Solitary Fibrous Tumor, Hemangiopericytoma Type
Elisabeth J. Rushing, MD
Key Facts
Terminology
Now considered part of solitary fibrous tumor (SFT) spectrum (“cellular” or “malignant” SFT), especially at systemic sites
Clinical Issues
65% recurrence at 5 years and 90% at 12 years
Metastatic disease: 80% at 12 years
Image Findings
Hypervascular mass with prominent draining veins on arteriography
Narrow-based dural attachment
More likely to invade and destroy skull than meningioma
Microscopic Pathology
Dense cellularity interrupted by “staghorn” vessels
Pale islands
Ancillary Tests
CD34 variably (+), often patchy, can be (-)
CD99(+), variable Bcl-2(+), Leu-7(+), and FXIIIa(+)
Reticulin fibers around individual or small groups of cells in most cases
Top Differential Diagnoses
Solitary fibrous tumor
Meningioma
Mesenchymal chondrosarcoma
Melanocytic neoplasm
Gliosarcoma
Diagnostic Checklist
Necrosis indicates poor prognosis
TERMINOLOGY
Abbreviations
Solitary fibrous tumor (SFT)
Hemangiopericytoma (HPC)
Synonyms
Cellular SFT
Definitions
Highly vascular, usually dura-based malignant mesenchymal neoplasm
Now considered part of solitary fibrous tumor (SFT) spectrum (“cellular” SFT), especially at systemic sites
Prognosis less favorable in CNS
Possibly because of relative difficulty of wide excision in CNS
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon
Age
Peaks in 5th decade
Gender
Slightly more common in males
Site
Dura based, intracranial, or intraspinal
Parasagittal and falcine locations common
Rarely pineal, suprasellar, cerebellopontine angle
Presentation
Site-dependent neurological deficits
Seizures (uncommon)
Intracranial hemorrhage (rare)
Hypoglycemia from release of insulin-like growth factor (rare)
Treatment
Surgical approaches
Gross total resection
Prognostically significant
Intraoperative hemorrhage potential complication
Preoperative embolization may reduce bleeding
Adjuvant therapy
Role not yet established
Radiation
Lengthens recurrence-free interval, but minimal effect on overall survival
Prognosis
Tendency for late recurrences
Recurrences early in anaplastic examples
Metastases: Approximately 80% at 12 years
Lungs, liver, bone
Spread along CSF spaces
IMAGE FINDINGS
General Features
Best diagnostic clue
Hypervascular mass with prominent draining veins on arteriography
Location
Most are dura based
Morphology
Comparisons to meningioma
Often narrower base; less likely to have dural “tail”
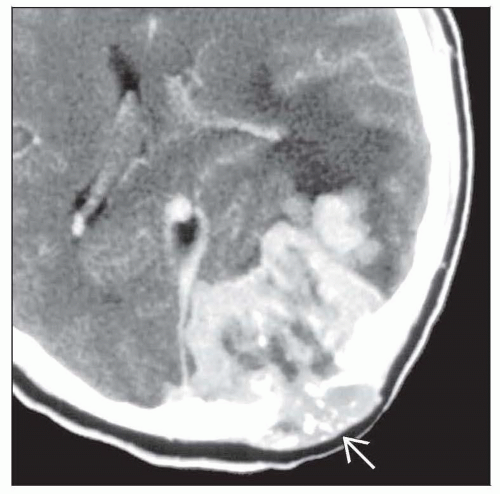
More likely to destroy skull; no hyperostosis
No tumoral calcifications, except for trapped skull
MR Findings
Isointense on T1WI; high or mixed intensity on T2WI
Variable enhancement
Internal flow voids indicate high blood flow
CT Findings
Destruction of adjacent skull (some cases)
No associated hyperostosis
No tumoral calcifications other than trapped skull
MACROSCOPIC FEATURES
General Features
Dura based, lobulated
Solid or spongy with gaping vascular channels on cut surface
Pink-gray to hemorrhagic
May invade and destroy bone
MICROSCOPIC PATHOLOGY
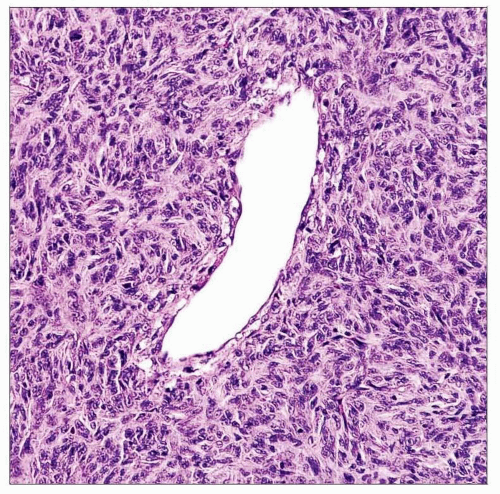
Histologic Features
Dense cellularity interrupted by “staghorn” or branching sinusoidal thin-walled vessels almost devoid of collagen
Pale, paucicellular areas (common)
Haphazard or jumbled arrangement of cells
Spindle-shaped to plump forms
Pleomorphism and nucleoli uncommon
Mitoses: Few to many
No tight whorls or psammoma bodies
Anaplastic: Necrosis or increased mitotic activity (> 5/10 HPF) plus 2 or more of the following
Hemorrhage
Increased cytologic atypia
High cellularity
Grade III
High cellularity, necrosis, and > 5 mitoses/10 HPF
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree