Sleep
On March 4, 1984, an 18-year-old woman named Libby Zion died at Cornell Medical Center’s New York Hospital. The cause of death was a drug-drug interaction, which occurred when an opioid (meperidine) she was given in the emergency room interacted with a prescription antidepressant (monoamine oxidase inhibitor) she had been taking. Her father, Sidney Zion, a writer for the New York Times, sued the hospital (Zion vs. New York Hospital), claiming that his daughter’s medical care had been inadequate because she had been treated by unsupervised, sleep-deprived house officers. The grand jury for the case noted that medical residents at New York Hospital commonly worked more than 100 hours per week, including shifts of more than 24 hours each. The jury found that such physician-training methods, common across the United States at that time, were potentially dangerous to patients (Kwan, 2002). This case and subsequent responses to it by government agencies resulted in the Bell Regulations: New York State Health Code (DeBuono & Osten, 1998), considered a national model for residency training that led to reforms in graduate medical education nationwide. The Bell Regulations include
Twelve-hour work limits for residents and attending physicians in emergency departments.
Work periods not exceeding 24 hours consecutively in areas other than the emergency room.
Scheduled work week for resident physicians not exceeding an average of 80 hours per week over a 4-week period.
At least one 24-hour period of nonworking time per week.
Twenty-four-hour supervision of acute care inpatient units by experienced attending physicians.
Improved working conditions and ancillary support for resident physicians.
Although these regulations were an important step toward reform, American hospitals do not always observe these suggested guidelines, and the effects of sleep deprivation still have the potential to cause significant problems during residency training.
It may be difficult for those who do not have the opportunity to sleep to empathize with those who have the opportunity but are unable to sleep. However, insomnia is common, occurring in at least one-third of all adults at some time in their lives. Insomnia and other sleep disorders may be early indications of physical or emotional illness. Understanding the requirements for and physiology of normal sleep enables physicians to provide effective interventions for their patients with sleep disturbances and helps ensure that they themselves obtain adequate, high-quality sleep.
• NORMAL SLEEP
Some fortunate individuals can function well on 5 or 6 hours of sleep, whereas others need at least 9 or 10 hours. Most healthy people need about 8 hours of sleep per night. Human beings are not unique in their need for sleep—other mammals that have been studied, including nonhuman primates and rodents, sleep for some portion of their circadian period.
Over the last few decades, progress has been made in understanding the physiology of sleep, including its electroencephalographic characteristics, states, stages, and patterning, or architecture. However, even after many years of study, it is still not clear how sleep restores function and preserves health.
The electroencephalogram in waking and sleeping
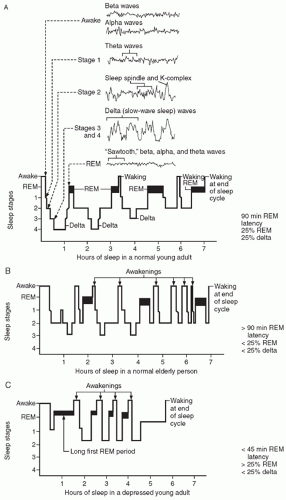
During the awake state, the electroencephalogram (EEG) shows characteristic brain waves. With active mental concentration, beta waves (15 to 30 cycles per second [cps]) over the frontal lobes predominate. Alpha waves (8 to 12 cps) over the occipital and the parietal lobes are seen when an awake person relaxes with closed eyes and becomes drowsy (Fig. 7-1A).
The two major physiological states in normal sleep are rapid eye movement (REM) and nonrapid
eye movement (NREM) sleep. The former is characterized by fast-wave EEG activity, and the latter includes a progression through four stages of increasing depth and slowing of the EEG (see Fig. 7-1).
eye movement (NREM) sleep. The former is characterized by fast-wave EEG activity, and the latter includes a progression through four stages of increasing depth and slowing of the EEG (see Fig. 7-1).
Non-REM sleep. Non-REM sleep, which makes up approximately 75% of total sleep time, is identified by slow eye movements, high amplitude, lowfrequency brain waves, and increased muscle tone. Stage 1 takes up about 5% of total sleep time and is characterized by low-voltage theta wave activity at 3 to 7 cps. Stage 1 quickly changes to stage 2.
Stage 2 sleep is associated with spindle-shaped waves at 12 to 14 cps (sleep spindles) and slow, high-amplitude groups of waves called K-complexes. Stage 2 makes up 45% of sleep time in young adults, more than any other one stage. This stage is associated with tooth grinding or bruxism, a chronic condition that can lead to tooth and gum problems, jaw pain, and headaches.
Stages 3 and 4 sleep are collectively known as slow-wave or delta sleep that is characterized by high-voltage delta waves at 1 to 3 cps. Delta sleep takes up about 25% of sleep time in young adults and occurs mainly during the first half of the sleep cycle. Delta is the deepest part of NREM sleep and can be associated with unusual behavioral characteristics such as sleepwalking (somnambulism), bed wetting (enuresis), and night terrors (see later text).
REM sleep. REM sleep is characterized by rapid eye movements, decreased muscle tone, and lowamplitude, high-frequency brain waves (including alpha and beta waves) that form a tracing resembling the teeth of a saw (sawtooth waves). It makes up about 25% of total sleep time in young adults, occurs primarily during the second half of the sleep cycle, and is associated with high levels of brain activity and dreaming. When compared with people in other stages of sleep, people in REM sleep are less likely to be woken by external stimuli but are more likely to wake spontaneously.
The average time to the first REM period after falling asleep, REM latency, is 90 minutes. Shortened REM latency is seen in patients with major depressive disorder and is one of the identifying signs of the sleep disorder called narcolepsy (see later text). After the first REM period, people normally experience REM periods of 10 to 40 minutes, each occurring about every 90 minutes throughout the night.
REM sleep also is characterized by suppression of sympathetic activity as shown by miosis (pupil constriction), as well as penile and clitoral erection. However, except for skeletal muscles controlling respiration and movements of the eyes and middle ear ossicles, the body is essentially paralyzed (i.e., atonic) during REM sleep.
REM sleep behavior disorder (RBD) is a rare condition that includes episodes of REM without muscle atonia. The resulting physical activity associated with dreaming or nightmares can lead the patient with this disorder to harm himself or his sleep partner during an REM sleep period. RBD has been associated in some patients with the development years later of Parkinson’s disease and Lewy body dementia.
The physiological importance of REM sleep can be demonstrated by the phenomenon known as REM rebound. In this situation, people deprived of sleep one night because of repeated awakenings or use of sedative agents (which depress REM sleep) experience a rebound or increase in REM sleep during the next sleep period. This rebound phenomenon, coupled with the findings of sleep studies conducted in conjunction with learning studies, has led to the hypothesis that REM sleep and dreaming are important in learning and memory consolidation. Research studies, however, have failed to support this hypothesis, and the ultimate function of REM sleep remains unknown (Siegel, 2001).
Sleep architecture. Sleep progresses through the four stages of NREM, which then occur in reverse order back to stage 1, typically followed by a period of REM. Although NREM sleep stages and REM periods may be missed or repeated, five to six cycles of NREM sleep with an REM period occur per night, each cycle taking about 90 minutes. This produces a structure known as sleep architecture (Fig. 7-1). Aging, psychopathological states such as depression, and use of psychoactive agents can affect sleep architecture.
Aging is associated with changes in sleep architecture. Neonates sleep about 16 hours per day, 50% of it in REM. By young adulthood, the percentage of REM sleep has decreased to 25%. The sleep architecture of the elderly is characterized by a combination of changes that often result in nonrestful sleep and daytime tiredness. These changes include
Prolonged sleep latency
Further reduction in REM sleep
Decreased total sleep time
Decreased delta sleep
Increased nighttime awakenings (Fig. 7-1B)
Depression is also associated with alterations in sleep architecture. Depressed patients characteristically show
Relatively normal sleep latency (time from going to bed to falling asleep) of less than 20 minutes or prolonged sleep latency
Short REM latency (appearance of REM within about 45 minutes of falling asleep)
Increased REM early in the sleep cycle
Decreased REM later in the sleep cycle (may be associated with the early morning awakening [terminal insomnia] that specifically characterizes sleep in depression)
Long first REM period
Increased total REM
Decreased delta sleep
Increased nighttime awakenings (Fig. 7-1C)
Evidence suggests that increased REM sleep may not only result from depression, but also be related to its pathophysiology. For example, drugs that increase the percentage of REM sleep (e.g., reserpine, an antihypertensive agent) or reduce the percentage of REM sleep (e.g., heterocyclic antidepressants) respectively, exacerbate and improve depressive symptoms. Also, restriction or deprivation of REM and NREM sleep in depressed patients leads to temporary improvement in their depressive symptoms.
Sleep deprivation
As the Zion case demonstrated, normal individuals deprived of sleep experience impaired physical and mental performance. If the deprivation persists, they may show psychiatric symptoms such as confusion, agitation, and, ultimately, pathological anxiety and psychotic symptoms such as paranoid delusions and hallucinations (Case 7-1).
case 7.1
THE PATIENT
During the 30th hour of a marathon radio program aimed at raising money for charity, the host, a 20-year-old college student who has no history of emotional or medical problems, begins to have difficulty concentrating and seems confused. By the 50th hour of the marathon, the student is agitated, refuses to eat anything his assistants bring him, and states, “I know you are all trying to poison me.” His colleagues become alarmed at his behavior and call 911. On the way to the hospital, the student starts shouting that everyone is against him. He is restrained after punching the emergency medical technician.
COMMENT
This student is showing the emotional effects of extended sleep deprivation. These effects include initial confusion, agitation, and aggression, and, with extended deprivation, symptoms suggesting a loss of touch with reality including delusional thinking (e.g., the belief that people are trying to harm him).
MANAGEMENT
The obvious initial management of this student is to allow him to sleep. However, because he is agitated and has psychotic symptoms (e.g., delusions), he could injure himself or others before he is able to fall asleep. The antipsychotic agent risperidone (Risperdal) is a good choice to reduce the student’s agitation and delusional thinking. Antipsychotics also have the beneficial side effect in this instance of causing general sedation. High-potency agents such as haloperidol (Haldol) can also be used but probably should be avoided in this case because young men are at particular risk for acute dystonic reactions when treated with these agents (see Chapter 19).
Not only is sleep required for optimal physical and mental performance, but it may also be necessary for life itself. Fatal familial insomnia, a rare disorder resulting from mutations in the prion protein gene, leads to degeneration of the thalamus, a brain region associated with arousal and consciousness (see Chapter 5). This degeneration results in the complete inability to sleep, followed by dementia. It is also, as the name of the disorder implies, fatal within 1 to 2 years (Parchi et al., 1998).
Neurotransmitters and the production of sleep
Because the monoamines are closely involved in the production and maintenance of sleep, use of psychoactive medications that alter their availability results in alterations in sleep patterns and sleep quality.
Serotonin and acetylcholine promote sleep. Specifically, increased availability of serotonin is associated with increased total sleep time and increased delta sleep. In contrast, reduction in serotonin by events like damage to the neural structures that produce it (e.g., the dorsal raphe nuclei) decreases these measures. Although ingestion of melatonin itself, a serotonin metabolite manufactured by the pineal gland during darkness, has not been shown to improve sleep, ramelteon (Rozerem) a melatonin agonist (see Chapter 18), has been approved by the Food and Drug Administration (FDA) to treat insomnia.
Acetylcholine (ACh) in the reticular formation is associated with inducing REM sleep. In patients with conditions associated with decreased ACh, such as normal aging and Alzheimer’s disease, REM sleep, total sleep time, and delta sleep are decreased.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree