Sigmoid Colectomy: Single-Incision Laparoscopic Surgery Technique
Rodrigo Pedraza
Eric M. Haas
DEFINITION
Single-incision laparoscopic sigmoidectomy is a minimally invasive technique in which a sigmoid colectomy is performed laparoscopically through a single-port device. The entirety of the procedure is accomplished using one sole incision through which all the laparoscopic instruments are placed.
Reduced port single-incision laparoscopic sigmoidectomy is a modified technique in which the single-port device is placed through a Pfannenstiel incision and an additional port is placed through the umbilicus. This technique is also called “single plus one” sigmoidectomy1 and is used to facilitate operative exposure, avoid instrument conflict, and benefit from the Pfannenstiel incision—diminished infection, dehiscence, and hernia rates.
PATIENT HISTORY AND PHYSICAL FINDINGS
Single-incision laparoscopic sigmoidectomy is safe and feasible for essentially all benign and malignant sigmoid diseases requiring resection.2, 3, 4 The most common indications include diverticular disease, cancer, and polyps.
Patients with diverticular disease typically present with recurrent episodes of diverticulitis or complications such as perforation or obstruction. Left lower quadrant pain and tenderness are commonly encountered and may be accompanied with nausea, vomiting, and fever. Lower gastrointestinal (GI) bleeding is rarely present.
Cancer and polyps of the sigmoid colon are frequently diagnosed incidentally during screening colonoscopy. Those with large polyps or malignancy may present with hematochezia, bowel obstruction, perforation, or lower abdominal or pelvic pain.
Single-incision laparoscopic sigmoidectomy is contraindicated in patients who cannot tolerate major abdominal surgical procedures, such as those with severe hemodynamic instability, recent myocardial infarction, or severe thromboembolic event.
History of prior abdominal surgery may lead to a prolonged procedure due to extensive lysis of adhesions; nonetheless, it is not an absolute contraindication to the use of the singleincision approach.
The procedure may be performed in patients with high body mass index (BMI). However, the high complexity and high conversion rates make this a less ideal scenario for singleincision sigmoidectomy. In patients with high BMI, conventional multiport or hand-assisted laparoscopic technique may be more suitable.
Large, bulky tumors may require further incision lengthening during the procedure, losing pneumoperitoneum, thus hindering the ability to complete the case with the single-incision technique. Nevertheless, some single-port devices allow incision lengthening without compromising the pneumoperitoneum.
Surgeons without experience with single-incision colectomy may encounter technical difficulties. Before offering this approach, competency with conventional multiport and/or hand-assisted laparoscopic techniques is recommended. Additionally, it is suggested that the surgeon becomes proficient in single-incision sigmoidectomy in those with benign disease prior to performing oncologic resections.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Regardless of the procedure indication, all patients necessitate appropriate preoperative evaluation with endoscopic and radiologic studies.
For patients with diverticular disease, colonoscopy or flexible sigmoidoscopy is warranted to assess the length of the affected bowel, to determine resection levels, and to confirm the diagnosis. Furthermore, a computed tomography (CT) scan of the abdomen and pelvis is mandatory to evaluate the severity of the pericolonic disease. Some patients with severe active disease demonstrated on the CT scan may benefit from a course of antibiotics or even abscess drainage prior to the procedure.
If the indication for the sigmoidectomy is a colonic polyp or malignancy, endoscopic tattooing of the lesion is required to ensure proper location during the laparoscopic procedure (FIG 1).
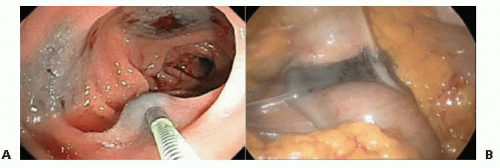
FIG 1 • Tattooing the lesion in at least three quadrants of the bowel wall during colonoscopy (panel A) facilitates proper location of the pathology during the laparoscopic approach (panel B).
For malignant cases, a complete oncologic workup is mandatory. A multidisciplinary approach involving surgeon and medical oncologist is preferable. Lymph node and distant organ involvement are evaluated with the CT scan of the abdomen and pelvis and positron emission tomography (PET) scan. Patients with lower tumors in the rectosigmoid junction may need magnetic resonance imaging (MRI) to evaluate tumor local progression into the pelvis and lymph node status.
SURGICAL MANAGEMENT
Preoperative Planning
Bowel preparation is traditionally achieved through a polyethylene glycol-based laxative solution and oral antibiotics. This practice has recently been called into question. An accepted alternative is the use of a modified bowel preparation with preoperative enema to clear out the distal stool.
In the operating room and under anesthesia, rigid proctosigmoidoscopy is recommended to ensure the level of the lesion is above the rectum and to ensure that the bowel is clean of fecal matter.
For noncontaminated cases, prophylactic antibiotics are administered according to the Surgical Care Improvement Project (SCIP) measures.
If the cases involve active infection such as those with recurrent diverticulitis or perforation, broad-spectrum antimicrobials with gram-negative and anaerobe bacterial coverage are chosen.
Positioning
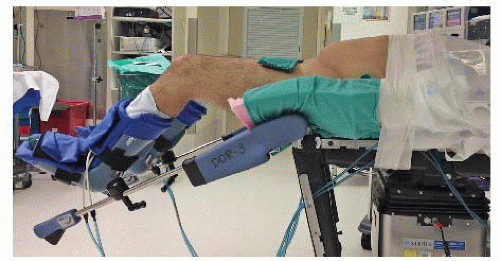
The patient is placed in a modified lithotomy position with both arms tucked at the patient’s side. The patient is secured with adhesive tape over the chest, without compromising chest expansion (FIG 2). Antislip rubber pads may be used to further secure the patient to the operating room table. It is imperative to ensure proper and secured positioning, as later in the procedure, Trendelenburg position will be required.
The optimal modified lithotomy position is achieved with a 25- to 30-degree thigh flexion and with moderate thigh abduction (FIG 2). This positioning allows adequate surgeon maneuverability, avoiding conflict with the patient’s thighs while affording proper perineal access.
For abdominal entry, laparoscopic exploration, and lysis of adhesions, the patient is in supine position. In this portion of the procedure, the surgeon and assistant are located on the right and left side, respectively.
Thereafter, the patient is placed in Trendelenburg position with the left side elevated. The surgeon and assistant are located on the right side of the patient with the laparoscopic monitor on the left (FIG 3).
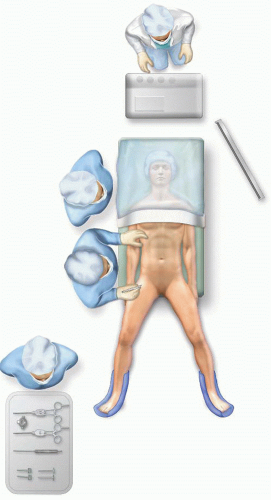 FIG 3 • Operative room patient/surgeon configuration for single-incision laparoscopic sigmoid colectomy. |
TECHNIQUES
INCISION AND PORT PLACEMENT
Typically, a 2.5-cm vertical umbilical skin incision is performed (FIG 4). The umbilical stump is divided, affording fascial lengthening to 4 cm without modifying the skin incision (FIG 4). Following entry into the abdominal cavity, the single-port device is placed.
An alternative approach is the abdominal entry using a 4-cm Pfannenstiel incision (FIG 5). This modification improves cosmetic outcomes while decreasing wound infection and hernia rates. This approach is challenging, as the instruments are in close proximity with the target operative field, limiting maneuverability. Thus, when this approach is used, we favor a single plus one technique using a Pfannenstiel incision with an additional 5-mm incision for the camera in order to avoid instrument conflict (FIG 5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree