Sebaceous Carcinoma
David Cassarino, MD, PhD
Key Facts
Terminology
Adnexal carcinoma that often lacks clear cell features in poorly differentiated cases
Etiology/Pathogenesis
Strong association with MTS if patients have multiple sebaceous tumors
Clinical Issues
Eyelids are the most common site (˜ 75% of cases)
Mohs excision is effective in most cases
Aggressive tumors with high incidence of metastasis (> 30%) and generally poor prognosis unless discovered early
Microscopic Pathology
Dermal-based infiltrative, nodular to sheet-like tumor
Often focal follicular &/or epidermal connections
Well-differentiated tumors show clear cell changes
Moderately and poorly differentiated tumors show few to rare clear cells
Often show basaloid or squamoid features
Mitotic figures are usually abundant
Areas of comedonecrosis are common
Ancillary Tests
EMA(+) in well-differentiated cases, but often lost in poorly differentiated tumors
AR(+) in most cases, including poorly differentiated
Top Differential Diagnoses
Clear cell squamous cell carcinoma (SCC)
Clear cell basal cell carcinoma (BCC)
Other primary cutaneous adnexal carcinomas
Metastatic carcinoma to the skin
TERMINOLOGY
Synonyms
Sebaceous adenocarcinoma
Definitions
Malignant adnexal tumor of sebaceous cells
Often lacks clear cell features in poorly differentiated cases and may show basaloid or squamoid features, leading to high incidence of misdiagnosis
ETIOLOGY/PATHOGENESIS
Unknown in Most Cases
Some cases likely due to solar (UV) damage, as most occur on sun-damaged skin of elderly
Genetic
Strong association with Muir-Torre syndrome (MTS) in patients who have multiple sebaceous tumors &/or multiple keratoacanthomas and internal organ malignancies
Genes implicated include MLH1, MSH2, MSH6
Encode mismatch repair proteins
Mutations lead to microsatellite instability (MSI)
MSI assays and immunohistochemistry can be used to screen for Muir-Torre syndrome
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon tumors, but one of the more common types of adnexal carcinoma
Age
Most occur in elderly patients
Gender
Females have slightly higher incidence
Site
Eyelids are by far the most common site (˜ 75% of cases)
Remainder of cases occur in other head and neck sites, followed by trunk, extremities
Presentation
Nodular, firm, yellow-tan lesions
Often ulcerated
Treatment
Surgical approaches
Complete excision is necessary to ensure local removal
Mohs excision is reported to be effective in most cases
Sentinel lymph node biopsy may be useful for staging purposes
Prognosis
Aggressive tumors with high incidence of metastasis (> 30% of cases) and generally poor prognosis unless discovered early
MACROSCOPIC FEATURES
General Features
Dermal-based firm, nodular lesion
Size
Usually 1-4 cm
MICROSCOPIC PATHOLOGY
Histologic Features
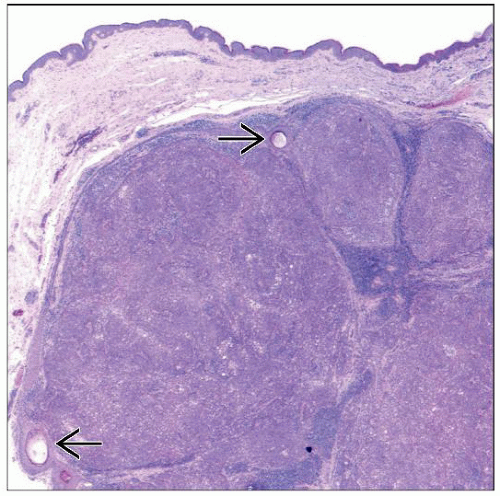
Dermal-based infiltrative, nodular to sheet-like tumor
Often with focal follicular &/or epidermal connections
Pagetoid involvement of epidermis may be seen in up to 30% of cases
Tumor consists of variably differentiated epithelioid cells
Clear cells often present but vary greatly in number
Well-differentiated tumors show prominent clear cell changes
Cells contain abundant cytoplasmic lipid, often producing multiple vacuoles and nuclear indentation
Nuclei are enlarged and vesicular or hyperchromatic-staining, with prominent nucleoli
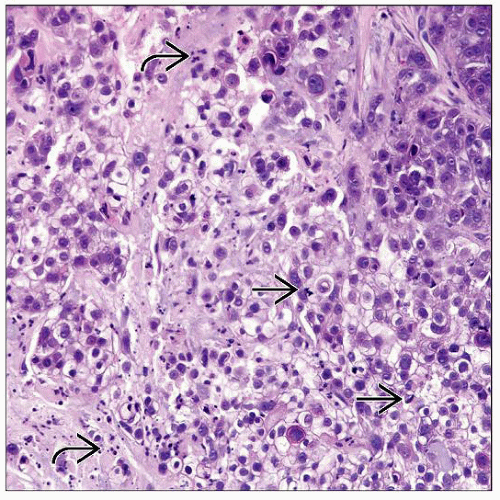
Moderately and poorly differentiated tumors show few to rare clear cells
May be composed predominantly of basaloid or squamoid cells
Show prominent cytologic atypia and pleomorphism
Mitotic figures, including atypical forms, are usually abundant
Areas of necrosis, with comedonecrosis pattern, are common
Lymphovascular invasion present in significant percentage of cases
Cytologic Features
Enlarged, epithelioid cells with abundant cytoplasm and hyperchromatic or vesicular nuclei with enlarged nucleoli
Clear cells usually show cytoplasmic vacuoles and nuclear indentation
However, cells can also be basaloid (common) or squamoid (rare)
ANCILLARY TESTS
Histochemistry
Sudan black B and oil red O (need frozen tissue)
Reactivity: Positive
Staining pattern
Cytoplasmic staining
Periodic acid-Schiff
Reactivity: Usually negative (indicating lack of glycogen)
Immunohistochemistry
EMA is positive in most well-differentiated cases, but is often negative in poorly differentiated tumors
EMA is negative in BCC, but often shows at least focal staining in SCC
EMA often highlights ductal structures in other adnexal carcinomas (i.e., porocarcinoma and hidradenocarcinoma), but not in sebaceous carcinoma
Androgen receptor (AR) is positive (nuclear staining) in most cases, including poorly differentiated carcinomas
SCC and most other primary cutaneous carcinomas are negative for AR
However, AR is often positive in BCC (> 60% of cases) and some metastatic carcinomas to the skin
HMWCKs (i.e., CK5/6 and CK903/34βE12) and p63 are typically strongly and diffusely positive
Help to exclude metastatic tumors (most of which are negative for both of these markers) but do not distinguish from other primary cutaneous tumors
D2-40 (podoplanin) is positive in a subset of cases, especially in more basaloid sebaceous carcinomas
Can also highlight areas of lymphovascular invasion
Other markers that may be positive include CAM5.2, BER-EP4, CK7 (˜ 50% of cases), and CD10 (˜ 50%)
Negative for CEA-M, CK20, GCDFP-15, RCA/PRNA, TTF-1, S100
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree