Right Hemicolectomy: Single-Incision Laparoscopic Technique
Theodoros Voloyiannis
DEFINITION
Single-incision laparoscopic right hemicolectomy is a refined technique of conventional laparoscopy where a single multichannel laparoscopic port is used via a 2.5- to 5-cm total incision length.
The goal is to keep the procedure simple, safe, and costeffective with comparable outcomes to hand-assisted or multiport laparoscopic technique.
Although single-incision laparoscopy differs from the conventional laparoscopy, it follows the same steps and oncologic principles. It can be completed without difficulty with an extracorporeal anastomosis. An intracorporeal anastomosis can be performed as well; however, it requires advanced laparoscopic skills and the addition of laparoscopic Endo GIA staplers.
DIFFERENTIAL DIAGNOSIS
The procedure can be performed for benign or neoplastic diseases or condition, including the following:
Appendectomy
Ileocecectomy
Formal right colectomy
Extended right colectomy
PATIENT HISTORY AND PHYSICAL FINDINGS
A detailed history and physical exam is essential preoperatively to determine if the patient is suitable for laparoscopic single-incision right hemicolectomy. Potential contraindications to laparoscopic single-incision right hemicolectomy are summarized in Table 1.
In case of underlying neoplasia, the size of the tumor determines if it can be extracted without tension via the single-port wound protector. In general, tumors up to 7 cm can be extracted via a 5-cm maximum length single incision. The procedure can still be performed with elongation of the incision for extraction of larger tumors. In that case, the benefit of the single port is eliminated, with the exception of the avoidance of use of multiple laparoscopic ports.
A large palpable tumor preoperatively with fixation to the abdominal wall or other organs may be a contraindication to single-incision laparoscopy, although excision en bloc with soft tissue abdominal wall is still possible via a single incision in some cases.
Signs and symptoms of obstructing neoplastic lesion with proximal distended right colon with or without competent ileocecal valve and small intestinal dilation may also suggest contraindication to laparoscopic approach due to difficulty establishing a safe working space with pneumoperitoneum. Anastomosis may be contraindicated in this case.
It is important to define the underlying pathology—benign versus malignant disease and the location of the lesion preoperatively. Ileocecectomy or right hemicolectomy for neoplasia may require formal lymphadenectomy with en bloc resection of the ileocolic vascular pedicle. Hepatic flexure or proximal transverse colon lesions may require additional resection of the right colic vein or right branch or the middle colic artery and vein and further mobilization of the proximal transverse colon.
Involvement of other organs or structures, such as right ovary, small intestine, abdominal wall, right ureter, right kidney, duodenum, small intestine, omentum, liver, and gallbladder, may require a hand-assisted laparoscopy or open laparotomy. Potential intraoperative consultation to other subspecialties may be required in these cases. It is the primary surgeons’ responsibility to communicate with the consulting service that a single-incision laparoscopic approach is planned.
Failure to identify the tumor extent preoperatively may lead to longer operative time if a single-port technique is used. Conversion to hand-assisted or open approach is prudent in these cases.
Presence of preoperative umbilical or other incisional hernia does not preclude a single-incision approach; however, it may require lengthier operative time, extension of the incision, and possibly placement of a xenograft.
Previous abdominal surgeries with extensive abdominal or pelvic adhesions may increase the operative time. A single incision may actually facilitate a faster abdominal adhesiolysis as it can partially be performed open via the port’s wound protector with assistance of a retractor.
Crohn’s terminal ileitis or right colitis with a large phlegmon or perforation with complex fistulae or abscess may preclude a single-incision laparoscopic approach.
Previous appendectomy is not a contraindication to singleincision laparoscopic right hemicolectomy, as adhesions may be the only intraoperative finding with minimal increase to operative time.
Table 1: Absolute Contraindications to Single-Incision Laparoscopic Right Colectomy | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
IMAGING AND OTHER DIAGNOSTIC STUDIES
Preoperative colonoscopy with India ink tattoo injection is of paramount importance for smaller nonpalpable benign or malignant lesions or polyps, which are not resectable endoscopically. The surgeon must clearly identify the site of the tattoo at 5 cm distal to the lesion preoperatively in the absence of other anatomic landmarks, such as the ileocecal valve or the appendiceal orifice and the cecum itself.
India ink tattoo by different gastroenterologists has been reported to be placed proximally around the lesion, distal to the lesion, or both proximal and distal to the lesion, leading occasionally to a false distal colonic resection margin.
Inadvertent extracolonic India ink injection may lead to inflammatory—diverticulitis type—reaction of the surrounding mesentery and omentum, thus making the single-incision laparoscopic colonic mobilization challenging. Absence of preoperative tattoo for smaller or nonpalpable lesions distal to the ileocecal valve may lead to failure to localize the lesion intraoperatively, lengthy procedure and possible need for intraoperative colonoscopy, and conversion to laparotomy. This may lead to significant air insufflation of the colon and small intestine unless a carbon dioxide (CO2) colonoscopic insufflation is available. Compressing the terminal ileum with a laparoscopic grasper during the intraoperative colonoscopy may prevent small intestinal distension.
Computed tomography of the abdomen and pelvis with oral and intravenous (IV) contrast helps determine the feasibility of a single-incision laparoscopic approach and identifies the exact location of larger right colonic neoplastic lesions, involvement of adjacent organs or structures, mesenteric adenopathy and possible metastatic lesions, hernia, and other abdominal nonrelated pathology. Inflammatory disease of the terminal ileum or right colon is suspected by the presence of phlegmon, abscess, fistula, or obstruction.
Magnetic resonance imaging (MRI) of the abdomen may assist with the identification of indeterminate liver lesions and with the assessment of metastatic lesions preoperatively. Positron emission tomography (PET) computed tomography is not generally needed preoperatively.
Preoperative barium enema or small bowel follow-through contrast study has generally been replaced by colonoscopy. Ultrasound (US) of the abdomen has limited usefulness for the identification of colonic pathology.
A carcinoembryonic antigen is obtained as baseline tumor marker for surveillance.
SURGICAL MANAGEMENT
Preoperative Planning
Full bowel preparation is administered the day prior to surgery. Right colectomy without bowel preparation is equally safe but it may increase the weight and volume of the right colon and impair the laparoscopic handling of the colon. Furthermore, extraction of the specimen via a small 3.5-cm single incision may become challenging.
Preoperative medical or pulmonary cardiac clearance as necessary.
Correction of preoperative anemia as needed.
IV antibiotics, venous thromboembolism (VTE) prophylaxis, µu-receptor antagonist (alvimopan) immediately preoperatively, correction of electrolyte abnormalities.
Instrumentation
A bariatric length, 10-mm 30-degree camera is used. Use a right-angle adaptor for fiberoptic attachment to the camera, if needed, to avoid conflict of the fiberoptic cord with other laparoscopic instruments. Use a preheated camera or other devices for camera lens cleansing. Repeated camera cleansing requires frequent removal via the single port, which adds time to the procedure.
Two bariatric length laparoscopic bowel graspers are used. Bariatric length laparoscopic energy device such as 43-cm LigaSure, 5 mm with monopolar tip, Enseal, or similar is used. Energy devices that produce excessive moisture/fog may impair the visibility as most single-incision laparoscopic ports have a side port for smoke evacuation at the same level with the channel for air insufflation.
Bariatric length laparoscopic 5-mm suction irrigation
Laparoscopic smoke evacuator channel
Laparoscopic scissors
Laparoscopic 5-mm or 10-mm clip applier (optional)
Laparoscopic Endoloop polydioxanone (PDS) for the ileocolic vascular pedicle
Staplers: linear gastrointestinal anastomosis (GIA) 75-mm, double, or preferably triple line, blue staple cartridges
Second set of instruments for extracorporeal anastomosis
Patient, Team, and Operating Room Setup
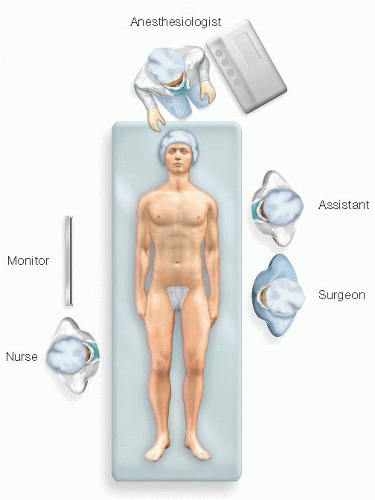
The patient is placed over a foam pad on supine position with the arms and legs tucked to the side and secured to the table with a Velcro safety strap or broad tape across the chest and lower extremities (FIG 1).
Sequential compression devices (SCDs) are applied to the lower extremities.
A laparoscopic operating room (OR) table with steep tilting is used. Test maximum tilting prior to draping to assess patients’ secure positioning on the table.
A Foley catheter is inserted and taped over the right thigh in order to avoid urethral trauma during patient positioning changes throughout the operation. A bear hugger or other thermal device is applied to the chest and legs.
Protecting foam pad is placed over the head to protect from injury with laparoscopic instruments.
The laparoscopic tower and energy devices are placed to the right of the patient’s head.
The surgeon stands to the patient’s left side with the assistant standing to his right side (FIG 2). The scrub nurse stands by the patient’s right leg. One or two high-definition monitors are placed to the patient’s right side at eye level in front of the surgeon.