Stasis Dermatitis
Cary Chisholm, MD
Key Facts
Clinical Issues
Age
Middle-aged and elderly individuals
Site
Distal extremities, abdomen
Appearance
Brown to black discoloration of affected areas
Erythematous, pruritic, scaly papules and plaques
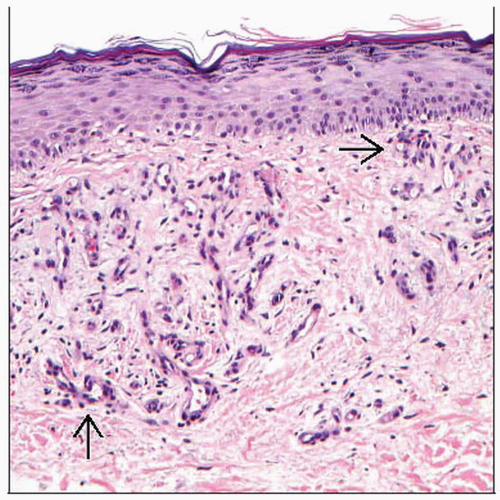
Microscopic Pathology
Acanthosis with mild spongiosis
Overlying hyperkeratosis with orthokeratosis or parakeratosis
Proliferation of superficial dermal blood vessels
Variable degree of fibrosis
Red blood cell extravasation
Variable amount of hemosiderin deposition
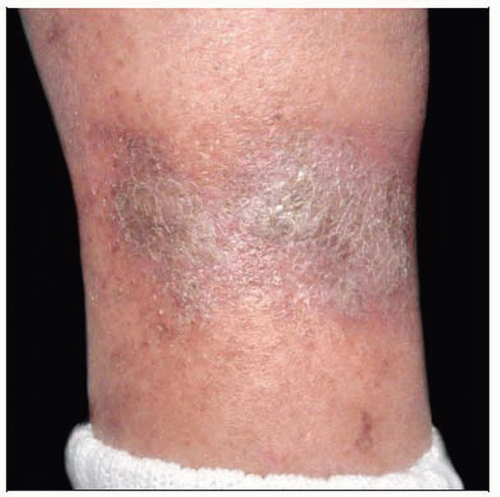 Brawny, gray-brown, adherent, dry scale over the medial ankle is the most common location for stasis dermatitis. Lower extremity is edematous with hyperpigmentation. |
TERMINOLOGY
Synonyms
Hypostatic dermatitis
Definitions
Hyperpigmentation primarily of the distal extremities in patients with chronic venous incompetence
ETIOLOGY/PATHOGENESIS
Pathogenesis
Develops secondary to longstanding venous insufficiency
Blood flow slows or becomes retrograde
Increased intravascular pressure caused congestion and dilation of capillaries
Vascular sludging impairs adequate tissue oxygenation
Chronic ischemia
Damage of the endothelium
Vascular leak and edema
Red blood cell extravasation
Hemoglobin is degraded, causing clinical hyperpigmentation
Microthrombi form, leading to focal necrosis and eventually ulceration
Chronic inflammation with deposition of fibrous tissue
Hardening of skin referred to as lipodermatosclerosis
Deranged cytokine cascades
Upregulation of transforming growth factor-β, basic fibroblast growth factor, platelet-derived growth factor
Increased matrix metalloproteinases lead to dermal matrix degradation
Lipodermatosclerosis contributes to ulcer formation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree