Sinonasal Inflammatory Polyp
Bruce M. Wenig, MD
Key Facts
Terminology
Nonneoplastic inflammatory swellings of the sinonasal mucosa
Etiology/Pathogenesis
Etiology linked to multiple factors
Clinical Issues
Most arise from lateral nasal wall or from ethmoid recess
Nasal obstruction, rhinorrhea, and headaches
Polypectomy
Approximately 50% of patients will have recurrence following surgery
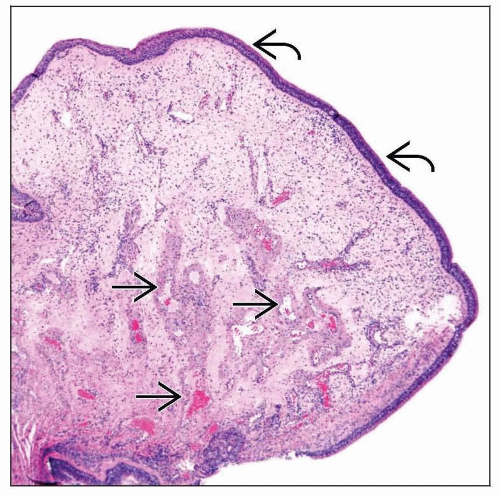
Microscopic Pathology
Surface ciliated respiratory epithelium typically intact; may show squamous metaplasia
Markedly edematous stroma noteworthy for absence of mucoserous glands
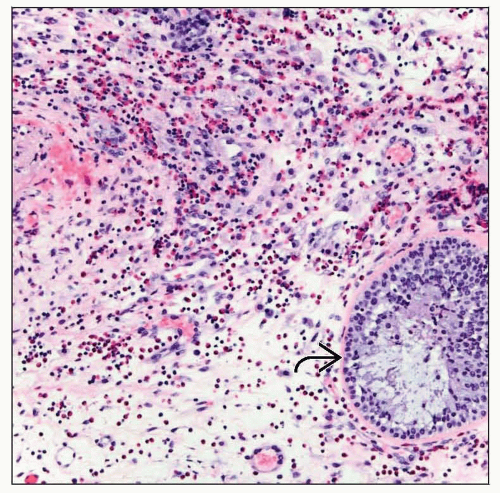
Mixed chronic inflammatory cell infiltrate predominantly composed of eosinophils, plasma cells, and lymphocytes
Secondary changes may include
Surface ulceration
Fibrosis
Infarction
Granulation tissue
Atypical stromal cells
Granuloma formation
Deposition of amyloid-like stroma
Osseous &/or cartilaginous metaplasia
TERMINOLOGY
Definitions
Nonneoplastic inflammatory swellings of sinonasal mucosa
ETIOLOGY/PATHOGENESIS
Multifactorial
Etiology linked to multiple factors including
Allergy (atopy)
Infections
Cystic fibrosis
Diabetes mellitus
Aspirin intolerance
Familial
CLINICAL ISSUES
Epidemiology
Age
Occurs in all ages but commonly seen in adults over 20 years old
Rarely seen in children less than 5 years old
Exception in patients with cystic fibrosis who develop nasal polyps in 1st and 2nd decades of life
Gender
Equal gender distribution
Site
Most arise from lateral nasal wall or ethmoid recess
Normal physiologic parameters of lateral nasal cavity mucosa are such that prominent edema readily forms in mucosal lamina propria
Makes this site more susceptible to development of polyps
May be unilateral or bilateral, single or multiple
Not infrequently, involvement of both nasal cavity and paranasal sinuses
Presentation
Nasal obstruction, rhinorrhea, and headaches
Samter triad
Nasal polyps, asthma, and aspirin intolerance
Rarely, may be associated with bone erosion, destruction, blindness
Endoscopic Findings
Mulberry turbinate
Clinical term referring to swollen nasal turbinate tissue
Formed as result of edema interspersed among thick vessel walls of normal turbinate vascularity
Appearance may clinically suggest pathologic process, such as vascular malformation
Treatment
Options, risks, complications
Identification and treatment of possible etiologic factor(s) is initial approach in treatment
Surgical approaches
Polypectomy
Medial maxillectomy (Caldwell-Luc procedure) including removal of stalk for antrochoanal polyps
Drugs
Patients with cystic fibrosis may respond to medical therapy, but surgical resection may be required
Prognosis
Approximately 50% of patients will have recurrence following surgery
Recurrence rates highest in patients with aspirin intolerance and asthma
Development of functional endoscopic sinus surgery contributed to
Decreasing morbidity of sinonasal surgery and recurrence of nasal polyposis in patients with cystic fibrosis
Improving sinonasal-related symptomatology for asthmatic patients
IMAGE FINDINGS
General Features
Soft tissue densities, air-fluid levels, mucosal thickening, and opacification of paranasal sinuses
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree