Small Bowel Resection and Anastomosis
Small bowel resection is performed when a segment of small intestine must be removed. The nature of the pathology dictates the extent of resection. Carcinoma of the small intestine is rare. Resection for carcinoma should encompass margins of at least 10 cm and a fan-shaped piece of mesentery containing regional nodes. Resection for benign disease is far more common. In the latter case, margins should be conservative, and as much bowel as possible should be preserved. This is particularly true when reoperations may be necessary (e.g., in patients with Crohn’s disease). Strictureplasty, a popular alternative to resection in patients with Crohn’s disease, is briefly presented at the end of this chapter.
When a significant length of small intestine must be removed, measure the length of the remaining bowel. Take a wet umbilical tape and measure the length along the antimesenteric border with the bowel under slight stretch. Record the measured length in the operative note.
Steps In Procedure—Small Bowel Resection
Midline laparotomy
Run small intestine from ligament of Treitz to ileocecal valve
Identify segment to resect, and eviscerate it
Return the rest of the bowel to the abdominal cavity
Grasp the bowel and identify avascular window in mesentery adjacent to bowel at sites of proposed resection
Extent of resection depends on pathology
Wider resection with generous fan of mesentery is needed for malignancy
Create window under bowel
Divide bowel
Divide mesentery in V-shaped fashion
Check ends for viability (resect additional bowel if necessary)
Create anastomosis (stapled or sutured)
Close mesenteric defect
Wrap omentum around anastomosis
Check hemostasis and close abdomen without drains
Hallmark Anatomic Complications—Small Bowel Resection
Anastomotic leak
List of Structures
Jejunum
Ileum
Cecum
Ileocecal valve
Suspensory ligament of duodenum (ligament of Treitz)
Small Bowel Resection (Fig. 74.1)
Technical Points
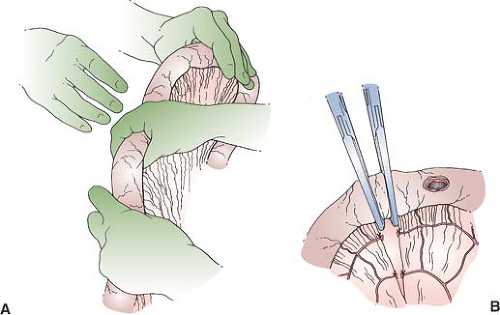
Always “run” the entire small intestine before any resection. Grasp a section of small bowel and pass it from one hand to the other, “walking” your fingers proximally. You should be progressing in the general direction of the left upper quadrant. Identify the suspensory ligament of duodenum (ligament of Treitz). Progressing distally from the ligament of Treitz, elevate a section of small bowel about 10 cm in length. Flip each section over so that both sides are examined. Then pass the section to your first assistant. Continue in this fashion to the ileocecal valve. If, by chance, the loop of bowel that you grasp in the beginning leads you to the ileocecal valve instead of the ligament of Treitz, it is perfectly acceptable to run the bowel from distal to proximal, finishing at the ligament of Treitz. Minimize the amount of time that the bowel is out of the abdomen. Interference with venous drainage, swelling, and hypothermia can result from prolonged evisceration. Return all bowel, with the exception of the segment to be resected, to the abdomen.
Grasp the bowel between the thumb and forefinger of your nondominant hand and use your thumb to feel the mesenteric border of the bowel at one of the planned resection margins. Take a fine-pointed mosquito hemostat and pass it under one of the small vessels that supply the bowel. Double-clamp and ligate the vessel with fine silk. Do not try to break through on your first pass unless the mesentery is very flimsy. Divide the mesentery close to the bowel with precision to minimize the bulk of tissue included in ligatures next to the bowel. The mesenteric surface of the bowel will then be clean and ready for anastomosis.
Clamp the bowel with Allen clamps or similar straight clamps designed to hold bowel securely. Kocher clamps will work if nothing else is available. Divide the bowel between the clamps with a scalpel.
Repeat this process at the other end of the segment to be resected.
Lift the bowel up to display the mesentery and identify the line along which you plan to resect it. With the mesentery slightly stretched, place the opened blade of a pair of Metzenbaum scissors into the incision in the mesentery and lift up, elevating a flap of peritoneum with the tip of the blade. Push-cut the peritoneum by pushing with the crotch of the barely opened scissors, outlining a V-shaped segment of mesentery to be resected. This cut should not injure the underlying mesenteric vessels. Flip the bowel over and do the same thing on the other side of the mesentery. Use the thumb and forefinger of your nondominant hand to elevate the thin, fatty mesentery. A finger fracture technique is sometimes useful. Double-clamp and divide all mesenteric vessels, and remove the resected segment.
Secure the mesenteric vessels with suture ligatures of 3-0 silk.
Anatomic Points
Running the bowel allows the surgeon to inspect the entire length of small bowel for disease or incidental developmental anomalies. The most common anomaly is Meckel’s diverticulum, which has been reported to be present (although is usually asymptomatic) as frequently as 4.5% of the time.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree