Selective Neck Dissection for Melanoma
Vasu Divi
DEFINITION
The goal of a selective neck dissection for melanoma is the complete removal of the lymph nodes and lymphatics that drain a specific region of skin in the head and neck.
This procedure is performed for patients presenting with clinically evident regional metastasis as well as for patients with a positive sentinel lymph node.
PATIENT HISTORY AND PHYSICAL FINDINGS
All patients with melanoma of the head and neck should undergo palpation of the regional lymphatics, including the parotid glands and cervical levels 1 to 5.
Melanomas at the junction of the neck and the chest, back, or shoulder should also include palpation of the axillary lymph nodes.
All patients with melanoma, particularly those with proven regional metastases, should have a focused review of symptoms, looking for symptoms concerning for metastatic disease.
All patients with melanoma should also have a complete skin exam, looking for second primary cutaneous malignancies.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Preoperative imaging of the neck is not necessary in patients without clinically evident neck disease.
In patients with palpable adenopathy
Imaging by contrast-enhanced computed tomography (CT) scan is generally recommended to evaluate the extent of disease.
Fine needle aspiration is used to obtain pathologic diagnosis of the enlarged lymph node.
In cases of distant metastatic disease, the need for selective neck dissection is balanced against the life expectancy of the patient. In many cases, achievement of regional control in the neck is preferred, given the complications of untreated disease in the head and neck.
SURGICAL MANAGEMENT
Preoperative Planning
Determination of the type of neck dissection to be performed is based on the location of the primary tumor and location of neck disease.
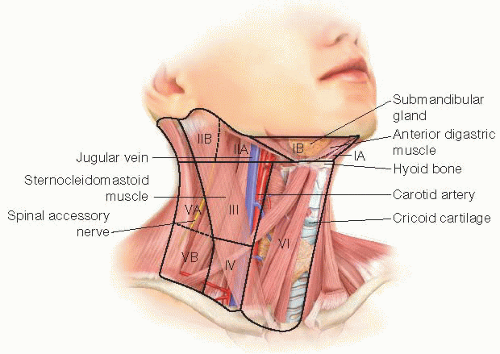
The relevant lymphatic basins of the head and neck include the parotid lymph nodes, levels 1 to 5, and the postauricular lymph nodes (FIG 1).
This serves as a rough guide to when different lymphatic basins should be addressed; ultimately, the clinician should dissect all lymphatic basins that could potentially be harboring clinical disease based on an understanding of lymphatic drainage patterns.
The removal of the superficial lobe of the parotid gland is performed for any primary cutaneous tumor anterior to the external auditory canal and above the angle of the mandible.
Levels 1 to 4 are dissected with any lesion involving the scalp anterior to the plane of the external auditory canal, facial skin, or anterior neck skin.
Levels 2 to 5 are dissected with any lesion involving the scalp posterior to the plane of the external auditory canal or posterior neck skin.
If the primary lesion is in the scalp and located very close to the plane of the external auditory canal, dissection should include levels 1 to 5.
Positioning
Patients are placed supine with the top of the head at the edge of the surgical bed.
A bump is placed underneath the shoulder blades to allow for extension of the neck, being careful to maintain support of the head on the operating room (OR) table.
TECHNIQUES
SELECTIVE NECK DISSECTION LEVELS 1 TO 4
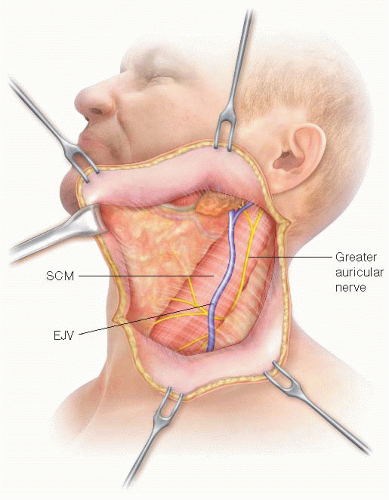
A curvilinear incision is made midway between the angle of the mandible and the clavicle; the incision travels within a neck crease, extending a few centimeters from the mastoid tip toward the approximate midpoint of the thyroid cartilage (FIG 2).
Skin is incised down through the subcutaneous tissue and platysma.
Subplatysmal skin flaps are elevated to expose the deeper contents overlying levels 1 to 4 of the neck; this will extend to the mentum, along the strap musculature in the midline, to the posterior border of the sternocleidomastoid muscle (SCM), and down to the level of the clavicle (FIG 3).
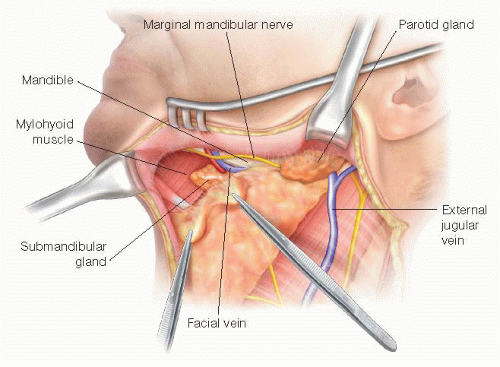
The marginal mandibular nerve is identified in the superficial layer of the cervical fascia near the angle of the mandible and is identified using nerve stimulation. The nerve is dissected free and elevated over the plane of the mandible (FIG 4).
The facial artery and vein are identified and ligated as they cross over the plane of the mandible.
The tissue over the mandible is then incised from the mentum to the angle of the mandible, taking care not to injure the previously dissected marginal mandibular nerve. This tissue is pulled inferiorly, taking care to remove the perifacial lymph nodes located near the facial vessels. During this
dissection, the retromandibular vein may be identified and ligated as it travels through the tail of the parotid gland.
Incise soft tissue over contralateral anterior belly of the digastric muscle from mentum down to hyoid bone.
Begin elevating contents of level 1A by pulling tissue laterally off the mylohyoid muscle toward the ipsilateral anterior belly of the digastric muscle; this will require division of tissue along the hyoid bone inferiorly.
Bring packet of tissue over ipsilateral digastric and back onto mylohyoid until the edge of the mylohyoid is reached see FIG 4.
Retract the mylohyoid muscle medially to allow for exposure of the contents deep to the submandibular gland. This may require some blunt dissection in this area. Identify the hypoglossal nerve, lingual nerve, and submandibular duct (FIG 5).
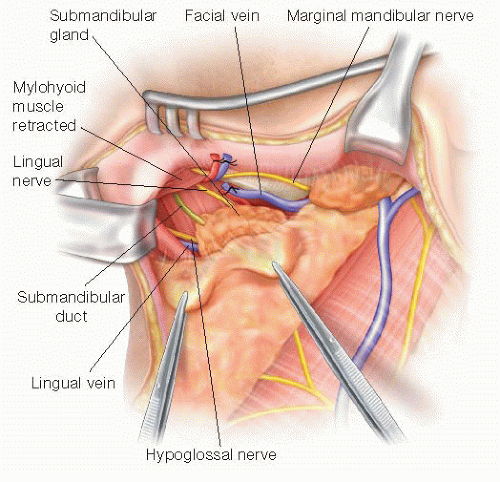
FIG 5 • The mylohyoid muscle is retracted anteriorly exposing the lingual nerve, submandibular duct, and hypoglossal nerve. The hypoglossal nerve is in a deeper plane than the lingual nerve and is only exposed after dividing the overlying fascia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access