelvic lymphadenectomy for gynecologic pathology may include many of the same regional lymph node basins, but is approached through a lower midline incision and will not be covered in this chapter.
These procedures carry a significant risk of local morbidity, including skin flap necrosis, wound infection, seroma formation, and lymphedema. For melanoma, the procedure should be only performed for documented disease in the region commonly described as a “therapeutic” lymphadenectomy. Sentinel lymph node staging, computed tomography or ultrasound directed fine-needle aspiration, and now positron emission tomography can be used to preoperatively stage the region and has replaced elective nodal dissection for melanoma.
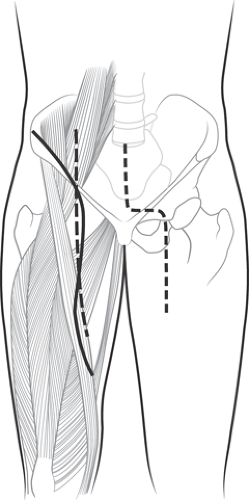
Incision and Elevation of Flaps: Superficial and Deep Regions (Fig. 96.1)
Technical Points
 |
After induction of anesthesia, the patient is positioned supine with the leg externally rotated and the knee slightly flexed to improve medial exposure. In larger patients, placing a bump under the thigh may further facilitate exposure. Preoperative antibiotics are frequently given despite the procedure being a Class I (infection classification) case. Most wound complications
are related to skin flap necrosis and lymphedema. These are not likely to be influenced by antibiotics, and randomized controlled trials have questioned their efficacy in preventing wound complications. However, because of these high wound complication rates, it is reasonable to provide a short course of antibiotics directed toward common skin flora. A Foley catheter and sequential compression devices are typically used. Muscle paralysis should be minimized until the femoral nerve is clearly identified. The skin preparation and draping should include lower abdomen to knee with wide medial and lateral exposure.
are related to skin flap necrosis and lymphedema. These are not likely to be influenced by antibiotics, and randomized controlled trials have questioned their efficacy in preventing wound complications. However, because of these high wound complication rates, it is reasonable to provide a short course of antibiotics directed toward common skin flora. A Foley catheter and sequential compression devices are typically used. Muscle paralysis should be minimized until the femoral nerve is clearly identified. The skin preparation and draping should include lower abdomen to knee with wide medial and lateral exposure.
The inferior aspect of the incision is placed directly over the femoral vessels and should extend inferiorly to the convergence of the sartorius and femoral vessels. The superior aspect of the incision may vary based on surgeon choice, patient body habitus, and anticipated proximal extent of the dissection. We prefer a lazy S–shaped incision from the anterosuperior iliac spine to the medial thigh with the middle portion overlying the bottom of the inguinal ligament. The abdominal pannus in large body habitus patients can be rotated medially and elevated superiorly to provide better visualization. An alternate straight vertical incision traversing the inguinal ligament onto the lower abdomen works well in thin patients. If a previous sentinel lymph node biopsy site exists, it should be included in the incision. The proximal extent of the incision can vary depending on proximal extent of the dissection and will need to be longer if a deep dissection is to be done. The abdomino-inguinal incision is seldom indicated to gain wider access to the pelvis but can provide wide exposure of the entire internal pelvis when clinically indicated: proximal control of vessels, difficult bleeding, or bulky adenopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree