Squamous Cell Carcinoma
Bruce M. Wenig, MD
Key Facts
Terminology
Malignant epithelial neoplasm arising from surface epithelium with squamous cell differentiation
Etiology/Pathogenesis
Associated risk factors include
Nickel exposure, exposure to textile dust, tobacco smoking, prior Thorotrast use
May develop from sinonasal (schneiderian) papilloma; majority transform to keratinizing SCC
Clinical Issues
Represents approximately 3% of head and neck malignant neoplasms
Sites in decreasing order of frequency
Maxillary sinus antrum > nasal cavity > ethmoid sinus > sphenoid, frontal sinuses
Microscopic Pathology
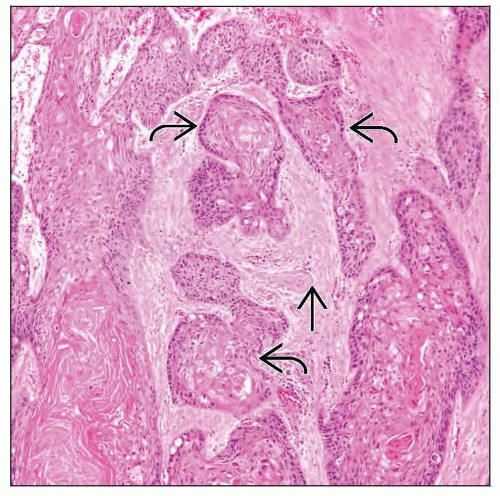
Divided into keratinizing and nonkeratinizing subtypes
Keratinizing squamous cell carcinoma
Most common type representing 80-85% of all cases
Divided into well-, moderately, poorly differentiated carcinomas
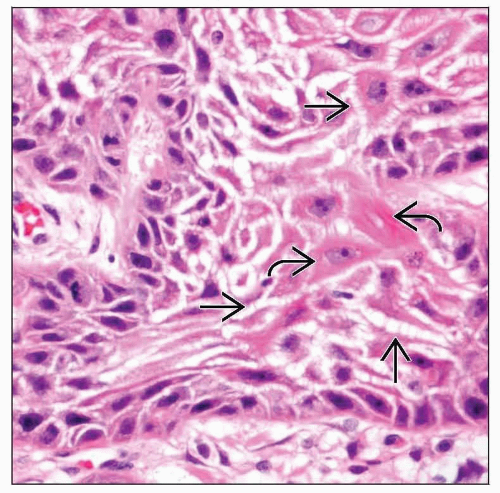
Nonkeratinizing squamous cell carcinoma
Represents approximately 15-20% of all cases
Often shows downward (inverted or endophytic) growth with broad interconnecting bands or nests of neoplastic epithelium
Composed of elongated cells with cylindrical or columnar appearance
TERMINOLOGY
Abbreviations
Squamous cell carcinoma (SCC)
Synonyms
For keratinizing squamous cell carcinoma
Sinonasal carcinoma
Epidermoid carcinoma
For nonkeratinizing squamous cell carcinoma
Transitional carcinoma
Respiratory epithelial carcinoma
Ringertz carcinoma
Cylindrical cell carcinoma
Definitions
Malignant epithelial neoplasm arising from surface epithelium with squamous cell differentiation
2 histologic subtypes
Keratinizing SCC
Nonkeratinizing SCC
Variants of SCC occur (discussed elsewhere) including
Verrucous carcinoma
Papillary SCC
Spindle cell squamous carcinoma
Basaloid SCC
Adenosquamous carcinoma
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Associated risk factors include
Nickel exposure
Exposure to textile dust
Tobacco smoking
Prior Thorotrast use
Developmental
May develop from sinonasal (schneiderian) papilloma
Majority transform to keratinizing SCC
Majority arise in association with inverted-type sinonasal papilloma
Human papillomavirus (HPV) may be found
Direct cause and effect not definitively found
CLINICAL ISSUES
Epidemiology
Incidence
Represents approximately 3% of head and neck malignant neoplasms
Represents < 1% of all malignant neoplasms
Most common malignant epithelial neoplasm of sinonasal tract
Age
Most frequent in 6th and 7th decades of life
95% of cases arise in patients older than 40 years
Gender
Male > Female
Site
In decreasing order of frequency, sites of occurrence include
Antrum of maxillary sinus > nasal cavity > ethmoid sinus > sphenoid and frontal sinuses
Maxillary sinus
No lateralization
Nasal cavity
Primarily lateral wall
No lateralization
10% bilateral although may represent extension from one side via septal perforation
Nasal septum
Most arise from anterior rather than posterior septum
Nasal vestibule SCC cutaneous (not mucosal) derived
Presentation
Maxillary sinus
Early symptoms often confused with sinusitis resulting in delay in diagnosis
With progression of disease, grouped in 5 categories
Nasal: Nasal obstruction, persistent purulent rhinorrhea, nonhealing sore/ulcer, epistaxis, mass
Oral: Referred pain including to upper premolar, molar teeth, ulceration, loosening of teeth, fistula
Facial: Swelling, asymmetry
Ocular: Eyelid swelling, proptosis/exophthalmos
Neurologic: Numbness, paraesthesia, pain, cranial neuropathy
Nasal cavity
Unilateral obstruction, nonhealing sore, rhinorrhea, epistaxis
Mass
Pain in minority of cases
Treatment
Options, risks, complications
Complete surgical resection plus adjuvant radiotherapy
Surgical approaches
Surgical advances permit complex tumor removal and reconstruction surrounding these structures
Results in functional, cosmetic improvements
Prognosis
Keratinizing SCC
Maxillary sinus
Poor prognosis
Often presents with advanced clinical stage
Clinical stage of greater prognostic import than histologic type
30-45% local recurrence
Metastatic disease uncommon if tumor confined to involved sinus, but over disease course
25-30% locoregional nodal spread
10-20% distant spread
Poorer prognosis related to
Higher clinical stage disease involving more than one anatomic area
Recurrent tumor following initial curative therapy
Regional lymph node metastasis
Presence of facial numbness/swelling, orbital-related symptoms, oral cavity involvement, skin involvement
Nasal cavity
Generally > 50% 5-year survival
Approximately 20% local recurrence
Approximately 30% develop locoregional nodal spread
Approximately 20% distant spread
Spread may occur to paranasal sinuses, orbit, oral cavity, skin, cranial cavity
Patients at greater risk for 2nd primary malignancy
Other mucosal site in upper aerodigestive tract
Sites other than head and neck (e.g., lung, gastrointestinal tract, breast)
Nasal septum
60-80% 5-year survival
Approximately 11% local recurrence
Approximately 25% develop locoregional nodal spread
Approximately 15% develop distant spread
Poor prognosis related to
Tumors larger than 2 cm
Lymph node metastasis
Nasal vestibule
65-87% 5-year survival
Approximately 24% local recurrence
Approximately 18% develop locoregional nodal spread
< 5% distant spread
Poor prognosis related to
Tumors larger than 1.5 cm
Involvement of ≥ 2 sites in vestibule
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree