|
Typical Clinical Features |
Microscopic Features |
Ancillary Investigations |
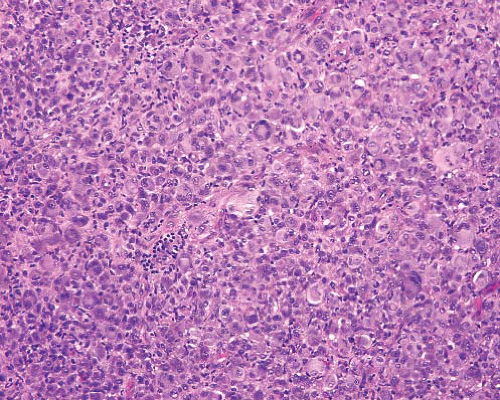
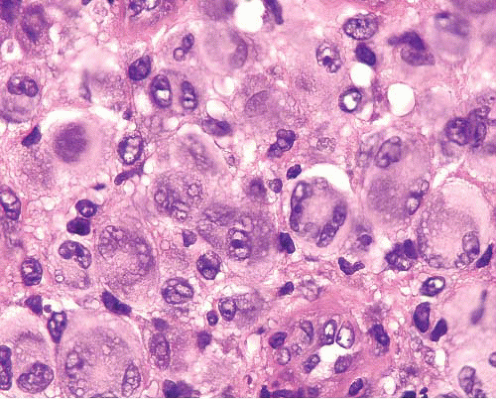
Reticulohistiocytoma |
Solitary cutaneous or multicentric reticulohistiocytosis affecting skin and synovium of joints |
Multinucleated giant cells with ground glass cytoplasm, plump histiocytes, and mixed inflammatory cells |
PAS+ (diastase resistant) CD68+, CD163+, MiTF+ (nuclear) in some |
Juvenile xanthogranuloma, cutaneous |
Infants, head and neck, trunk, proximal limbs
Yellow-brown plaque or nodule |
Infiltrative dermal lesion
Sheets of histiocytes
Older lesions have more foamy cells and more Touton giant cells |
S100 protein−, CD163+ |
Juvenile xanthogranuloma, deep |
Infants or young children, trunk, intramuscular |
Monotonous sheets of macrophages |
CD68+, S100 protein−, CD1a− |
Regenerating skeletal muscle |
Damage due to trauma or infiltrating neoplasm |
Atrophy of muscle fibers bringing nuclei into close proximity, mimicking giant cells
No cytologic atypia |
Desmin+ |
Localized tenosynovial giant cell tumor |
Any age, F > M
Usually in digits, particularly hand, but may involve larger joints
Nodular, circumscribed mass closely related to the synovium of the tendon sheath or joint |
Circumscribed
Sheets of small, histiocyte-like rounded or polygonal mononuclear cells, with varying numbers of osteoclast-like giant cells, foamy histiocytes, siderophages, and other inflammatory cells
Hemosiderin deposition |
Osteoclast-like giant cells and proportion of mononuclear cells CD68+
Desmin+ dendritic cells in up to 50% of cases |
Diffuse tenosynovial giant cell tumor |
Young adults
Papilliform lesion within the synovium; can spread into surrounding soft tissue
Extra-articular form has no connection to adjacent joint; usually in periarticular soft tissue but sometimes muscle |
Infiltrative margins, sheet-like patterns of mixture of mononuclear cells, osteoclast-like giant cells along with foamy cells, siderophages, and other inflammatory cells
Variable cellularity with looser zones
Cleft-like spaces |
Immunophenotype similar to that in localized giant cell tumor |
Giant cell tumor of soft parts (low grade) |
Typically middle-aged adults
Extremities, trunk, abdomen and pelvis, and head and neck
More common in superficial than deep soft tissue |
Multinodular, cellular nodules of multinucleated osteoclast-like giant cells distributed among mononuclear cells
Divided by collagenous septa with hemosiderinladen macrophages
Mononuclear and giant cells show vesicular, round to oval nuclei lacking atypia
Mitoses
Vascular invasion in some tumors |
CD68+ (diffuse and strong in osteoclast-like giant cells, focal in mononuclear cells)
Variable SMA+ in mononuclear cells. CK and S100 protein+ (focally in occasional tumors) |
Phosphaturic mesenchymal tumor |
Frequently associated with oncogenic osteomalacia
Soft tissue, particularly limbs
Symptoms abate with removal of tumor |
Low to focally moderate cellularity
Sheets of spindle to stellate cells with small, bland nuclei, within calcified smudgy myxoid to myxochondroid matrix
Mitotic activity absent to very low
Thin-walled branching hemangiopericytic vessels
Osteoclast-like giant cells |
FGF23+ in most tumors |
Tumoral calcinosis |
Painless subcutaneous mass near joints or in extremities |
Multilocular cyst
Fibrosing granulomatous giant cell reaction around crystalline amorphous or calcified material |
Nodular fasciitis |
Young adults, short history, sometimes previous trauma, size <5 cm |
Loose fascicles of spindle and stellate cells in myxoid stroma, extravasated erythrocytes, lymphocytes
Small multinucleated cells in later stages |
SMA+ |
Dermatofibroma |
Dermal lesions |
Epidermal hyperplasia
Storiform pattern of bland spindle cells with foamy histiocytes
Trapping of peripheral collagen bundles
Hemosiderin and mixed chronic inflammation
Touton-type giant cells |
Factor XIIIa+, variable calponin and SMA+ |
Plexiform fibrohistiocytic tumor |
Children to young adults. F > M
Most often in upper extremities
Small dermal or subcutaneous lesions |
Multinodular or plexiform arrangements of histiocyte-like cells, spindle fibroblast-like cells and multinucleated, often osteoclast-like giant cells |
Giant cells and histiocyte-like cells CD68+, fibroblast-like cells SMA+ |
Giant cell malignant fibrous histiocytoma |
Older adults
Deep soft tissue of limbs or trunk |
Sheets and fascicles of markedly anaplastic spindle to ovoid cells
Giant cells are predominantly osteoclast-like, but atypical tumor giant cells can also be present |
Osteoclast-like giant cells CD68+ |
Giant cell fibroblastoma |
Children in first decade
Dermis and subcutis |
Loose fascicles of spindle cells in abundant collagenous to myxoid stroma
Variable numbers of scattered multinucleate stromal cells with central closely packed small dark nuclei arranged in wreath-like formations
Pseudovascular spaces rimmed by spindle and giant cells |
CD34+
COL1A1-PDGFRB fusion transcripts |
Pleomorphic lipoma |
Neck and back
M > F
Subcutis |
Admixture of mature adipocytes, bland spindle to ovoid cells, floret cells, and rope-like collagen bundles
Floret cells are multinucleate giant cells with hyperchromatic, radially arranged wreath-like nuclei |
CD34+ (strong in spindle cells)
Variable S100 protein+ |
Leiomyosarcoma with osteoclast-like giant cells |
Older adults
Retroperitoneum, extremities
Also in skin and subcutis and large blood vessels |
Intersecting fascicles of spindle cells with bluntended nuclei, paranuclear vacuolations, and eosinophilic cytoplasm |
SMA, desmin, and h-caldesmon+ |
Carcinoma with osteoclast-like giant cells |
Primary site may be evident |
Nested architecture, epithelioid cells |
CK+, EMA+ |