Subtotal Parathyroidectomy or Total with Autologous Graft
Brian D. Saunders
DEFINITION
Parathyroidectomy is a functional surgical procedure performed to remove all or nearly all of a patient’s hyperactive parathyroid tissue. Primary hyperparathyroidism is the most common pathologic entity requiring parathyroidectomy. Although roughly 85% to 90% of primary hyperparathyroidism involves a single overactive parathyroid gland, there are somatic, as well as inherited, conditions that result in multiglandular parathyroid pathology.1 Further, secondary and occasionally tertiary hyperparathyroidism may require surgical resection of more than one parathyroid gland. Subtotal parathyroidectomy is the removal of all but a small portion of one parathyroid gland from the neck. This usually equates to removing three and a half parathyroid glands. The remnant portion of parathyroid tissue is left on its native blood supply and in its normal anatomic position. An alternative to a subtotal resection of parathyroid tissue is a total or complete removal of parathyroid tissue (e.g., all four glands) and the immediate transplantation of autologous parathyroid tissue into a heterotopic position.
DIFFERENTIAL DIAGNOSIS
The necessity for a multiglandular resection of parathyroid tissue may be recognized preoperatively or intraoperatively. There are a number of etiologies for hyperparathyroidism that are always multiglandular in nature and, as such, would warrant preoperative planning for either a subtotal parathyroidectomy or a total parathyroidectomy with parathyroid autotransplantation. These include multiple endocrine neoplasia (MEN) type I- and type IIa-related primary hyperparathyroidism and secondary hyperparathyroidism related to renal failure. Other pathophysiologic conditions leading to hyperparathyroidism may involve the overactivity of more than one gland. Intraoperative recognition of multiple enlarged glands, or recognition through intraoperative parathormone monitoring data, may lead the surgeon to subtotally resect the parathyroids or perform a total parathyroidectomy with immediate transplant. These include sporadic primary hyperparathyroidism due to multiglandular hyperplasia, lithium-related primary hyperparathyroidism, tertiary hyperparathyroidism, and CDC73-related causes of hyperparathyroidism.2 This latter category is a familial hyperparathyroidism caused by germline mutations in the CDC73 gene (also known as HRPT2 or parafibromin) and includes familial, isolated hyperparathyroidism and hyperparathyroidism-jaw tumor syndrome.3
PATIENT HISTORY AND PHYSICAL FINDINGS
Hyperparathyroidism is a biochemical diagnosis. The evaluation of a patient for hyperparathyroidism may begin with an incidental note of an elevated calcium level on a laboratory report or with interrogating a patient’s calcium level based on the patient’s presenting signs or symptoms. Patients with recurrent nephrolithiasis (especially calciumbased kidney stones) or osteoporotic (e.g., fragility or nontraumatic) bone fractures should be evaluated for hypercalcemia and hyperparathyroidism. Other, less specific, symptoms that may warrant a biochemical investigation for hyperparathyroidism include fatigue; musculoskeletal aches and pains; neurocognitive decline; mood lability; abdominal pain; and recurrent, otherwise unexplained, pancreatitis.
A detailed family history should be sought to evaluate the possibility of an inherited cause of hyperparathyroidism. The patient should be queried about family members with pituitary tumors, other cases of parathyroid disease, medullary thyroid cancer, pheochromocytomas, enteropancreatic neuroendocrine tumors (especially gastrin-producing tumors), and ossifying fibromas of the mandible.
Patients with suspected inherited causes of hyperparathyroidism should be counseled to seek genetic counseling and testing as this may impact operative planning, future disease surveillance, and the health of relatives.
Renal-related secondary hyperparathyroidism is a constant and expected biochemical finding in all patients with chronic kidney dysfunction. The degree of hyperparathormonemia is routinely followed by treating nephrologists, especially in patients who have progressed to some form of renal replacement therapy (peritoneal or hemodialysis). National management guidelines exist for the target parathyroid hormone (PTH) level for each stage of chronic kidney disease.4
Physical examination findings for patients with hyperparathyroidism are uncommon. Certainly, the neck of each patient proposed for a parathyroidectomy should be thoroughly examined. The identification of a palpable mass would warrant further imaging investigation. It is distinctly unusual to palpate a parathyroid adenoma. A palpable mass with severe hyperparathyroidism should raise the specter of the unusual entity of parathyroid carcinoma. Often, though, a palpable central neck mass in a patient with hyperparathyroidism is an incidentally discovered thyroid nodule.
For patients planned to undergo a total parathyroidectomy with immediate autologous parathyroid transplantation, a detailed inspection of the forearms should be undertaken. It is important to note the handedness of the patient, as the parathyroid autograft is usually placed in the nondominant forearm. In patients with preexisting or impending renal failure, note should be made of arteriovenous fistula position. Great care should be taken to avoid injuring a functional fistula or disturbing the bed of a soon-to-be constructed fistula.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Hyperparathyroidism (whether primary, secondary, or tertiary) is a biochemical diagnosis. This must be made to the satisfaction of the surgeon prior to contemplating any procedure. The surgeon should consider imaging studies only after a diagnosis has been secured and the need for an operation has been established.
Known multiglandular parathyroid disease processes that will require preoperative planning for a subtotal parathyroidectomy or a total parathyroidectomy with autologous graft do not require parathyroid imaging as both sides of the neck will need to be explored and all four of the parathyroid glands identified.
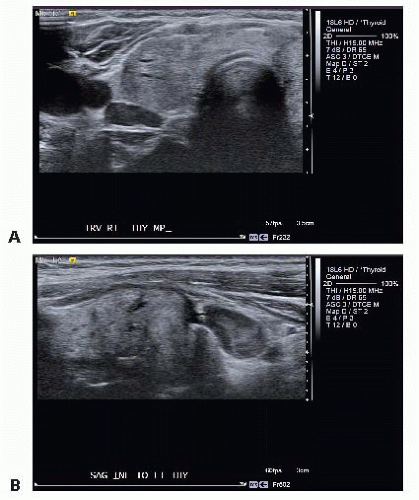
High-resolution ultrasonography of the neck (whether performed by the surgeon or a radiologist) is an excellent modality to attempt to localize enlarged parathyroid glands. Parathyroid adenomas appear as hypoechoic, ovoid masses that are separable from the thyroid gland. Upper parathyroid adenomas that lie in the tracheoesophageal groove will often be mobile with graded compression of the ultrasound probe (FIG 1A,B). Parathyroid adenomas adjacent to the thyroid can usually be well seen, although ectopic parathyroid adenomas (e.g., posterior to the clavicular heads) may be difficult to visualize due to limitations of the ultrasound waves in travelling through bone. Ultrasonography will also aid in the identification of concurrent thyroid pathology, which may then be dealt with at the time of the parathyroid operation.
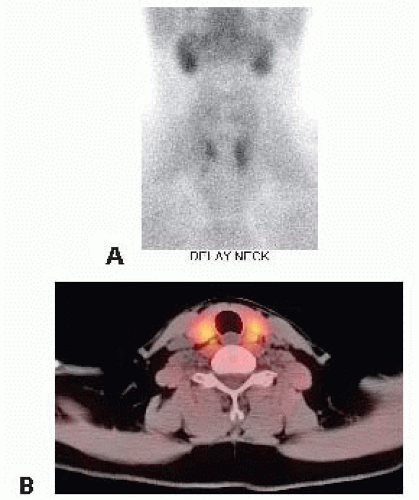
Nuclear medicine parathyroid scans using technetium sestamibi as a tracer can accurately identify overactive parathyroid glands about 85% of the time.5 When performed with a concurrent single-photon emission computed tomography (SPECT)/computed tomography (CT) scan, this overlay of functional and structural imaging provides an excellent anatomic map of disease localization invaluable to the operating surgeon (FIG 2A,B). One caveat is that small parathyroid adenomas in close association with the thyroid gland may be difficult to visualize with this imaging technique.
Neck CT scan or magnetic resonance imaging (MRI) is occasionally used to image parathyroid glands. Newer CT scan imaging protocols are becoming more widespread, such as 4D CT scans. This takes advantage of the timing of the intravenous (IV) contrast bolus, the vascularity of the parathyroid tumors, and the delayed washout of hyperactive parathyroid lesions.
More invasive modalities of parathyroid localization include selective venous sampling for PTH measurement. This technique requires experienced interventional radiologists and is best reserved for the reoperative setting.
Imaging prior to reoperative parathyroid surgery is essential to minimize exploration in a scarred operative field and to minimize iatrogenic morbidity. It is ideal to have two concordant imaging studies prior to all reoperative parathyroid surgery (see Part 5, Chapter 45).
SURGICAL MANAGEMENT
Preoperative Planning
Prior to any parathyroid operation, all diagnostic biochemical data should be reviewed to confirm to the surgeon’s satisfaction that a diagnosis of surgically correctable hyperparathyroidism is present in the patient.
If an autologous parathyroid transplant is planned, confirmation with the patient as to which upper extremity will be the recipient site should be sought.
The wound classification for parathyroid surgery is clean. It is rare for parenteral antibiotics to be indicated prior to parathyroid surgery. Individual patient characteristics (e.g., cardiac valvular lesions, implanted prosthetic hardware), however, should always be considered.
Local or general anesthesia may be used.
Positioning
The patient is positioned supine on the operating room (OR) table with the arms tucked either at the sides or lying on the abdomen. A sheet, fastened with towel clips, is used to secure the arms next to the patient and to allow for removal of the arm boards from the OR table (FIG 3).
If a parathyroid transplant is planned to the patient’s forearm, this arm can be extended from the patient and reprepped and draped at the time of that portion of the procedure (after the parathyroid tissue has been removed from the neck).
A towel roll or other small bump is placed behind the patient’s shoulder to aid in extension of the neck.
The bed is positioned with the head up, the feet down, and in some slight Trendelenburg. This is known as the semi-Fowler’s position or the beach chair position.
Some surgeons will rotate the OR table 90 degrees to have the head of the patient away from the anesthesia providers and thus more accessible to the surgical team.
 FIG 3 • The patient is positioned on the OR table with the arms tucked, a roll behind the shoulders, and the head elevated. |
TECHNIQUES
PLACEMENT OF INCISION
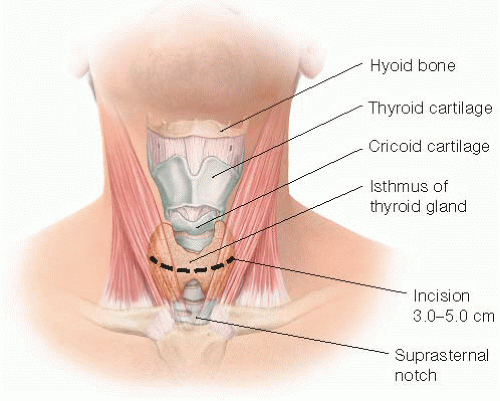
A transverse incision is made in the line of a skin crease roughly 1 cm caudal to the cricoid cartilage or two fingerbreadths cephalad to the suprasternal notch. The incision may be between 3 and 5 cm in length and is centered on the midline of the neck (FIG 4). Some surgeons will infiltrate the region of the incision with a local anesthetic combined with epinephrine. Placement of the incision within a natural skin line or crease of the neck is more important for postoperative cosmesis than the length of the incision (FIG 5).
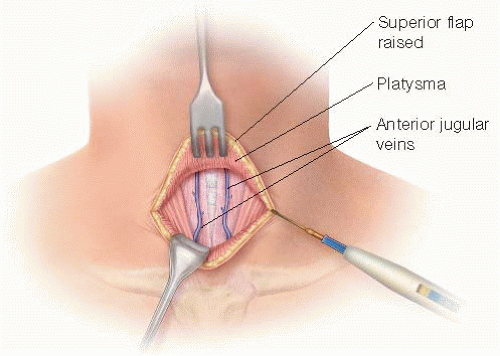
CREATION OF FLAPS
Dissection is deepened through the subcutaneous tissues and through the platysma muscle with electrocautery. Subplatysmal flaps are created superiorly, inferiorly, and laterally with a combination of electrocautery and blunt dissection (FIG 6).
Care must be taken to avoid injury to the paired anterior jugular veins. Should a rent be made in one of these veins, it is best to ligate the vein rather than attempt to cauterize the vein.
The superior flap should extend to the level of the thyroid cartilage and the inferior flap down to the sternal notch.
ENTRY INTO THE DEEP CENTRAL NECK SPACE
The avascular, midline raphe between the sternohyoid and sternothyroid muscles on each side is entered with electrocautery. This midline is best identified by digital palpation of the midline of the underlying trachea. These strap muscles should be separated to expose the underlying thyroid isthmus (FIG 7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree